|
 |
|
|
Abstract
Intubating patients with a huge, fixed supraglottic mass causing an obstruction of the glottis is difficult to most anesthesiologists. We attempted awake fiberoptic orotracheal intubation assisted by Glidescope® Videolaryngoscope (GVL) following topical anesthesia with 4% lidocaine spray and remifentanil infusion. The glottis could not be identified by the GVL view. However, by entering toward the right side of the mass with bronchoscope, the glottis was found. Due to stiffness of the mass, we were unable to further enter the area using the bronchoscope. Alternatively, we attempted to expose the glottis by GVL blade and then successfully intubated the patient by manually pressing the cricoids cartilage. GVL is nonetheless an excellent instrument in airway management compared to fiberoptic bronchoscope for patients with a huge and fixed supraglottic mass.
Serious problems can arise during the induction of general anesthesia in patients with a supraglottic mass due to airway obstruction. For these patients, a preoperative test and an assessment by an anesthesiologist are necessary, and various types of equipment and methods should be planned in order to secure the airway during each step of the procedure [1]. A method using a flexible bronchoscope is recommended for patients with a supraglottic mass in which airway management is expected to be difficult. However, the opening and closing of the vocal cord is not observed when the patient breathes, and intubation is difficult due to the short distance and the narrow vision when approaching the oral cavity. In addition, intubation using a flexible bronchoscope is also limited in the event of hemorrhaging or when considerable amounts of secretions such as sputum are present. One report recommended airway management using a Macintosh laryngoscope to offset the difficulty of using a flexible bronchoscope in such patients [2]. Recent developments in videolaryngoscope development have shown great advancements in the field of endotracheal intubation in the last a few years. Among the developed videolaryngoscopes, the Glidescope® videolaryngoscope (GVL) provides better access to the glottis compared to the conventional Macintosh laryngoscope, requires less power when using it, and presents an anatomical structure as observed by the operator that is also simultaneously observable by other medical staff members. This can increase the success ratio of endotracheal intubation [3]. We experienced a successful awake orotracheal intubation in a patient with a very large tumor fixed at the top of the glottis using the GVL with the help of a flexible bronchoscope. This case is reported here with a related literature survey.
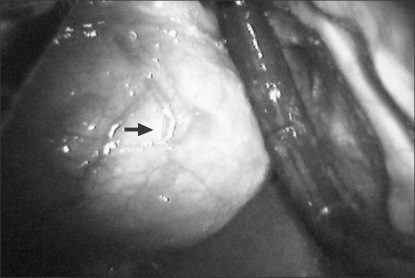
A 158 cm, 40 kg, 26-year-old female patient visited the hospital complaining of hoarseness and intermittent respiratory distress. It was found in a bronchial endoscope examination through the nasal cavity that an elliptic tumor mass about 4 cm in diameter was blocking almost all of the top part of the glottis. The computed tomography (CT) showed that the tumor mass may have originated from the left aryepiglottic fold. The boundary between the tumor mass and other surrounding parts was relatively well distinguished, and the round tumor mass caused the laryngeal cartilaginous structure to deviate to the right (Fig. 1). No abnormality was found in a preoperative blood test, electrocardiography (EKG) and chest PA image. There was no specific finding in the family and personal history. In tests related to the airway, the mouth opening and neck extension were normal, and the Mallampati score was 3. Initially, we decided to carry out awake orotracheal intubation using the GVL and a flexible bronchoscope. Considerations were given to the patient's demand to avoid a tracheostomy if possible, taking her young age into account, as well as her discomfort with the intubation through her nasal cavity during the bronchoscopy test.
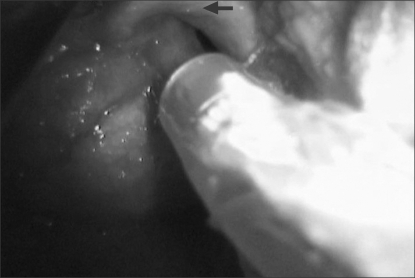
As premedication, midazolam 2 mg and glycopyrrolate 0.2 mg were injected intramuscularly. When arriving at the operation room, her blood pressure was 110/70 mmHg, her heart rate was 80 beats/min and her peripheral arterial oxygen saturation (SpO2) was 97%. The ENT department prepared for an emergency tracheostomy because there was a high probability of airway obstruction during the induction process. 4% lidocaine was sufficiently sprayed onto the backside of the tongue, the soft palate, the pharynx and the larynx in the oral cavity using the GVL. Subsequently, 0.75 µg/kg of remifentanil was injected intravenously, and the injection was continued at a rate of 0.075 µg/kg/min. Oxygen was supplied through an oxygen mask at a rate of 5 L/min. An assistant exposed the tumor mass at the top of the glottis when the GVL blade was introduced into the oral cavity. Another operator inserted an endotracheal tube with an inner diameter of 7.0 mm at the right of the GVL blade and introduced the tip of a flexible bronchoscope, of which the outer diameter was 5.2 mm. However, only a part of the glottis was shown due to the solid tumor mass, and the deviated laryngeal cartilaginous structure and the bronchoscope tip could not proceed. Although attempts were made to move the bronchoscope tip forward several times while varying the moving direction, the introduction of the bronchoscope was halted for fear of the risk of hemorrhage and damage to the vocal cords. Subsequently, the solid tumor mass was pushed to the left using the GVL tip at the entrance of the vocal cord, and the patient's cricoid cartilage was pushed to the left posterosuperior direction by an assistant. A part of the vocal cord could then be seen. Endotracheal intubation was successfully performed using an endotracheal tube with an inner diameter of 7.0 mm into which a stylet was inserted (Fig. 2). Propofol 80 mg and rocuronium 30 mg were injected intravenously as preparation for the induction. While securing the airway, the patient grimaced in pain once, but she followed the instructions well and did not execute any defensive motion. Anesthesia was maintained with sevoflurane 1.2 vol% and remifentanil 0.2-0.3 µg/kg/min, and methylprednisolone 125 mg was administered to prevent postoperative laryngeal edema. The intraoperative vital signs of the patient were stable and there were no specific findings during the operation, which continued for 2.5 hours. Extubation was carried out after confirming the recovery of consciousness and spontaneous breathing after the operation had finished. The patient was transferred to the postanesthetic care unit, and there were no specific findings in that ward as well. The tumor mass was diagnosed as a schwannoma in a histological examination and the patient was discharged 7 days after the operation.
An operation method through the oral cavity was determined considering the patient's repulsion upon the suggestion of a method through the nasal cavity, which she had experienced before. Another factor was the risk of hemorrhaging during the introduction of the bronchoscope. We decided to use the GVL, as it was expected that the bronchoscope tip would not easily reach the entrance of the vocal cord due to the change in the anatomical structure caused by the supraglottic mass when the flexible bronchoscope was introduced through the oral cavity. There have been many reports of cases in which difficult airway management was successfully performed using the GVL and a bronchoscope together. Moore and Wong [4] reported that they could perform intubation relatively easily in an obese patient, despite the fact that a challenging airway management situation had been expected, as they took advantage of the flexibility of the bronchoscope as they watched the GVL monitor. Sukernik et al. [5] introduced the protocol of using the GVL in conjunction with a flexible bronchoscope for patients in whom a challenging airway management scenario is expected. For patients of Cormack-Lehane Grade 1 or 2 based on an oral cavity observation with the GVL, they suggested the method of moving the tip of a flexible bronchoscope directly to the vocal cord while watching its progress on the GVL monitor. For patients of Grade 3 or 4, they suggested a method in which the operator attempts endotracheal intubation, checking the vocal cord through the images displayed by the bronchoscope, while an assistant observes the moving direction of the flexible bronchoscope tip through the GVL monitor and gives directions to the operator. Xue et al. [6] reported that they performed endotracheal intubation successfully in a relatively easy manner by applying the method described above with 13 patients for challenging endotracheal intubation scenarios were expected.
In the present case, a method involving the use of a flexible bronchoscope in conjunction with the GVL was chosen to secure the airway, but the endotracheal intubation process failed. The first possible reason for the failure was that the bronchoscope tip was not moved forward owing to the tumor mass and the anatomical change of the aryepiglottic fold. Asai and Shingu [7] stated that the small space due to the anatomical structure of the posterior pharynx and the larynx is a typical reason for a failure of endotracheal intubation using a flexible bronchoscope. It was also reported that the tip of the endotracheal tube could be resisted by an anatomical structure such as the aryepiglottic fold when it was inserted through the top of the bronchoscope [8]. Second, the bronchoscope was not strong enough to push the tumor mass and the surrounding structures away due to its thinness. Hakala and Randell [9] reported that the success ratio was high when a thick endoscope was employed. In our case, the thin bronchoscope was not strong enough to move the tumor mass, which was a large, solid and fixed schwannoma that extended from the left aryepiglottic fold to the epiglottis. In most case reports in which endotracheal intubation succeeded with a flexible bronchoscope, the supraglottic mass was a pyriform cyst that was not firmly fixed. It was reported that a bronchoscope could be inserted by pushing the tumor mass aside with the tip, although careful operation of the bronchoscope was required in the case of a pyriform cyst due to the risk of hemorrhaging and dropout [10-12]. The final reason may be that the tumor mass was not moved aside and thus impeded the tip of the GVL blade, which was simply used as a camera to watch the moving direction of the bronchoscope tip. Additionally, the assistant was not given an active assignment to expose the vocal cord, such as by pressing the part near the cricoid cartilage.
Moorthy et al. [13] studied airway management with 801 patients who had a supraglottic mass and classified them into four categories (Moorthy's airway category) based on their clinical symptoms and the findings using a laryngoscope and a flexible bronchoscope. They recommended the use of airway management algorithms during induction for the patients in each category. The patients for whom airway management is difficult are grades as Grades 2b, 3 or 4. The patient in the present case report was classified into Moorthy's airway category Grade 3 or 4 because only a part of the vocal cord was observed after making considerable effort to do so. Thus, the recommended method of endotracheal intubation was through a flexible bronchoscope or directly through a laryngoscope, and tracheostomy had to be considered if a challenging situation arose.
The advantages of using the GVL are as follows: First, the visible part of the airway can be enlarged on the monitor and the operator can observe the details, even when the blade is not accurately located at the centerline of the vocal cord. Second, the tip of the GVL blade is bent by 60 degrees, allowing structures that are not readily observed by general laryngoscopes to be observed; moreover, the blade can be easily bent. Third, other medical staff members can also observe the progress simultaneously [3,14]. Therefore, the success ratio of intubation can be increased using the GVL and a flexible bronchoscope together in an organized manner.
As a result of the findings of this article, we recommend an airway management method that includes the operation of a GVL blade and cooperative pressing of the cricoid cartilage by an assistant for the awake orotracheal intubation of a patient with a fixed supraglottic mass. This paper reports such a case with a related literature survey.
References
1. Bradley PJ. Treatment of the patient with upper airway obstruction caused by cancer of the larynx. Otolaryngol Head Neck Surg 1999; 120: 737-741. PMID: 10229602.


2. Kanaya N, Nakayama M, Seki S, Kawana S, Watanabe H, Namiki A. Two-person technique for fiberscope-aided tracheal intubation in a patient with a long and narrow retropharyngeal air space. Anesth Analg 2001; 92: 1611-1613. PMID: 11375856.


3. Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth 2005; 52: 191-198. PMID: 15684262.


4. Moore MS, Wong AB. GlideScope intubation assisted by fiberoptic scope. Anesthesiology 2007; 106: 885PMID: 17413943.


5. Sukernik MR, Bezinover D, Stahlman B, Vaida S, Pott L. Combination of Glidescope with fiberoptic bronchoscope for the optimization of difficult endotracheal intubation. A case series of three patients 2009;1;Available from
http://priory.com/medicine/Glidescope_bronchoscope.htm.
6. Xue FS, Li CW, Zhang GH, Li XY, Sun HT, Liu KP, et al. GlideScope-assisted awake fibreoptic intubation: initial experience in 13 patients. Anaesthesia 2006; 61: 1014-1015. PMID: 16978330.


7. Asai T, Shingu K. Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions. Br J Anaesth 2004; 92: 870-881. PMID: 15121723.



8. Wulf H, Brinkmann G, Rautenberg M. Management of the difficult airway. A case of failed fiberoptic intubation. Acta Anaesthesiol Scand 1997; 41: 1080-1082. PMID: 9311412.


9. Hakala P, Randell T. Comparison between two fibrescopes with different diameter insertion cords for fibreoptic intubation. Anaesthesia 1995; 50: 735-737. PMID: 7645711.


10. Rivo J, Matot I. Asymptomatic vallecular cyst: airway management considerations. J Clin Anesth 2001; 13: 383-386. PMID: 11498322.


11. Kim SH, Park WK, Choi HS, Oh KM, Hong SJ. The two step fiberoptic approach in the management of a difficult pediatric airway due to a vallecular cyst. Korean J Anesthesiol 2001; 40: 261-264.

12. Lee SY, Hahm TS, Jin HS. Endotracheal intubation in a patient with an almost complete obstruction of the glottis due to a movable supraglottic tumor: a case report. Korean J Anesthesiol 2009; 56: 87-91.


13. Moorthy SS, Gupta S, Laurent B, Weisberger EC. Management of airway in patients with laryngeal tumors. J Clin Anesth 2005; 17: 604-609. PMID: 16427530.


14. Benjamin FJ, Boon D, French RA. An evaluation of the GlideScope, a new video laryngoscope for difficult airways: a manikin study. Eur J Anaesthesiol 2006; 23: 517-521. PMID: 16672094.


- TOOLS