3. Chan MT, Hedrick TL, Egan TD, García PS, Koch S, Purdon PL, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on the role of neuromonitoring in perioperative outcomes: electroencephalography. Anesth Analg 2020; 130: 1278-91.


5. Disma N, Veyckemans F, Virag K, Hansen TG, Becke K, Harlet P, et al. Morbidity and mortality after anaesthesia in early life: results of the European prospective multicentre observational study, neonate and children audit of anaesthesia practice in Europe (NECTARINE). Br J Anaesth 2021; 126: 1157-72.

6. Constant I, Sabourdin N. The EEG signal: a window on the cortical brain activity. Paediatr Anaesth 2012; 22: 539-52.


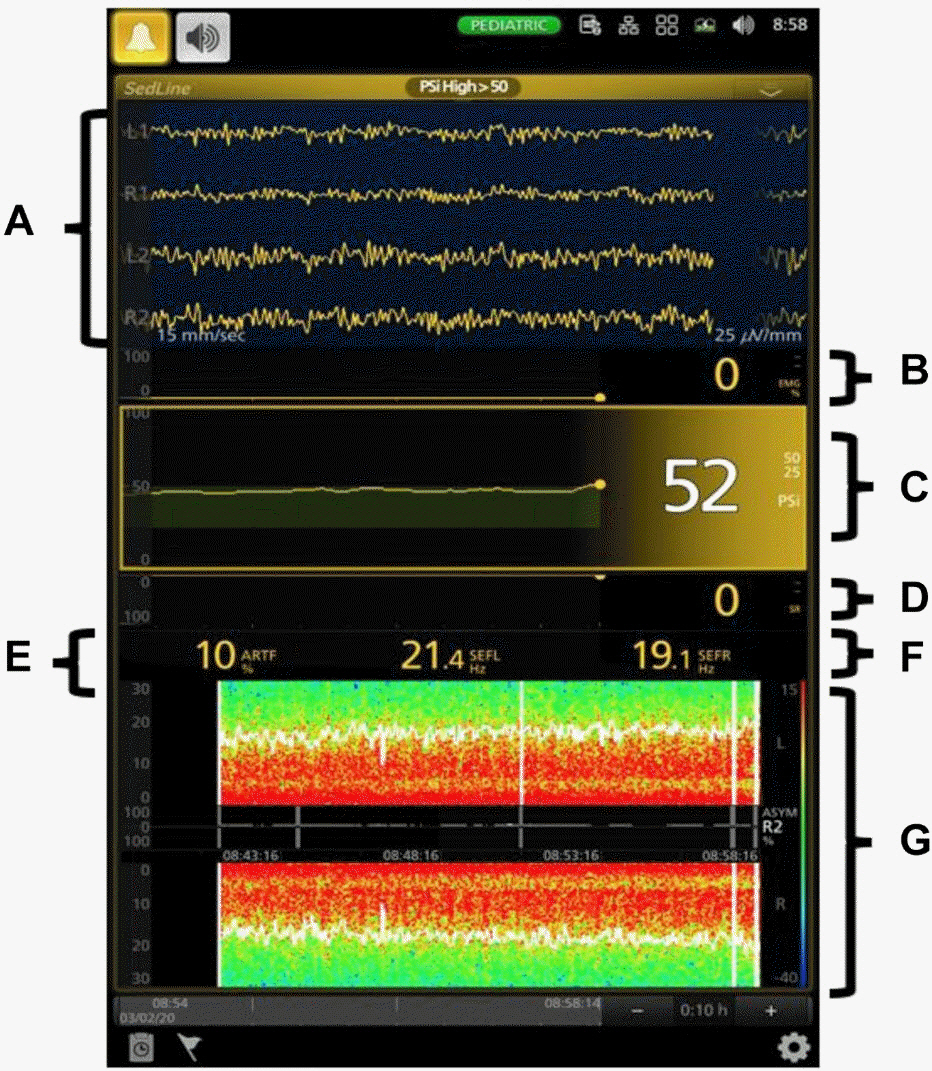
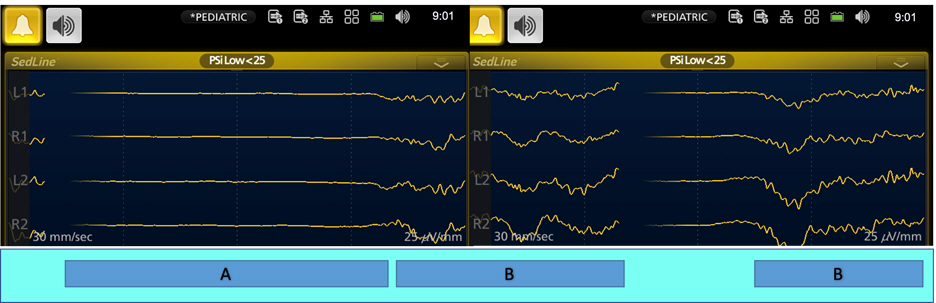
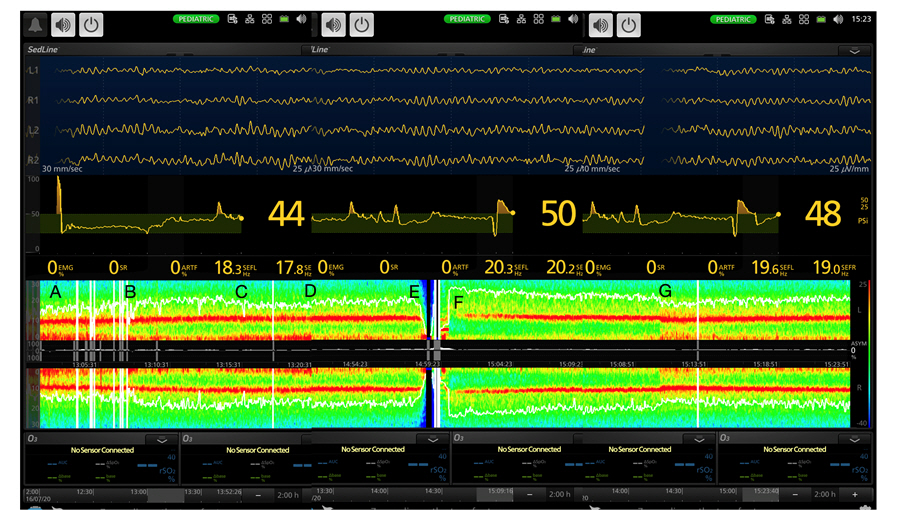
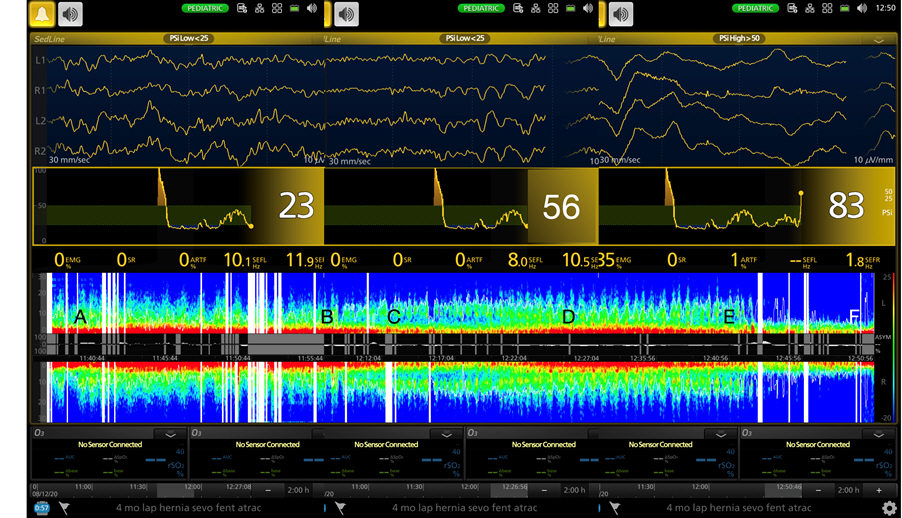
7. Yuan I, Xu T, Kurth CD. Using electroencephalography (EEG) to guide propofol and sevoflurane dosing in pediatric anesthesia. Anesthesiol Clin 2020; 38: 709-25.


9. Bowyer SM. Coherence a measure of the brain networks: past and present. Neuropsychiatr Electrophysiol 2016; 2: 1.


10. Yuan I, Chao JY, Kurth CD, Missett R, Cornelissen L. Intraoperative EEG monitoring in pediatric anesthesia. Curr Anesthesiol Rep 2023; 13: 135-42.


11. Markus M, Nagelsmann H, Schneider M, Rupp L, Spies C, Koch S. Peri- and intraoperative EEG signatures in newborns and infants. Clin Neurophysiol 2021; 132: 2959-64.


17. Desowska A, Berde CB, Cornelissen L. Emerging functional connectivity patterns during sevoflurane anaesthesia in the developing human brain. Br J Anaesth 2023; 130: e381-90.


21. Zakaria L, Desowska A, Berde CB, Cornelissen L. Electroencephalographic delta and alpha oscillations reveal phase-amplitude coupling in paediatric patients undergoing sevoflurane-based general anaesthesia. Br J Anaesth 2023; 130: 595-602.


22. Liang Z, Ren N, Wen X, Li H, Guo H, Ma Y, et al. Age-dependent cross frequency coupling features from children to adults during general anesthesia. NeuroImage 2021; 240: 118372.


24. Fahy BG, Chau DF. The technology of processed electroencephalogram monitoring devices for assessment of depth of anesthesia. Anesth Analg 2018; 126: 111-7.


25. Bong CL, Balanza GA, Khoo CE, Tan JS, Desel T, Purdon PL. A narrative review illustrating the clinical utility of electroencephalogram-guided anesthesia care in children. Anesth Analg 2023; 137: 108-23.


27. Jeleazcov C, Schmidt J, Schmitz B, Becke K, Albrecht S. EEG variables as measures of arousal during propofol anaesthesia for general surgery in children: rational selection and age dependence. Br J Anaesth 2007; 99: 845-54.


31. Sadhasivam S, Ganesh A, Robison A, Kaye R, Watcha MF. Validation of the bispectral index monitor for measuring the depth of sedation in children. Anesth Analg 2006; 102: 383-8.


32. Ricci Z, Robino C, Rufini P, Cumbo S, Cavallini S, Gobbi L, et al. Monitoring anesthesia depth with patient state index during pediatric surgery. Paediatr Anaesth 2023; 33: 855-61.


36. Hagihira S. Changes in the electroencephalogram during anaesthesia and their physiological basis. Br J Anaesth 2015; 115 Suppl 1: i27-31.


42. Koch S, Stegherr AM, Mörgeli R, Kramer S, Toubekis E, Lichtner G, et al. Electroencephalogram dynamics in children during different levels of anaesthetic depth. Clin Neurophysiol 2017; 128: 2014-21.


43. Hayashi K, Shigemi K, Sawa T. Neonatal electroencephalography shows low sensitivity to anesthesia. Neurosci Lett 2012; 517: 87-91.


45. Jones Oguh S, Iyer RS, Yuan I, Missett R, Daly Guris RJ, Johnson G, et al. Implementation of an electroencephalogram-guided propofol anesthesia practice in a large academic pediatric hospital: a quality improvement project. Paediatr Anaesth 2024; 34: 160-6.


46. Constant I, Seeman R, Murat I. Sevoflurane and epileptiform EEG changes. Paediatr Anaesth 2005; 15: 266-74.


48. Miao M, Han Y, Zhang Y, Xu Y, Zhang L, Yang Y, et al. Epileptiform EEG discharges during sevoflurane anesthesia in children: a meta-analysis. Clin Neurophysiol 2022; 143: 48-55.


52. Britton JW, Frey LC, Hopp JL, Korb P, Koubeissi MZ, Lievens WE, et al. Electroencephalography (EEG): an introductory text and atlas of normal and abnormal findings in adults, children, and infants [Internet]. Chicago, American Epilepsy Society. 2016, pp 25-6.
https://www.ncbi.nlm.nih.gov/books/NBK390354/pdf/Bookshelf_NBK390354.pdf
53. Santa Cruz Mercado LA, Lee JM, Liu R, Deng H, Johnson JJ, Chen AL, et al. Age-dependent electroencephalogram features in infants under spinal anesthesia appear to mirror physiologic sleep in the developing brain: a prospective observational study. Anesth Analg 2023; 137: 1241-9.


54. Seltzer L, Swartz MF, Kwon J, Burchfiel J, Cholette JM, Wang H, et al. Neurodevelopmental outcomes after neonatal cardiac surgery: role of cortical isoelectric activity. J Thorac Cardiovasc Surg 2016; 151: 1137-42.


57. Yuan I, Landis WP, Topjian AA, Abend NS, Lang SS, Huh JW, et al. Prevalence of isoelectric electroencephalography events in infants and young children undergoing general anesthesia. Anesth Analg 2020; 130: 462-71.


69. Alkhatip AA, Kamel MG, Farag EM, Elayashy M, Farag A, Yassin HM, et al. Deep hypothermic circulatory arrest in the pediatric population undergoing cardiac surgery with electroencephalography monitoring: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth 2021; 35: 2875-88.


71. Long MH, Lim EH, Balanza GA, Allen JC Jr, Purdon PL, Bong CL. Sevoflurane requirements during electroencephalogram (EEG)-guided vs standard anesthesia care in children: a randomized controlled trial. J Clin Anesth 2022; 81: 110913.


73. Weber F, Walhout LC, Escher JC. The impact of Narcotrend™ EEG-guided propofol administration on the speed of recovery from pediatric procedural sedation-a randomized controlled trial. Paediatr Anaesth 2018; 28: 443-9.


75. Mason KP. Paediatric emergence delirium: a comprehensive review and interpretation of the literature. Br J Anaesth 2017; 118: 335-43.


76. Koch S, Rupp L, Prager C, Wernecke KD, Kramer S, Fahlenkamp A, et al. Emergence delirium in children is related to epileptiform discharges during anaesthesia induction: an observational study. Eur J Anaesthesiol 2018; 35: 929-36.


79. Kim J, Lee HC, Byun SH, Lim H, Lee M, Choung Y, et al. Frontal electroencephalogram activity during emergence from general anaesthesia in children with and without emergence delirium. Br J Anaesth 2021; 126: 293-303.