 |
 |
| Korean J Anesthesiol > Volume 76(1); 2023 > Article |
|
Abstract
Background
The tracheal bronchus in Kartagener syndrome (KS) is a rare case that may cause difficulty in one-lung ventilation (OLV). Here we reported a case of successful OLV using bronchial blocker in a patient with tracheal bronchus and KS.
Case
A 66-year-old female patient with KS was admitted for left-side diaphragmatic plication. The patientŌĆÖs preoperative computed tomography image showed a tracheal bronchus of the apical segment in the right upper lobe. The patient received epidural analgesia and general anesthesia through total intravenous anesthesia. An EZ-Blocker┬« (Teleflex Life Sciences Ltd., Ireland) was used to perform OLV.
Kartagener syndrome (KS) is a subset of primary ciliary dyskinesia that is inherited in an autosomal recessive manner. Its clinical features include situs inversus, chronic sinusitis, and bronchiectasis [1]. The decreased ciliary function causes frequent respiratory infections in neonates with defective mucociliary clearance [2].
The tracheal bronchus is a congenital anomaly of bronchial variations with an incidence of 0.001ŌĆō2%. The normal right upper lobe (RUL) bronchus arises 1ŌĆō3 cm distal to the carina. However, the tracheal bronchus is usually seen 2ŌĆō6 cm above the carina. It is associated with other congenital anomalies such as Down syndrome and congenital heart disease [2ŌĆō4].
Until now, there have been no reports of tracheal bronchus in patients with KS. We describe the case of one-lung ventilation (OLV) using an EZ-Blocker® (EZB, Teleflex Life Sciences Ltd., Ireland) during thoracic surgery in a tracheal bronchus patient with KS.
A 66-year-old female patient with KS, 150 cm in height and 47 kg in weight, underwent left-side diaphragmatic plication. She had undergone surgery for diaphragmatic palsy 18 years prior. Routine laboratory tests showed normal results, and atrial premature contractions were frequently observed during electrocardiography. The patientŌĆÖs chest radiography and computed tomography revealed dextrocardia and bronchiectasis without situs inversus. In addition, patients had a tracheal bronchus of the apical segment in the RUL (Fig. 1). Auscultation was normal, and the pulmonary function test showed a mild restrictive pattern. The day before surgery, we explained our plan for airway management and the risk of failure of OLV and got written informed consent. The written informed consent of publication for the use of photos and case details in this report has been obtained.
The patient received a 0.2 mg intramuscular injection of glycopyrrolate 30 min before the surgery. Baseline vital signs were checked upon the patientŌĆÖs arrival in the operating room. The patient was placed in a left lateral decubitus position during the procedure. An epidural block was performed at the T4 level, with a test dose of 3 ml (2% lidocaine with 1 : 200,000 epinephrine) and a loading dose of 5.5 ml (fentanyl: 50 ╬╝g, 0.75% ropivacaine: 1 ml, and normal saline: 3.5 ml) administered through the catheter. A patient-controlled epidural analgesia device was set with a bolus dose of 3 ml, a lockout interval of 5 min, and a no-limit of 4 h. Anesthesia was induced and maintained using target controlled infusion of propofol at target concentration of 3ŌĆō4 ┬Ąg/ml and remifentanil at concentration of 3ŌĆō6 ng/ml. The right radial artery was used for arterial line placement. We performed a fiberoptic bronchoscopy assisted intubation using a single-lumen endotracheal tube (SLT, size: 7.5, cuffed; TaperGuardTM, Covidien, Ireland). Results of the fiberoptic bronchoscopy showed a tracheal bronchus of the RUL apical segment that mimicked a normal carina (Fig. 2). The tracheal bronchus had a smaller diameter compared to a normal carina and a sharp bifurcation angle at divergence. As the fiberoptic bronchoscope advanced into the main trachea, an actual tracheal carina was observed (Fig. 3). Under the bronchoscopic vision, in which the endotracheal tube is placed above the tracheal bronchus, the EZB was lubricated and introduced until its distal ends reached the right and left main-stem bronchus (Fig. 4). After the EZB was positioned properly, the endotracheal tube was readvanced carefully into the trachea not to obstruct the opening of tracheal bronchus. We disconnected the tube for 20 s to collapse the operated lung and reinflate the left-side cuff of the EZB. A pressure-controlled volume guaranteed ventilation mode was used. The patient received a tidal volume of 5ŌĆō6 ml/kg with a fraction of inspired oxygen of 0.6ŌĆō0.7. Furthermore, the inspiratory:expiratory (I:E) ratio was 1:2. The respiratory rate was adjusted to keep the end-tidal carbon dioxide partial pressure between 30 and 40 mmHg. The operation took 2 h and 45 min, and anesthesia was administered for 4 h. After extubation, the patient was transferred to the post-anesthesia care unit. To stabilize the patientŌĆÖs vital signs, we administered 3 L/min of supplemental oxygen through a nasal cannula. The patient was discharged uneventfully on the fifth postoperative day.
Here we reported a case of using EZB in a patient with tracheal bronchus. The patientŌĆÖs underlying disease was KS that usually accompanies with dextrocardia and bronchiectasis [1]. Tracheal bronchus is known to be associated with other congenital anomalies, such as Down syndrome, VATER (vertebrae, anus, trachea, esophagus, renal) syndrome, tracheoesophageal fistula, esophageal atresia, laryngeal and duodenal webs, spinal fusion and cardiac congenital defects, and hypoplastic lung [2ŌĆō4]. There have been no reports of tracheal bronchus in patients with KS.
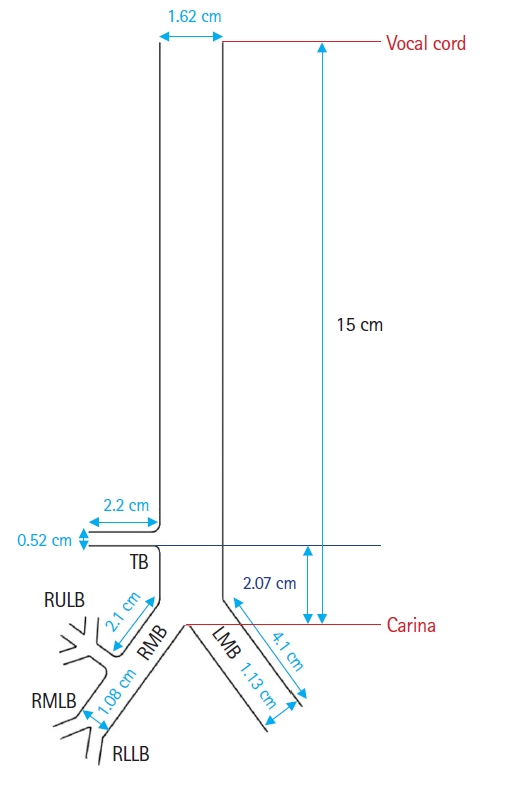
The tracheal bronchus is subdivided into the displaced type or supernumerary type. A displaced tracheal bronchus refers to a normal RUL bronchus or segment that is transposed from the right main bronchus to the trachea. In such cases, there is no RUL bronchus originating from the right main bronchus. A supernumerary tracheal bronchus is an accessory segment or bronchus where there is a normal trifurcation of the RUL bronchus [5]. This patient has a supernumerary tracheal bronchus showing an extra RUL that has its origin above the carina (Fig. 5).
OLV is challenging in patients with lung anomalies such as tracheal bronchus. The tracheal bronchus is an abnormal branch near the carina, making it difficult to determine which tube is better for OLV. Several devices can be used to separate the lungs, including the double-lumen tube (DLT). The DLT is the most widely used device for OLV. There was also a case of successful right-lung isolation for left pneumonectomy using DLT in a patient with a right tracheal bronchus [6]. However, the use of DLTs has limitations and complications. They are larger than conventional endotracheal tubes and are often more difficult to correctly insert. Additionally, they are associated with vocal cord damage and tracheal ruptures. Using these devices in patients with difficult airways may be more problematic. There is a report of unsuccessful attempts at positioning a DLT to achieve lung isolation in the case of a patient who has a more complex torsion structurally accompanied by a tracheal bronchus [7]. In addition, the tracheal cuff of the DLT can block the tracheal bronchus because it is fixed above the carina [8]. Even in our patient, the length from the carina to the bronchus opening was only 2.07 cm, so there was a high risk of blockage of the opening when using DLT (Fig. 5). Moreover, when the patient requires postoperative ventilation, the DLT should be changed to SLT after surgery.
Bronchial blocker (BB) is an alternative to the use of DLTs. Using a BB with a SLT can minimize airway damage when a patient is placed on a ventilator immediately after surgery. With BBs, lung isolation can be selectively performed even with an abnormally-structured bronchus. However, BBs are less stable and take longer to fix than DLTs [9]. There are several types of conventional BBs, including the wire-guided endo-bronchial Arndt blocker, Cohen flex-tip blocker, and Univent torque control blocker. A conventional BB is easy to use, but it is difficult to reposition if there is a change in the posture.
An EZB is a novel bronchial blocker. Minimum 7 mm of inner diameter of SLT allows easy insertion of an EZB as well as easy positioning and repositioning during surgery. An EZB further eliminates the need for careful size adjustment with each patient. However, there are disadvantages to using the EZB in patients with lung anomalies. Because they have a fixed shape, EZBs are difficult to use in anomalies near the carina. In this case, there was no other anatomical distortion except the tracheal bronchus, and the Y-shaped design of the EZB allowed the blocker to anchor on the carina and lead to positional stability comparing with other BBs. The insertion time of an SLT with an EZB was longer owing to two separate actionsŌĆöintubation with a single lumen and insertion of the EZB [10]. However, although the overall anesthesia duration could be prolonged, it was determined that the risk of aspiration could be reduced by using SLT to intubate faster than DLT to secure the airway safely. A previous study [11] reported a slower alveolar collapse in non-dependent lung when using a BB, but this was solved by disconnecting the SLT before OLV.
Since the patient was scheduled for left-lung surgery, we successfully performed OLV using the EZB without side effects. If the patient had a tracheal bronchus on the side that required surgery, it would have been significantly difficult to achieve complete OLV with the EZB alone.
NOTES
Conflicts of Interest
Eunsoo Kim has been an editor for the Korean Journal of Anesthesiology since 2016. However, he was not involved in any process of review for this article, including peer reviewer selec┬Łtion, evaluation, or decision-making. There were no other poten┬Łtial conflicts of interest relevant to this article.
Fig.┬Ā1.
The serial axial computed tomography images of cranial to caudal. A small tracheal bronchus (arrow) was observed in the apical segment of the right upper lobe.

Fig.┬Ā2.
The tracheal bronchus of the right upper lobe (RUL) apical segment. The tracheal bronchus of the RUL apical segment (arrow) mimics the normal carina.

Fig.┬Ā3.
The actual tracheal carina. As the fiberoptic bronchoscope advanced into the main trachea, an actual tracheal carina was observed.
Fig.┬Ā4.
The placement of the EZ-Blocker® (EZB) into the right and left main-stem bronchus. Under the bronchoscopic vision, an endotracheal tube is placed above the tracheal bronchus, and an EZB is introduced until its distal end reaches the right and left main-stem bronchus.

Fig.┬Ā5.
The schematic of structure of tracheal bronchus. The opening of the tracheal bronchus is located 2.07 cm above the carina. Tracheal bronchus was a supernumerary type showing an extra right upper lobe that has its origin above the carina. TB: tracheal bronchus, RMB: right main bronchus, LMB: left main bronchus, RULB: right upper lobe bronchus, RMLB: right middle lobe bronchus, RLLB: right lower lobe bronchus.
References
1. Mishra M, Kumar N, Jaiswal A, Verma AK, Kant S. Kartagener's syndrome: A case series. Lung India 2012; 29: 366-9.



3. Kim H, Kim Y, Jou S, Lee W. True tracheal bronchus: classification and anatomical relationship on multi-detector computed tomography. J Korean Soc Radiol 2017; 76: 264-72.


4. Doolittle AM, Mair EA. Tracheal bronchus: classification, endoscopic analysis, and airway management. Otolaryngol Head Neck Surg 2002; 126: 240-3.



5. Suzuki M, Matsui O, Kawashima H, Takemura A, Matsubara K, Hayashi N, et al. Radioanatomical study of a true tracheal bronchus using multidetector computed tomography. Jpn J Radiol 2010; 28: 188-92.



6. Kawagoe I, Kohchiyama T, Hayashida M, Satoh D, Suzuki K, Inada E. Successful one-lung ventilation with a right-sided double-lumen tube in a patient with a right upper tracheal bronchus, who underwent left pneumonectomy for left hilar lung cancer. Masui 2016; 65: 594-8.

7. Yoshimura T, Ueda KI, Kakinuma A, Nakata Y. Difficulty in placement of a left-sided double-lumen tube due to aberrant tracheobronchial anatomy. J Clin Anesth 2013; 25: 413-6.


8. Ho AM, Karmakar MK, Lam WW, Lam FO, Lee TW, Ng SK, et al. Does the presence of a tracheal bronchus affect the margin of safety of double-lumen tube placement? Anesth Analg 2004; 99: 293-5.


9. Clayton-Smith A, Bennett K, Alston RP, Adams G, Brown G, Hawthorne T, et al. A comparison of the efficacy and adverse effects of double-lumen endobronchial tubes and bronchial blockers in thoracic surgery: a systematic review and meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth 2015; 29: 955-66.


-
METRICS

-
- 1 Crossref
- Scopus
- 2,917 View
- 205 Download








