|
 |
|
|
We report a suspected case of malignant hyperthermia (MH) during sevoflurane anesthesia which was treated with dantrolene ingestion via nasogastric tube. We obtained a written, informed consent from the patient about using the information of the patient.
A 19-yr-old male patient, 75 kg, ASA class I, was scheduled for orbit reconstruction. The patient's medical history and laboratory findings were unremarkable. There was no familial history of MH, neuromuscular disorder.
After applying standard monitoring, anesthesia was induced with fentanyl, lidocaine, propofol, and rocuronium. After tracheal intubation, anesthesia was maintained with oxygen, medical air, sevoflurane, and rocuronium. Baseline data included the following: arterial blood pressure (BP) 120/80 mmHg, heart rate (HR) 90 beats per minute (bpm), SpO2 100%, axillary temperature 35.1℃. The vital signs were stable during the surgery.
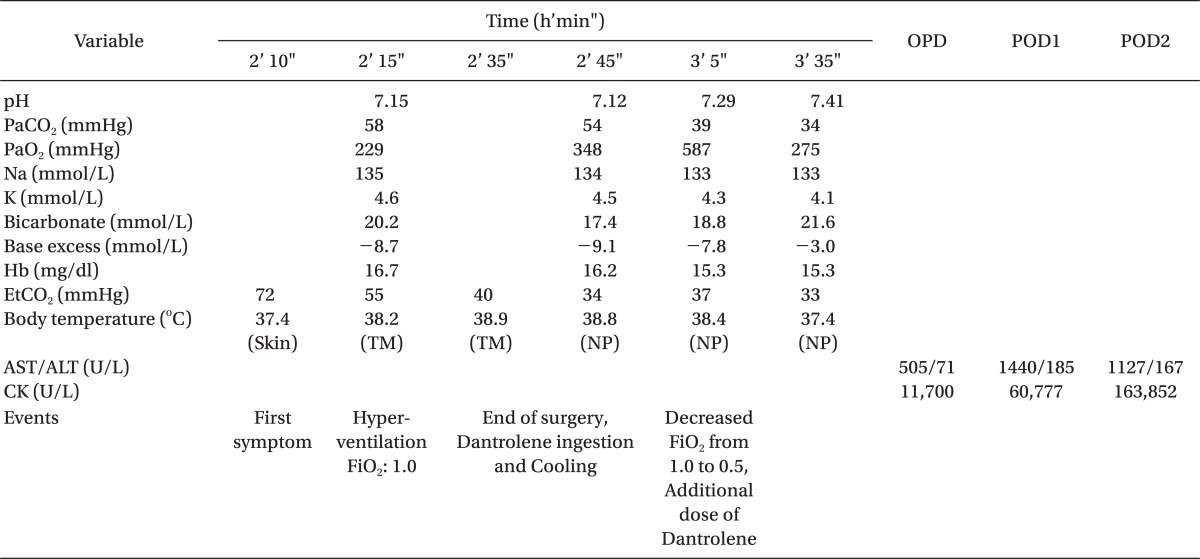
Approximately two hours after the induction of anesthesia, the surgery was expected to end within 30 minutes, and sevoflurane was changed to desflurane in order to facilitate recovery. After 10 minutes, end tidal CO2 (EtCO2) suddenly began to increase from 37 to 72 mmHg, and vital signs were also changed (axillary temperature; 36.1℃ to 37.4℃, BP; 130/70 mmHg to 160/100 mmHg, HR; 80 bpm to 155 bpm). Desflurane was discontinued, 100% oxygen (flow rate 10 L/min) was given, corrugate circuit and CO2 canister were changed, and the ventilatory rate was doubled. Midazolam 5 mg was intravenously injected, and propofol infusion was started. An arterial catheter was inserted, and arterial blood gas analysis (ABGA) showed the followings: pH 7.15, PaCO2 58 mmHg, PaO2 229 mmHg, base excess -9.6 mmol/L (Table 1). The surgery was completed at 2 hours and 35 minutes after the induction of anesthesia. After completion of surgery, a Foley catheter and nasogastric tube were inserted, and the body temperature (BT) of tympanic membrane was 38.4℃. Therapy for MH was initiated and included external cooling with cooling pad, cold intravenous (IV) fluids, forced diuresis, and bladder irrigation with cold saline. Since we did not have IV dantrolene, we tried to contact the hospital that stored dantrolene for the hospitals in our province, but they did not have any available dantrolene. Since there was no other choice, we created a dantrolene suspension by mixing 12 dantrolene capsules for oral medication (4 mg/kg, total 300 mg) in 50 ml of warm sterile water and injected it via nasogastric tube 5 minutes after the end of surgery. After 30 minutes, another dose of dantrolene suspension 100 mg was injected. Thirty minutes after the first dose of dantrolene ingestion, the patient's condition was gradually stabilized: EtCO2 34 mmHg, BT 37.4℃, BP 130/80 mmHg, and heart rate 94 bpm. ABGA was normalized (Table 1). One hour after the last dose of dantrolene, we confirmed the patient's condition as stable and stopped propofol infusion. The patient recovered from general anesthesia and transferred to the intensive care unit (ICU) after extubation. One hour after ICU admission, BT elevated to 38.2℃ again and cooling was continued with additional dantrolene ingestion (50 mg). Seven hours after ICU admission, BT was 37.1℃ and did not elevated again. The patient showed red colored urine and complained of generalized myalgia. Forced diuresis was continued from operation day to POD2 with hydration, furosemide, and mannitol infusion (urine output was about 300 ml/hr from Operation day to POD1). Urine color was normalized on POD2. The patient showed an increased aspartate aminotransferase, alanine aminotransferase and serum creatinine kinase (CK) level (Table 1) due to muscular destruction. Postoperative serum K+, PT, and aPTT was within normal limit (K+; 4.0, PT; 11.8 sec, INR; 0.98, aPTT; 25.9 sec). Dantrolene 100 mg, three times a day, was continued for 3 days. On POD2, the patient was transferred to the general ward and discharged on POD 11.
The patient's score of clinical indicators of MH was 63, and we could assume this patient had MH-susceptible [1]. The patient refused DNA analysis and muscle biopsy.
The best way to treat an MH crisis is early intravenous administration of dantrolene. The recommendation is that at least 36 bottles of dantrolene be available immediately in every hospital [2]. But in our country, only one base hospital has 6 vials of dantrolene in each province because of its high cost and the rare incidence of MH (in South Korea, we had only 39 vials of dantrolene in August 2011). Unfortunately, there was another case of MH in our province just before our case, and there was no remaining dantrolene for this patient. We tried to contact Korea Orphan Drug center, and they arranged us to contact the base Hospital of Seoul (two hours by car from our hospital). The manager of dantrolene in the Hospital informed us they have only three vials of dantrolene. At this time, the patient's condition began to stabilize, so we did not consider intravenous dantrolene.
Dantrolene sodium is well absorbed, with peak blood levels 3 to 6 hours after ingestion [3]. Allen et al. [4] reported that an acceptable plasma level of dantrolene can be achieved by oral dantrolene 5 mg/kg divided 3-4 times a day. In our case, 30 minutes after 4 mg/kg of dantrolene ingestion (four times of IV dose), the patient began to recover and additional doses were given, too. But BT elevated again one hour after ICU admission and gradually decreased. Thus, it is thought that oral dantrolene was effective about 3 hours after ingestion. Nagase et al. [5] reported similar case. Their patient's heart rate was decreased soon after the dantrolene ingestion via nasogastric tube, but BT was still high until peritoneal lavage with ice cold saline.
The standard therapy for MH crisis is administering intravenous dantrolene as soon as possible, but if it is not available, oral route dantrolene therapy maybe 'plan B'. Also, oral dantrolene capsule is cheap and easy to prescribe.
In conclusion, we experienced an MH case that was treated with dantrolene ingestion via nasogastric tube. Oral dantrolene ingestion via nasogastric tube may be another option of MH treatment, but the effect is limited because of its delayed onset.
References
1. Larach MG, Localio AR, Allen GC, Denborough MA, Ellis FR, Gronert GA, et al. A clinical grading scale to predict malignant hyperthermia susceptibility. Anesthesiology 1994; 80: 771-779. PMID: 8024130.


2. Chartrand D. Rapid intervention for an episode of malignant hyperthermia. Can J Anaesth 2003; 50: 104-107. PMID: 12560297.


3. Krach LE. Pharmacotherapy of spasticity: oral medications and intrathecal baclofen. J Child Neurol 2001; 16: 31-36. PMID: 11225954.


4. Allen GC, Cattran CB, Peterson RG, Lalande M. Plasma levels of dantrolene following oral administration in malignant hyperthermia-susceptible patients. Anesthesiology 1988; 69: 900-904. PMID: 3057938.


5. Nagase M, Naganuma Y, Ryo K, Sato N, Kawashima Y. Treatment of malignant hyperthermia by dantrolene sodium administered through a nasogastric tube. Masui 1984; 33: 1021-1026. PMID: 6512969.

- TOOLS