|
 |
|
|
Abstract
Background
In an era of medical cost containment, cost-effectiveness has become a major focus in healthcare. The effect of a new policy on the use of low fresh gas flow during maintenance of general anesthesia with volatile anesthetics was evaluated.
Methods
The numbers and duration of general anesthesia cases using sevoflurane 5 weeks prior to and 15 weeks after policy implementation were retrieved from the electronic medical records database. The number of sevoflurane bottles consumed was also assessed. The anesthesia hours per bottle of sevoflurane were compared before and after policy implementation.
Medical expenditure has been rising continuously in recent years due to an increased incidence of major illnesses such as cardiovascular diseases and cancer, frequent use of expensive medical devices, increased interest in quality of life, and the aging population. Medical cost containment has gained interest not only at the national level but also at the hospital level [1].
One area of potential cost reduction in the field of anesthesia involves the use of volatile anesthetics. Many anesthesiologists use a fresh gas flow rate of 2-3 L/min during maintenance of anesthesia. However, considering the low blood-gas coefficients of current volatile anesthetics and the advances in patient monitoring during anesthesia such as volatile anesthetic concentration monitoring, the use of low-flow anesthesia is a viable option in terms of reducing the consumption of volatile anesthetics [2-4]. In addition, the danger of compound A accumulation and its toxicity with the use of sevoflurane during low-flow anesthesia has been shown to be unfounded in humans [5-8].
Our department made it a policy to maintain anesthesia with a fresh gas flow of 1 L or less during anesthesia when using volatile anesthetics. We performed this observational study to evaluate the effect of low fresh gas flow on volatile anesthetic consumption.
The study was approved by the institutional review board. Currently, 12 operating rooms are in use and perform 25-35 surgical cases per day which require general anesthesia. The surgical procedures performed include orthopedic, urologic, thoracic, cardiac, neurosurgical, ophthalmic, gynecologic, otolaryngologic, dental, and general surgical procedures.
Beginning on the second week of March, a new policy concerning fresh gas flow rate during maintenance of general anesthesia using volatile anesthetics came in to effect. The policy stated that when maintaining anesthesia using volatile anesthetics, the fresh gas flow rate should be less than or equal to 1 L per minute. The combination and ratio of gases used were at the discretion of each anesthesia caregiver. The policy also stated that the fresh gas flow rate should be increased to 2-3 L per minute for 5 minutes when a change in volatile anesthetic concentration was required and subsequently reset to less than 1 L per minute. The policy did not contain any directions regarding fresh gas flow rate during induction. All anesthesia caregivers working in the operating room were informed of the new policy and were periodically reminded by supervising faculty.
Since sevoflurane accounted for more than 90% of the volatile anesthetics used in our hospital, the amount of sevoflurane consumed was recorded on a weekly basis. The number of cases that used sevoflurane for general anesthesia as well as the duration of anesthesia were also retrieved from the electronic medical record system. The number of general anesthesia hours performed per bottle of sevoflurane (250 ml) was calculated by dividing the total duration (hours) of general anesthesia using sevoflurane per week by the number of sevoflurane bottles consumed. The number of sevoflurane bottles consumed was calculated by checking the weekly inventory. A period of 5 weeks prior to the implementation of the new policy was compared with the subsequent 15 weeks.
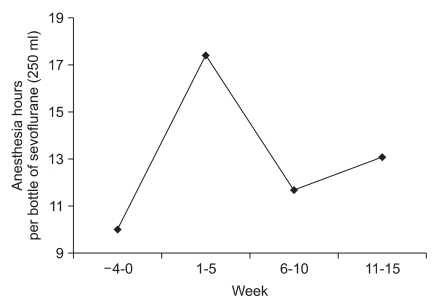
The number of surgical cases performed under general anesthesia using volatile anesthetics and the total anesthesia time during the study period are summarized in Table 1. The number of anesthesia hours per bottle of sevoflurane was 10.0 hours per bottle before the implementation of the low fresh gas flow policy (Fig. 1). In the first 5 weeks after policy implementation, anesthesia hours per bottle of sevoflurane increased by 73.7% (17.4 hours per bottle). In the following two consecutive 5-week periods, anesthesia hours per bottle of sevoflurane increased by 16.5% and 30.1%, respectively (Fig. 1). During the 15 weeks after policy implementation, the anesthesia hours per bottle of sevoflurane increased by 38.3% (13.9 hours per bottle).
The number and duration of surgical cases were comparable throughout the study period (Table 1). There were no reports of renal failure during the study period among patients who underwent surgery and anesthesia with sevoflurane.
Our study results show that by implementing a low fresh gas flow rate policy during maintenance of general anesthesia using volatile anesthetics, the consumption of volatile anesthetics can be reduced substantially. This also implies that anesthesia resources can be used more efficiently by maximizing their utility.
Hospital costs can be divided into fixed costs and variable costs. The healthcare industry is famous for its high proportion of fixed costs [1]. Therefore, the financial status of a hospital is highly dependent on the volume of patients. But this is not to say that reduction in variable costs is meaningless, especially considering the high prices of resources required in healthcare. The operating room and the practice of anesthesia in some ways are even more biased towards fixed costs. The high costs of building and maintaining the operating theater, personnel, and various devices are the main factors. However, there are still a significant proportion of variable costs that incur with each surgical case that requires general anesthesia. Volatile anesthetics are one of the major items in this regard [9-11].
The consumption of volatile anesthetics during general anesthesia mainly depends on two factors. The set volume percent of the volatile anesthetic on the vaporizer and the fresh gas flow rate. Throughout each surgical case, the depth of anesthesia required is met by increasing and decreasing the volume percentage of volatile anesthetics. Therefore, regulating the volume percentage of the volatile anesthetic is impractical and even unethical in terms of cost reduction. However, using a lower fresh gas flow rate not only has a direct proportional effect on the consumption of volatile anesthetics, but has been shown to be safe and effective in several different settings [12,13].
There are some limitations to this study. First, the effect of the policy seems to be inconsistent and fading over time. As with all policies, persistent education and advocacy of the low fresh gas flow are required to maintain the effect. Acceptance and use of the policy by each anesthesia caregiver may also be a factor, since the residents of our department rotate through a number of affiliated hospitals on a monthly basis. Second, data were gathered only for cases using sevoflurane and therefore caution is required when extrapolating to other volatile anesthetics. As mentioned, most of our general anesthetic cases are performed with sevoflurane. We generated data for desflurane as well with similar results. However, due to the small number of cases, they were excluded since this dataset was more vulnerable to bias.
In conclusion, the low fresh gas flow rate policy during maintenance of general anesthesia using sevoflurane reduced the amount of sevoflurane consumption by nearly 40%. Adoption of similar policies with other volatile anesthetics and in other institutions may help improve the cost-effectiveness of volatile anesthetics.
References
1. Roberts RR, Frutos PW, Ciavarella GG, Gussow LM, Mensah EK, Kampe LM, et al. Distribution of variable vs fixed costs of hospital care. JAMA 1999; 281: 644-649. PMID: 10029127.


2. Ekbom K, Assareh H, Anderson RE, Jakobsson JG. The effects of fresh gas flow on the amount of sevoflurane vaporized during 1 minimum alveolar concentration anaesthesia for day surgery: a clinical study. Acta Anaesthesiol Scand 2007; 51: 290-293. PMID: 17250746.


3. Cotter SM, Petros AJ, Doré CJ, Barber ND, White DC. Low-flow anaesthesia. Practice, cost implications and acceptability. Anaesthesia 1991; 46: 1009-1012. PMID: 1781522.


4. Baxter AD. Low and minimal flow inhalational anaesthesia. Can J Anaesth 1997; 44: 643-652. quiz 652-3. PMID: 9187785.


5. Obata R, Bito H, Ohmura M, Moriwaki G, Ikeuchi Y, Katoh T, et al. The effects of prolonged low-flow sevoflurane anesthesia on renal and hepatic function. Anesth Analg 2000; 91: 1262-1268. PMID: 11049919.


6. Kharasch ED, Frink EJ Jr, Artru A, Michalowski P, Rooke GA, Nogami W. Long-duration low-flow sevoflurane and isoflurane effects on postoperative renal and hepatic function. Anesth Analg 2001; 93: 1511-1520. PMID: 11726433.


7. Conzen PF, Kharasch ED, Czerner SF, Artru AA, Reichle FM, Michalowski P, et al. Low-flow sevoflurane compared with low-flow isoflurane anesthesia in patients with stable renal insufficiency. Anesthesiology 2002; 97: 578-584. PMID: 12218523.


8. Choi SR, Cho WJ, Chin YJ, Chung CJ. The effects of prolonged minimal-flow sevoflurane anesthesia on postoperative hepatic and renal function. Korean J Anesthesiol 2008; 54: 501-506.

9. Odin I, Feiss P. Low flow and economics of inhalational anaesthesia. Best Pract Res Clin Anaesthesiol 2005; 19: 399-413. PMID: 16013690.


10. Suttner S, Boldt J. Low-flow anaesthesia. Does it have potential pharmacoeconomic consequences? Pharmacoeconomics 2000; 17: 585-590. PMID: 10977395.


11. Watcha MF, White PF. Economics of anesthetic practice. Anesthesiology 1997; 86: 1170-1196. PMID: 9158367.


12. Baum JA, Aitkenhead AR. Low-flow anaesthesia. Anaesthesia 1995; 50(Suppl): 37-44. PMID: 7485917.

13. Ebert TJ, Arain SR. Renal responses to low-flow desflurane, sevoflurane, and propofol in patients. Anesthesiology 2000; 93: 1401-1406. PMID: 11149433.


- TOOLS