 |
 |
| Korean J Anesthesiol > Volume 76(2); 2023 > Article |
|
The novel ŌĆ£anterior passageŌĆØ sub-longissimus-thoracis plane (SLoP) block for lumbar spine surgery, which is meant to target the SLoP from an anterior-lateral entry point, is proposed.
Herein, we describe three patients aged 71, 75, and 56 years who underwent uneventful surgeries for L5-S1, L5-S1, and L4-L5-S1 transforaminal lumbar interbody fusions, respectively, under general anesthesia. The patients had controlled hypertension and no other significant medical history. Despite the administration of considerable intravenous (IV) analgesia 30 min before the end of the surgery (tramadol 150 mg, paracetamol 1,000 mg, ketorolac 30 mg and morphine 4 mg), the patients had significant issues with pain control 30 min after surgery, as evidenced by numeric pain rating scale (NPRS) scores of 8/10, 9/10, and 7/10, respectively.
The patients gave written consent for the publication of their case reports.
All patients received 15 ml of ropivacaine 0.375% (Kabi-Fresenius, Portugal) bilaterally using a 12-cm 21 gauge needle (Echoplex®, Vygon, France) under low frequency ultrasound guidance (Acuson P300®, Siemens, Germany). No complications were observed, and the neurological evaluation was not affected. The patients reported rapid pain relief (NPRS scores dropped from 8/10 to 1/10, from 9/10 to 1/10, and from 7/10 to 0/10 for the patients aged 71, 75, and 56 years, respectively). Tramadol 100 mg IV every 8 h, paracetamol 1,000 mg IV every 8 h, and ketorolac IV every 8 h were prescribed. The NPRS score started increasing at 18, 16, and 24 h postoperatively, up to a maximum of 2/10, 3/10, and 3/10, respectively, during the hospital stay but no further rescue analgesia was needed. The two patients aged 71 and 75 years received the SLoP block type 1, and the remaining patient received the SLoP block type 2.
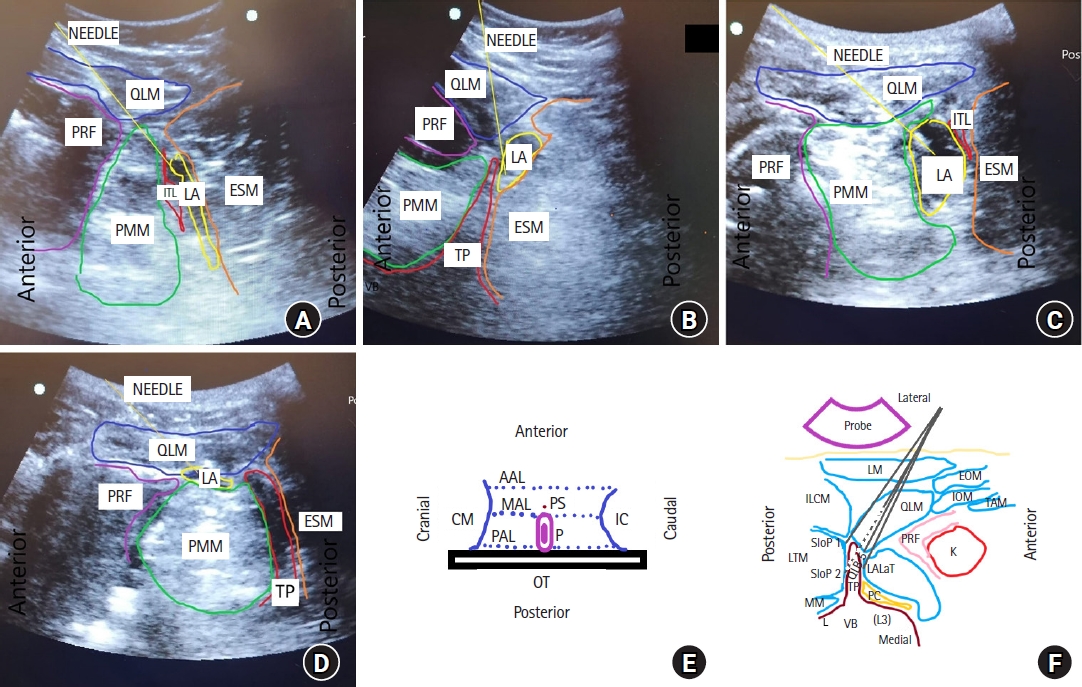
The SLoP block type 1 is shown in Fig. 1A. The curved probe (Acuson P300, Germany) is placed in the mid-axillary line transversally at the mid-point between the lower coastal margin and the iliac crest to identify the transverse process (TP) of L3. To perform the SLoP block type 1, the needle is advanced using the in-plane approach in an anterior-to-posterior direction through the latissimus dorsalis muscle, puncturing the skin 2ŌĆō3 cm posteriorly to the anterior axillary line at the L3 level, towards the plane between the psoas major muscle (PMM) and quadratus lumborum muscle [1,2]. The needle is then advanced further through the PMM to reach the TP/intertransverse ligament (ITL) [1]. Crossing the ITL, the SLoP can then be reached (if bony contact with the lateral TP is noted, the needle should be moved caudally or cranially, and then advanced to the SLoP). During injection, the local anesthetic (LA) can be observed dissecting the SLoP.
The SLoP block type 2 is shown in Fig. 1B. For this block, the needle can be passed laterally to the tip of the TP. The LA pushes the longissimus-thoracis muscle and spreads posteriorly to the TP in the SLoP (Fig. 1B).
The techniques used for lumbar spine surgery performed in the supine position through an anterior approach, namely, the LALaT block (Fig. 1C) [2] and the QLB type 5 (Fig. 1D)[1], and the form a triad that could be called the ŌĆ£anterior passage lumbarŌĆØ blocks (Figs. 1A-F). These blocks target injection site planes in close vicinity to each other but result in completely different dispersion patterns.
The anterior passage QLB type 5 shares the same injection site with the transmuscular QLB (T-QLB) [1], but the latter requires a posterior entry point. The LALaT block does not provide unnecessary analgesia to the abdomen as the lumbar plexus in the psoas compartment/paravertebral region is indirectly targeted (vertebral analgesia may, however, occur due to LA migration posteriorly toward the erector spinae plane [ESP]).
The anterior passage SLoP block, acting directly through the sub-ESP, should provide spinal analgesia that is at least comparable to other lumbar ESP techniques and potentially minimize the blockade of the anterior branches of the lumbar plexus [1].
The ESP block acts mostly on the posterior rami of the spinal nerves, which innervate the posterior components of the vertebrae; however, the postoperative neurologic evaluation may be affected due to some thoracic ŌĆ£ventralŌĆØ spread [2ŌĆō4]. In an MRI study, 30 ml of LA injected into the ESP at the T10 level was found to spread towards the ventral rami of the spinal nerves, even epidurally in some patients, which could affect the postoperative neurologic evaluation, increase the risk of falls, and interfere with the sympathetic block. At the lumbar level, ventral spread of the ESP block should be less common since the costotransverse foramina is not involved and the paravertebral space is not continual, although the previously described lumbar ESP block (and also the paraspinal fascial blocks) will impinge the surgical site [2,3].
In most patients with low thoracic ESP blocks, however, the LA was not found to spread caudally to L2. Therefore, even though this block does not interfere with the surgical site, it may fail to properly block the distal lumbar levels [4].
The longissimus-thoracis muscle has remarkable anatomy in this context. In the lumbar region, some of its fibers are attached to the entire length of the posterior surfaces of the TP, the accessory processes of the vertebrae, and the anterior layer of the lumbodorsal fascia. This means that it covers the lumbar vertebrae up to the articular pedicles (at the thoracic level, its medial insertions are located at the tips of the TP), which allows for the plane between the posterior vertebral components and the longissimus-thoracis muscle to be dissected from an anterior-lateral approach [5].
In conclusion, the SLoP block has an immense potential in the context of spinal surgery analgesia; it avoids impingement of the surgical site, is performed in the supine position and, results in limited LA epidural spread.
Fig.┬Ā1.
Description of the ŌĆ£anterior passageŌĆØ lumbar blocks: the sub-longissimus-thoracis plane (SLoP) block type 1 and type 2, lumbar anterior lateral transverse process (LALaT) block, and quadratus lumborum block (QLB) type 5. (A) Ultrasound image showing the novel ŌĆ£anterior passageŌĆØ SLoP block type 1. For this block, the transverse process (TP) is not observed during the injection because the ultrasound view targets the intertransverse region. A full description is available in the main text. (B) Ultrasound image showing an alternative approach to the novel ŌĆ£anterior passageŌĆØ SLoP block type 2. A full description is available in the main text. (C) Ultrasound image showing the ŌĆ£anterior passageŌĆØ LALaT block. The injection site is reached after the needle makes bony contact with the lateral portion of the TP, between the TP and the psoas major muscle (PMM) or, alternatively, between the intertransverse ligament (ITL) and the PMM. Relevant data about the technique (indications, procedure details, rationale) are available in the main text. (D) Ultrasound image showing the ŌĆ£anterior passageŌĆØ QLB type 5, the novel QLB 5. The injection point of the QLB 5 is between the PMM and the quadratus lumborum muscle (QLM), similar to the transmuscular QLB (T-QLB) but from an anterior entry point. Relevant data about the technique (indications, procedure details, and rationale) are available in the main text. (E) Schematic representation of the probe positioning and alignment for the blocks. The probe is positioned transversally. The needle is inserted in the middle axillary line (MAL), anterior to the probe, and directed towards the transverse process/intertransverse ligament in a medial/posterior direction. (F) Schematic representation of the relevant anatomy for these blocks. For these blocks, the curved probe is placed in the mid-axillary line with a transverse orientation, with the patient in a straight supine position. Movement of the ultrasound (US) probe towards the posterior axillary line (PAL) allows for the identification of the QLM. Once the L3 TP is visualized, posterior sliding of the probe should stop, as shown with the tip of the TP vertically oriented towards the skin in the ultrasound image. The QLM is visualized lying anteriorly and laterally to the most lateral portion of the TP and the tip of the TP. Medially (i.e., deeper in the US image), the PMM is visualized in contact with the TP and vertebral body. For all techniques, a shamrock sign is observed, in which the erector spinae muscle (ESM) is located posteriorly to the (TP), the QLM is located more superficially (laterally) and anteriorly to the TP, and the PMM is observed more deeply on the ultrasound image in front of the TP. The QLM functions as a safe method for needle tracking (the perirenal fat [PRF] should not be crossed). Additional descriptions are provided in the main text. SLoP 1: sub-longissimus plane block type 1 injection site, SLoP 2: sub-longissimus plane block type 2 injection site, VB: vertebral body, QLB 5: QLB type 5 injection site, K: kidney, PC: psoas compartment, LA: local anesthetic, AAL: anterior axillary line, CM: inferior chest wall margin, IC: iliac crest, LM: latissimus dorsalis muscle, TAM: transverse abdominis muscle, EOM: external oblique muscle, IOM: internal oblique muscle, LTM: longissimus thoracis muscle, MM: multifidus muscle, OT: operation table, P: probe.
References
1. Almeida CR, Cunha F, Pinto M, Gon├¦alves J, Cunha P, Antunes P. A lumbar anterior lateral transverse-process (LALaT) block for a patient with multiple traumatic injuries. J Clin Anesth 2021; 71: 110252.


2. Almeida CR, Oliveira AR, Cunha P. Continuous bilateral erector of spine plane block at T8 for extensive lumbar spine fusion surgery: case report. Pain Pract 2019; 19: 536-40.



3. Tulgar S, Ahiskalioglu A, De Cassai A, Gurkan Y. Efficacy of bilateral erector spinae plane block in the management of pain: current insights. J Pain Res 2019; 12: 2597-613.



4. Schwartzmann A, Peng P, Maciel MA, Alcarraz P, Gonzalez X, Forero M. A magnetic resonance imaging study of local anesthetic spread in patients receiving an erector spinae plane block. Can J Anaesth 2020; 67: 942-8.



5. Standring S, Gray H. GrayŌĆÖs anatomy: the anatomical basis of clinical practice. 20th ed. Edinburgh, Churchill Livingstone/Elsevier. 2018, pp 397-400.









