|
 |
|
|
Abstract
Hemoptysis requires proper treatment to prevent blood aspiration and asphyxiation. If the patient loses consciousness or is anesthetized, the bleeding inside the trachea may continuously flow into the distal part, which may be fatal. Fatal damage resulting from hemoptysis is mainly caused by asphyxiation, and it is important to find the exact location of the bleeding in order to prevent it from spreading to both lungs. However, endotracheal intubation may increase the bleeding by stimulating the bleeding lesion in the respiratory track, and can make airway management more difficult. We report a successful case of airway management using the cuff and Murphy eye of the endotracheal tube in a patient with tracheal bleeding.
Hemoptysis is mostly caused by small and vulnerable blood vessels in the mucous membrane [1]. The condition may cause fatal aspiration, and is therefore regarded as a medical emergency. For this reason, it is important to find the exact location of the bleeding and to treat it by maintaining an airway, endovascular embolization, or through surgical intervention [2,3]. When conscious, the patient can spit out the blood inside his or her trachea. However, if the patient loses consciousness or is anesthetized, the bleeding inside the trachea may continuously flow into the distal part, which may have fatal consequences from pulmonary aspiration. Moreover, endotracheal intubation may increase the bleeding by stimulating the bleeding lesion in the respiratory track, and can make airway management more difficult.
A 66-year-old male with a tracheal bleeding lesion was scheduled for a jejunostomy for enteral feeding. We used the expanded cuff of the endotracheal tube to block the tracheal bleeding from entering the bronchi, and placed the Murphy eye and tip of the endotracheal tube in the proper position to guarantee ventilation of both lungs. We report a successful case of airway management using the cuff and Murphy eye of the endotracheal tube in a patient with tracheal bleeding.
A 66-year-old male patient of 169 cm and 44 kg underwent a jejunostomy for enteral feeding. The patient was undergoing chemotherapy following an esophagogastrostomy for esophageal cancer, and was hospitalized for hemoptysis. Esophageal stent placement for enteral feeding had been attempted with a gastrofiberscope but had failed, causing retention in the stomach. Subsequently, the department of general surgery had performed elective surgery.
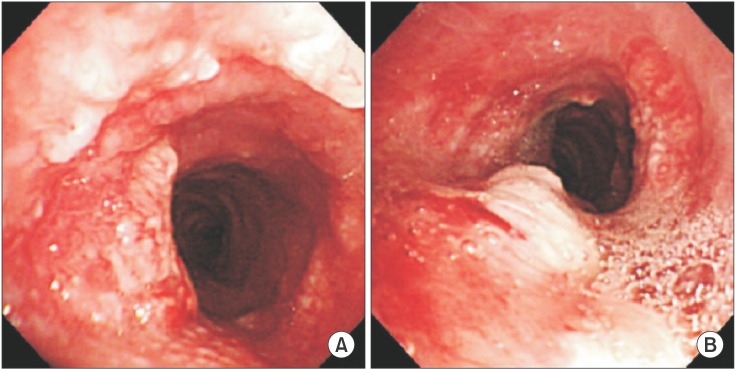
Hemoptysis with an amount of 400 ml a day had appeared a couple of days prior, and a nodular degeneration and flare were observed on the mucous membrane, 4 cm above the carina from the subglottic region, on the bronchofiberscopy performed 2 days before the surgery. Although no active bleeding was observed, petechial bleeding was evidenced, and it was assumed that this was where the hemoptysis had originated (Fig. 1). The biopsy results confirmed the presence of squamous cell carcinoma. A consultation was conducted by the otolaryngologist regarding preoperative bleeding treatment. However, due to the large lesion causing the petechial bleeding around the trachea, preoperative otorhinolaryngological bleeding treatment was not performed.
The preoperative chest X-ray showed an ill-defined infiltration in both lungs, with other laboratory results within the normal range. The arterial gas analysis read pH 7.42, PCO2 31.3 mmHg, PO2 82.9 mmHg, and BE -3.5 mM at FIO2 0.3. The patient was monitored using an electrocardiogram, noninvasive blood pressure measurement, and pulse oxymetry and bispectral index. The systemic blood pressure, heart rate, and arterial oxygen saturation before the anesthesia induction were 145/65 mmHg, 65 beats/min, and 96%, respectively.
General anesthesia was induced with propofol, remifentanil, and rocuronium. A fiberoptic bronchoscopic device was inserted in the trachea for pre-investigation before the endotracheal intubation. Differing from the results of the previous examination, a newly-developed nodular degeneration was observed from the subglottic region to the carina, and continuous petechial bleeding was also evidenced. Endotracheal intubation using a single lumen tube of 6.0 mm, Mallinckrodt Hi-LoŌäó, Mallinckrodt Medical Athlone, Ireland, was performed with guidance from the fiberoptic bronchoscopy.
While the patient could spit out the blood from the trachea while awake, there was a high risk that the blood would flow into both lung fields during the anesthesia as a result of muscular paralysis and loss of the coughing reflex. Therefore, it was necessary to prevent the blood from the lesion from flowing into the distal part during the anesthesia. We aimed to target the distal part with the ordinary endotracheal tube as much as possible. The tip of the endotracheal tube was placed towards the right main bronchus, while the Murphy eye faced the left main bronchus exactly, and the cuff was then expanded to compress the bleeding lesion and to prevent blood aspiration (Fig. 2).
No blood aspiration was observed in either bronchus from the fiberoptic bronchoscopy and the fiberoptic examinations performed every 30 minutes during the operation. It was also confirmed from the fiberoptic bronchoscopy that the tip of the endotracheal tube and the Murphy eye had been properly placed in the two main bronchi without altering the position of the endotracheal tube. There were no problems with the ventilation of either lung. Fortunately, the amount of petechial bleeding was small, and it could be removed with intermittent suction.
The operation was then carried out for 2 hours, after which it was confirmed from the acceleromyography (TOF-Watch SX®, Organon Ireland Ltd, Dublin, Ireland) used to assess the complete recovery of the muscle relaxation that the train of four (TOF) ratio was above 0.9, and the tube was removed after checking that the patient had recovered consciousness and opened his eyes.
After the operation, the patient was transferred to the ICU and his blood pressure and heart rate were measured at 170/90 mmHg and 70 times/min, respectively. The arterial oxygen saturation was measured at FIO2 0.35 through the Venturi mask, with a spontaneous respiration and respiratory rate of 97% and 16 times/min, respectively. The patient spit out about 40 cc of blood through coughing and was kept in the ICU for 2 days after the operation. The bleeding amount was about 300 cc per day, which did not represent a big increase from the pre-operation level. The chest X-ray showed normal findings and the patient was transferred to the general ward two days after the surgery.
It is important to find the exact location of the bleeding in patients with upper airway bleeding. The bleeding inside the trachea may continuously flow into the distal part if the patient loses consciousness or is anesthetized, and it has been reported that positive pressure ventilation can have fatal consequences from endotracheal aspiration.
In this case, the patient with the bleeding lesion was required to undergo endotracheal intubation for 2 hours as part of a scheduled general anesthesia. However, because the mechanical erosion and the ulceration caused by the endotracheal tube led to airway injuries [4,5], there was a risk that the endotracheal intubation would increase the bleeding by damaging the bleeding lesion in the airway. The authors sought to prevent the bleeding in the trachea from flowing into the main bronchi on both sides. To this end, the ordinary endotracheal tube was placed in the distal part as much as possible so as to insert the endotracheal tube while maintaining ventilation in both lungs, and the cuff was expanded in order to stop the endotracheal bleeding from flowing into the bronchi.
However, the distal part of the cuff can move into one of the main bronchi if the endotracheal tube is too deep and the cuff of the endotracheal tube is located on the carina, causing endobronchial intubation. Accidental endobronchial intubation has been found to occur in 3.7% of cases and if it happens, atelectasis in the lung without ventilation may cause hypoxia, while the overexpansion of the lung receiving ventilation may cause barotrauma and pneumothorax [6]. Prompt correction of the inappropriate positioning of the endotracheal tube through use of a fiberoptic bronchoscopy was reported to be effective in preventing further misplacement of the tube [7]. Therefore, the authors set up a ventilation strategy using the Murphy eye in order to ensure ventilation of both lungs while placing the endotracheal tube in the farthest distal part under guidance from the fiberoptic bronchoscopy.
Devised by Murphy in 1941, the Murphy eye is a hole on the side of the distal part of the endotracheal tube, which was designed to prevent the complete obstruction of ventilation when the tip of the endotracheal tube was blocked from touching the tracheal wall or clogged by tracheal excretions or lumps [8].
The authors used the Murphy eye as a means to achieve ventilation of the lung on one side. The endotracheal tube was positioned as closely to the carina as possible by placing the end hole of the endotracheal tube and the Murphy eye towards the right and left main bronchi after moving the endotracheal tube forward towards the carina under guidance from the fiberoptic bronchoscopy.
Another method we considered before establishing this ventilation strategy was to maintain lung ventilation by cutting the distal part of the cuff in the endotracheal tube. As there is only one end hole, the disadvantage of this method is that the ventilation may be completely obstructed if the tip of the endotracheal tube touches the tracheal wall or is clogged by a tracheal excretion, bleeding, or lump [9,10]. However, the method presents an advantage in that it may prevent improper ventilation through the Murphy eye occurring during the operation from a change in the direction or depth of the Murphy eye and placement of the endotracheal tube in the farther distal part with a distance large enough to cut the cuff and the Murphy eye. Furthermore, the endotracheal tip can be more easily located than in the ventilation method using the Murphy eye. Because of these merits, cutting the distal part of the cuff in the endotracheal tube represents a good alternative method.
The authors continuously checked that the delivered tidal volume was similar to that of the ventilator settings during the operation. If the delivered tidal volume was not equal to that of the ventilator settings and a greatly increased airway pressure as in endobronchial intubation was detected, even distribution of the tidal volume could not be assumed. In this case, the appropriate tidal volume and a peak inspiratory airway pressure in the normal range (17 to 20 cmH2O) were identified. In addition, the evenly auscultated sound of both lungs indirectly suggested that the tidal volume was evenly distributed.
A double-lumen tube may also be used for separate ventilation. Although the relative risk of a rare and severe complication such as tracheal rupture arising from the use of a doublelumen tube or a single-lumen tube is similar [5], the possibility of increasing the bleeding by stimulating the bleeding lesion in the respiratory track during the intubation or extubation from the large external diameter of the tube cannot be ignored. For this reason, the authors adopted a ventilation strategy using the Murphy eye of the endotracheal tube for airway management.
It is important to prevent the blood from flowing into the distal part in order to avoid blood aspiration in patients with continuous tracheal bleeding lesions. In these cases, it is ideal to place the cuff of the endotracheal tube in the distal part more than towards the lesions, or in the farthest distal part while enabling ventilation of both lungs. For this purpose, it may be a good alternative to use the Murphy eye for ventilation of both lungs by placing the endotracheal tube in the proper position under guidance from the fiberoptic bronchoscopy.
References
1. Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson L, Loscalzo S. Harrision's principles of internal medicine. 18th ed. New York, McGraw-Hill. 2011, pp 597-602.
2. Johnson JL. Manifestations of hemoptysis. How to manage minor, moderate, and massive bleeding. Postgrad Med 2002; 112: 101-106. 108-109. 113PMID: 12400152.

3. Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del Ciello A, Calandriello L, et al. Diagnosis and management of hemoptysis. Diagn Interv Radiol (Ank) 2014; 20: 299-309.

4. Pacheco-Lopez PC, Berkow LC, Hillel AT, Akst LM. Complications of airway management. Respir Care 2014; 59: 1006-1019. PMID: 24891204.


5. Mi├▒ambres E, Bur├│n J, Ballesteros MA, Llorca J, Mu├▒oz P, Gonz├Īlez-Castro A. Tracheal rupture after endotracheal intubation: a literature systematic review. Eur J Cardiothorac Surg 2009; 35: 1056-1062. PMID: 19369087.



6. McCoy EP, Russell WJ, Webb RK. Accidental bronchial intubation. An analysis of AIMS incident reports from 1988 to 1994 inclusive. Anaesthesia 1997; 52: 24-31. PMID: 9014541.


7. Rigini N, Boaz M, Ezri T, Evron S, Trigub D, Jackobashvilli S, et al. Prompt correction of endotracheal tube positioning after intubation prevents further inappropriate positions. J Clin Anesth 2011; 23: 367-371. PMID: 21641785.


8. Sugiyama K, Yokoyama K, Satoh K, Nishihara M, Yoshitomi T. Does the Murphy eye reduce the reliability of chest auscultation in detecting endobronchial intubation? Anesth Analg 1999; 88: 1380-1383. PMID: 10357348.


9. Tamakawa S. Every endotracheal tube needs a Murphy eye! Can J Anaesth 1999; 46: 998-999. PMID: 10522595.

- TOOLS