Introduction
Postoperative pain is a common problem that necessitates resolution without complications. The erector spinae plane block (ESPB) is currently used as a perioperative analgesic and postoperative pain management technique. Plane blocks are gaining popularity over neuraxial techniques because of the low risk of severe side effects. The ESPB, first described by Forero [
1] in 2016, is performed in patients experiencing chronic thoracic pain. Recent studies have demonstrated the effectiveness of ESPB in the thoracic and lumbar surgical areas [
2]. ESPB is performed by applying a local anesthetic between the transverse process of the vertebra and the erector spinae muscle [
2,
3].
ESPB applications are named according to the vertebral level at which they are performed; for instance, blocks performed at the level of the sacral vertebrae are called sacral ESPBs (SESPBs). According to the current literature, the SESPB has been applied using two approaches. First, an intermediate approach was described by Tulgar et al. [
4] in 2019 for postoperative analgesia in an adult patient who underwent pilonidal sinus surgery. In this approach, the SESPB technique involves placing the needle bilaterally on the intermediate crest. In the same year, Aksu and G├╝rkan [
5] reported adequate postoperative analgesia in a pediatric patient who underwent hypospadias surgery using the median approach to the SESPB, from the median sacral crest. There are radiological, anatomical, or clinical studies of SESPB in the current literature, but there is no anatomical and radiological study comparing the two methods of SESPB [
6ŌĆō
11]. The present cadaveric study aimed to determine the distribution of local anesthesia with the median and intermediate SESPB approaches. Radiological images and dissection results were compared to define the limits of distribution of the radiopaque solution.
Materials and Methods
A two-phase radiological and cadaveric study was performed. Ethics approval of this study was obtained from Karadeniz Technical University Faculty of Medicine with number: 2022/229 and the study protocol was registered on ClinicalTrials.gov (NCT05716061). After implementing the SESPB, the preliminary phase included radiological procedures, and the second phase included cadaveric dissections. Four embalmed cadavers (two female and two male; age at death: 68ŌĆō89 years) were included in the study. None of the cadavers had a history of trauma or sacral surgery.
The cadavers were categorized into two groups, with one female and one male in each group, and the SESPB was performed by an experienced anesthesiologist using the two different approaches under ultrasound (USG) guidance.
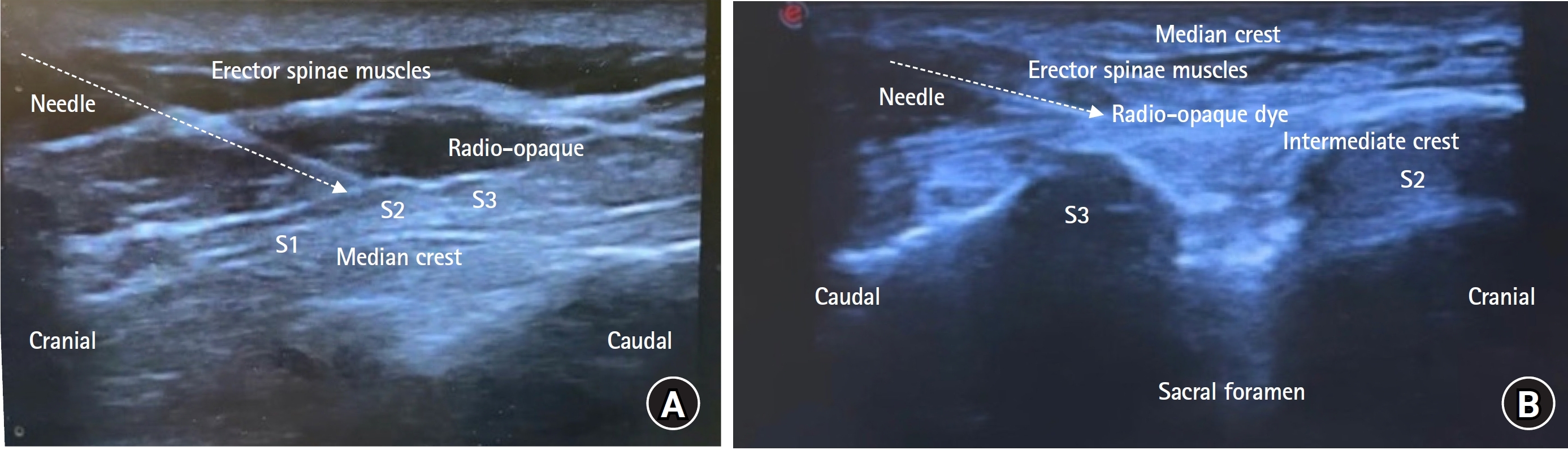
For the median approach, a linear probe covered with a sheath was positioned longitudinally at the midline at the level of the L5 spinous process. The median crest of the sacrum was observed, and the probe was moved caudally to visualize the first and second median sacral crest tips and the erector spinae muscle. As described by Aksu and G├╝rkan, a 22-Gauge (G), 50-mm needle (Stimuplex
┬« Ultra360, B. Braun) was then inserted in the craniocaudal direction using the in-plane technique until the tip of the needle touched the second sacral crest. After negative aspiration, 2 ml saline was injected, and the localization of the needle tip was confirmed using USG. Finally, 40 ml of a blue solution, including 4 ml methylene blue, 20 ml radiopaque dye (Iohexol, Kopaq 350 mg/1 ml, Ko├¦sel), and 16 ml saline, was injected between the sacral crest and erector spinae muscle (
Fig. 1A).
For the intermediate approach, first described by Tulgar et al. [
4], the block was performed bilaterally (rather than unilaterally, as in the median approach). After the linear probe was covered with a sheath, the USG probe was placed longitudinally at the location exactly over the middle of the sacrum, and the second median crest was observed. The probe was then moved 1.5ŌĆō2 cm laterally and placed over the second median crest of the sacrum. A 22-G, 50-mm needle was inserted in the caudocranial direction using the in-plane technique. Following negative aspiration, 2 ml saline was injected. USG confirmed the location of the needle tip, and 20 ml red solution was injected into the area between the median and intermediate crests under the erector spinae muscles (
Fig. 1B) [
4]. The same block was applied to the right side. A total of 40 ml of solution was administered to the cadavers (20 ml on each side). The 20 ml solution contained 2 ml red acrylic dye, 10 ml radiopaque dye (Iohexol, Kopaq 350 mg/1 ml, Ko├¦sel), and 8 ml saline.
A different color dye was used for each technique to distinguish between the two methods of cadaveric imaging. Due to the cadaverŌĆÖs rigidity, injecting the solution was challenging, and performing the block was more difficult than it had been in vivo. However, the procedureŌĆÖs difficulty was consistent across both groups, regardless of the cadaverŌĆÖs sex.
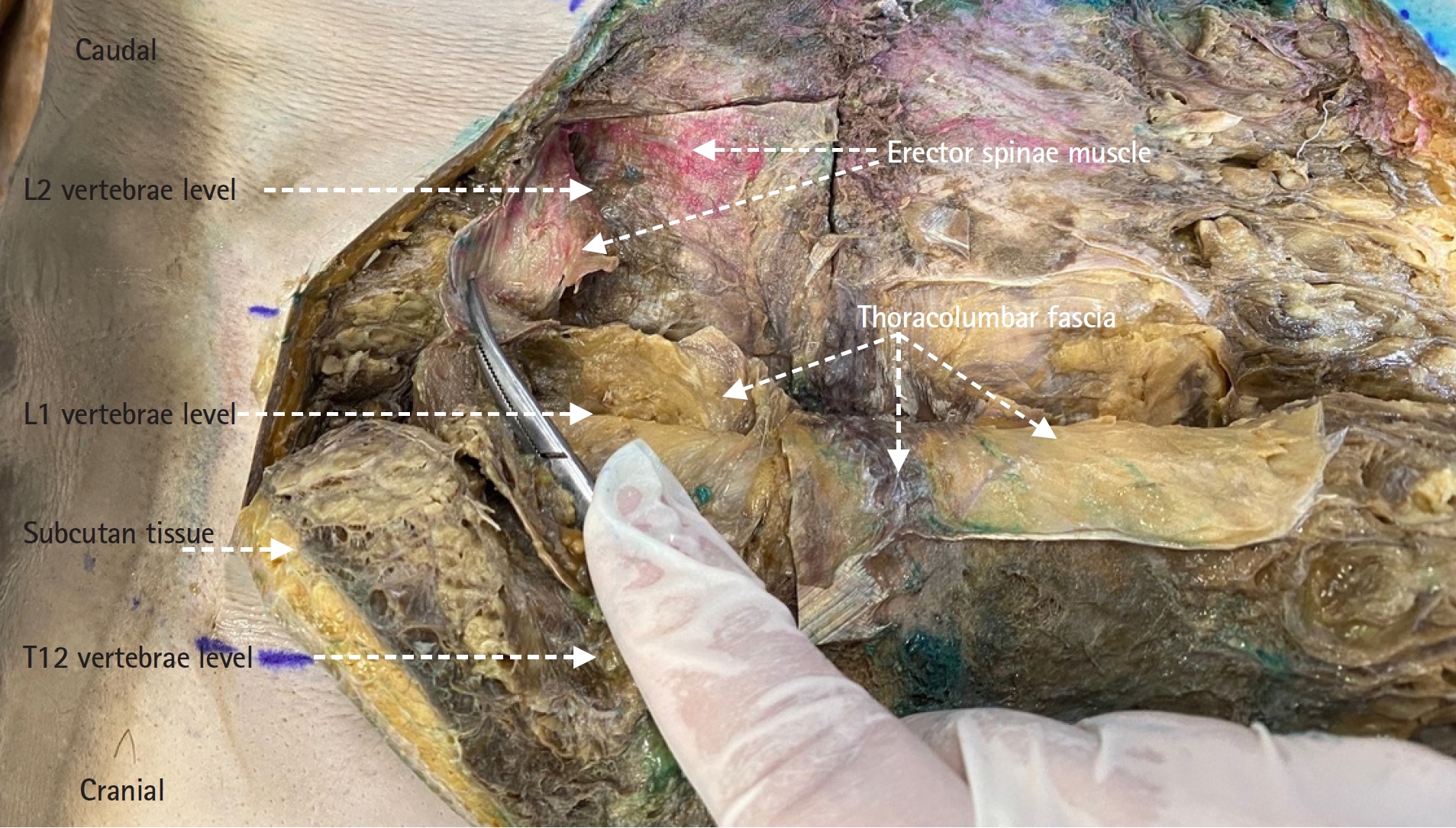
Within 30 min of injection, the cadavers were transferred to the Department of Radiology for computed tomography (CT) imaging. The scout view at 512 mm was used to obtain the scans, using a rotation time of 0.8 s, size collimation of 0.6 mm, 120 kv, and an effective current of 120ŌĆō480 mA (GE Revolution EVO systems). Axial, coronal, and sagittal reconstructions were performed with 1.25-mm sections to evaluate the distribution of the contrast material. Radiological imaging was completed within 30 minutes of administration. The cadavers were then returned to the Department of Anatomy and dissected by experienced anatomists to examine the distribution of the solution through the tissue planes. In the median group, a superficial subcutaneous area was dissected between the L5 and S5 horizontal planes from the medial to the lateral side in accordance with the radiologic results, and the distribution of the blue solution was observed. In the intermediate group, the subcutaneous area between the horizontal planes of L2 and S2 was dissected in the same way as in the first group. Then, according to the radiological results, the deep part of the erector spinae muscle group was also dissected, and the distribution of the red solution was observed.
Results
No differences were observed in the solution distribution between the male and female cadavers within each group. An experienced radiologist examined all the radiological results. The CT images were examined from the L1 horizontal level to the coccyx tip.
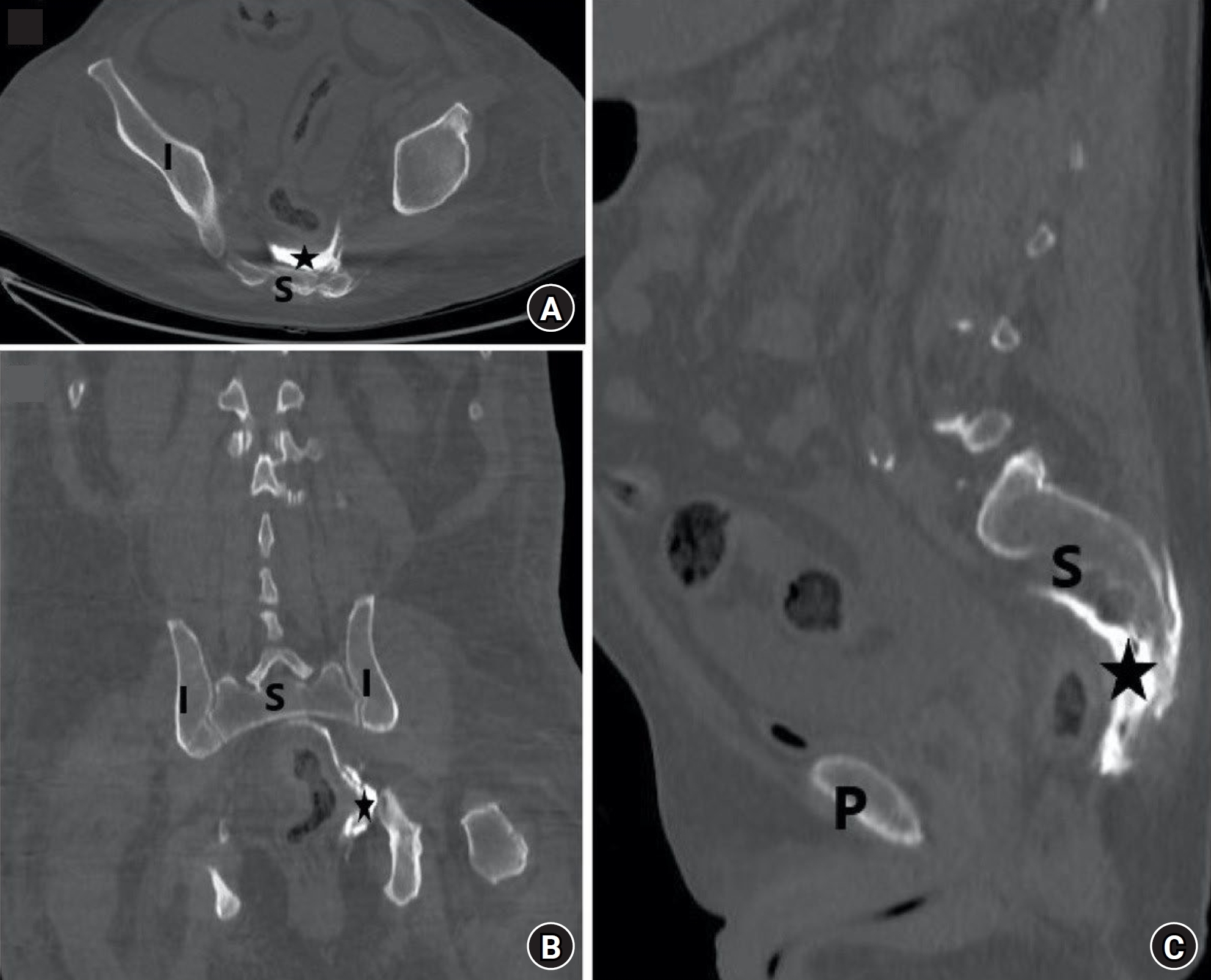
In the median group, CT images revealed subcutaneous pooling of radiopaque solution between the S1 and S5 horizontal planes. Additionally, passage of the radiopaque solution from the S2 to S5 levels through all the sacral foramina via the spinal nerves to the anterior aspect of the sacrum was observed (
Figs. 2AŌĆō
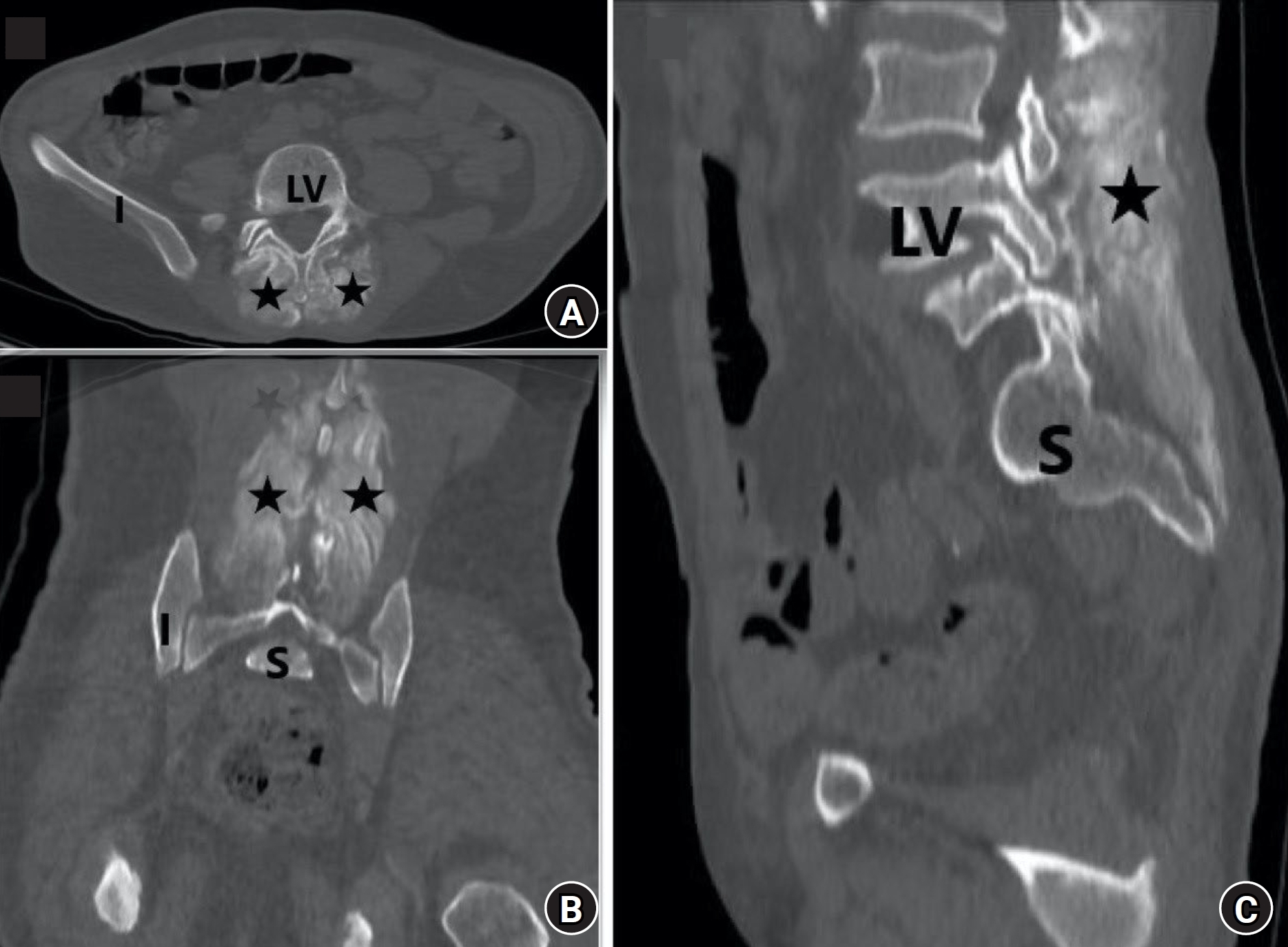
C). In the intermediate group, radiopaque solution distribution was observed along the bilateral erector spinae muscles between the L2 and S3 horizontal planes, and no anterior transition was detected (
Figs. 3AŌĆō
C).
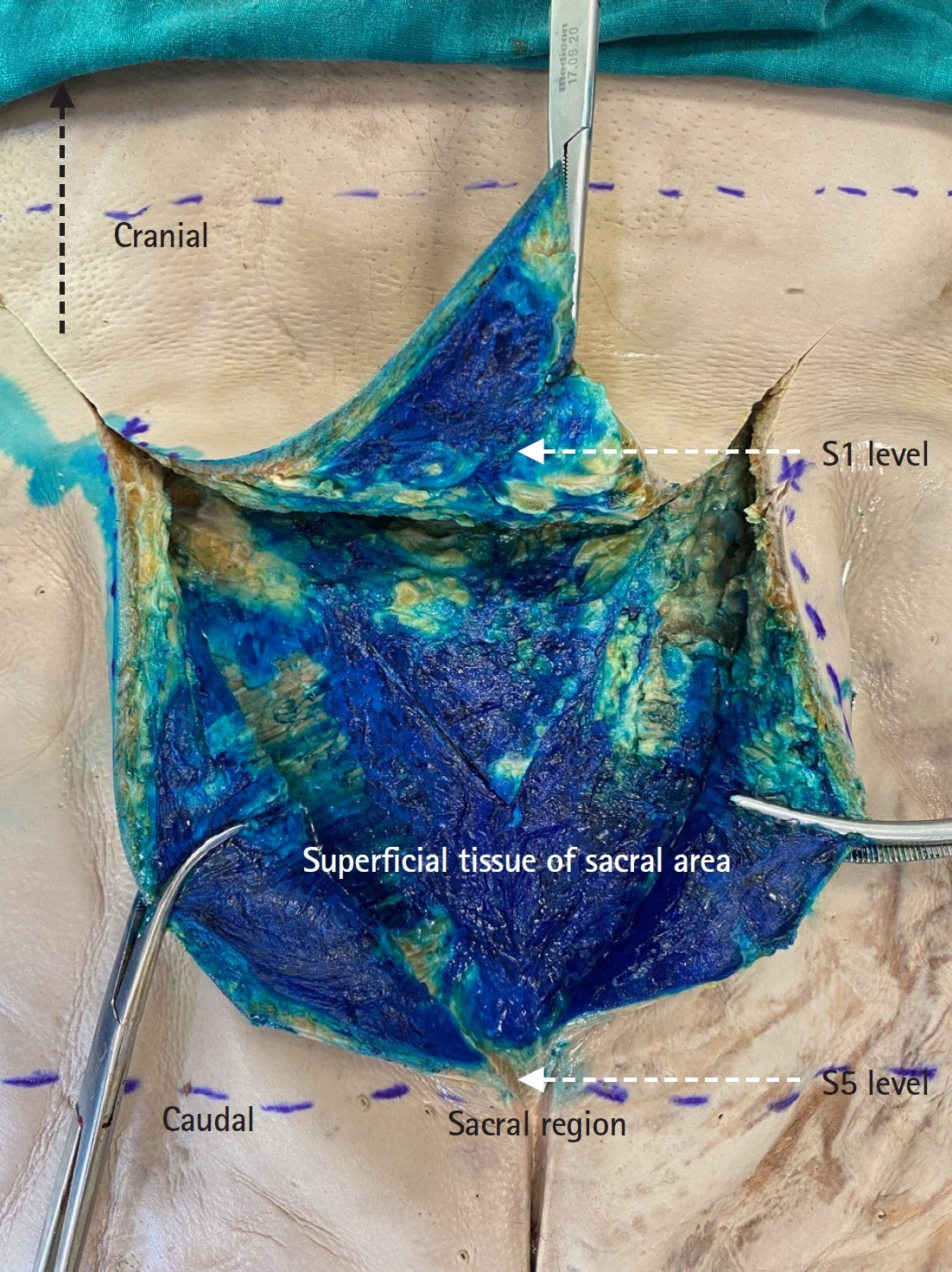
Anatomic dissections were performed from the superficial to deep tissue planes in both groups. In the median group, the distribution of the blue solution was observed in a 15 (horizontal) ├Ś 18.5 (vertical)-cm subcutaneous tissue area between the S1 and S5 horizontal planes (
Fig. 4). This area corresponds to the superficial tissue plane located between the skin and deep fascia of the back muscle group. The loose areolar tissue of the superficial compartment enabled the distribution of methylene blue solution over the deep fascia but not under the deep fascia or at the deep fascia covering the muscle plane.
In the intermediate group, as anticipated, the distribution of the red solution was not observed in the loose areolar tissue plane between the skin and deep fascia. After removing the loose areolar tissue, the deep fascia over the erector spinae was dissected. The muscle was then cut deeply in a vertical direction to observe the spread of the red solution. The red solution was detected cranially in the erector spinae muscle at the L2ŌĆōL3 intervertebral levels but not at the horizontal L2 vertebral level (
Fig. 5). Caudally, the red solution was detected in the muscle at the S2ŌĆōS3 intervertebral levels but not under the horizontal S3 vertebral level. At both levels, the distribution of the red solution was limited within the deep fascia enclosing the anterior portion of the erector spinae. The enclosed area included the arteries, veins, nerve structures of the muscle, and erector spinae.
Dissection revealed that the skin and deep fascia were the two main anatomical structures restricting the spread of the injected radiopaque solution. Consequently, the anatomical dissection results are closely aligned with the radiologic results.
Discussion
The current body of literature includes radiological, anatomical, and clinical studies on SESPBs. In our cadaveric study, anatomical and radiological findings results regarding the distribution patterns of the radiopaque dye for the two SESPB procedures were compared. In this study, we analyzed the SESPB methods described in the literature, using the highest volume of anesthetic agent reported to provide sufficient analgesia for both approaches to avoid any volume-based deficiency that could affect the distribution. Therefore, we administered a 40 ml radioopaque solution for both approaches.
With the median approach, the radiopaque solution spread only to the subcutaneous tissue, with no evidence of muscle involvement in the sacral region. A previous anatomical study conducted by Nanda et al. [
12] also examined the SESPB using the median approach and failed to observe any dye spread in the deep tissue compartments, including the sacral foramina and nerves, similar to our observation.
In our study, this distribution could not be demonstrated anatomically, but the radiological distribution of radiopaque dye to the anterior region was shown, this distribution may be volume-dependent. While Nanda used 20 ml for the block, we used a dose of 40 ml.
In addition, our radiological results revealed that the radiopaque solution passed from the sacral foramen to the anterior sacrum via the spinal nerves between the S2 and S5 levels. Here, the radiopaque dye may have diffused through the superficial tissues and reached the foramen, then traveled via the sacral nerves to the anterior part of the sacrum. Radiological observation of this distribution is important and may explain the findings from studies that have demonstrated adequate analgesia from the median SESPB approach.
In a clinical study conducted by Kukreja et al. [
10], postoperative analgesia was provided using the median SESPB approach in a sex reassignment surgery. Additionally, Aksu and G├╝rkan [
5] and Ûksüz et al. [
7] applied the median approach at the S4 level in pediatric anorectal and urogenital surgeries, respectively, and reported successful postoperative analgesia. Based on our radiological results, we believe that the anterior passage of the radiopaque solution may explain the successful analgesic effect on the sensory field of the pudendal and obturator nerves.
According to the literature, ESPBs are performed bilaterally at all vertebral levels; however, sacral ESPBs have only two approaches. The intermediate SESPB method has also been applied bilaterally, similar to other ESPB approaches [
1ŌĆō
4,
6,
9ŌĆō
11,
13ŌĆō
16]. In the intermediate approach, the solution was administered to the erector spinae muscle, approximately 1ŌĆō2 cm lateral to the median crest at the S2 level. Horizontal distribution of the dye longitudinally from the S3 to L2 level was observed. Similar to our study, previous anatomical and CT studies on thoracic and lumbar ESPBs have shown longitudinal spread of the dye, but not into the anterior passage [
3,
13,
14]. Theoretically, the dorsal ramus of the spinal nerves in the erector spinae muscle compartment at all levels is involved due to vertical spread. However, dorsal ramus involvement alone cannot explain the analgesic efficacy observed in some clinical trials focusing on thoracic and lumbar regions; the involvement of the anterior passage or ventral ramus is also required.
Adhikary et al. [
15] conducted a study on cadavers using magnetic resonance imaging after a thoracic ESPB and observed the distribution of the solution into the neural foramen and epidural space, confirming the anterior spread of the local anesthetic. In another cadaveric study evaluating ESPB at the level of the thoracic vertebrae, Bonvicini et al. [
16] revealed the diffusion of the dye ventrally into the intercostal spaces through the blood vessels connected to the nerve passing through the costotransverse foramen. In these two studies, unlike in our study, the anterior passage of the radiopaque solution in the thoracic region was demonstrated. Notably, the erector spinae muscle group is thinner in the thoracic region than in the sacral region, and it thickens as it descends. We evaluated the differences in the anterior passage of the radiopaque solution between the sacral and thoracic regions depending on the muscle thickness. Our findings suggested that in clinical studies comparing ESPBs, the vertebral level at which the block is applied should also be considered.
Diwan et al. [
17] conducted a cadaveric study in which they performed SESPBs using an intermediate approach by placing a catheter and administering a continuous infusion of radiopaque solution. Dissection findings in their study revealed the presence of methylene blue above and below the sacral multifidus muscle. They also observed staining of the sacral foramen and sacral nerves, with methylene blue leaking from the dorsal surface of the sacral foramen into the sacral epidural space. They attributed the diffusion of methylene blue into the ventral and epidural spaces to the injection of a continuous and pressurized volume of solution through the catheter. Our study results differed from this study as we administered a single injection rather than a continuous infusion through a catheter.
Mistry et al. [
11] performed an intermediate-approach SESPB in sacral spine surgery and observed selective sensory loss in the L4ŌĆōS3 dermatomes postoperatively. Piraccini et al. [
8] performed a unilateral, intermediate-approach SESPB, administering 15 ml of radiopaque solution at the S1 level to a patient with radicular pain. The patient's pain decreased after 20 minutes, according to a numerical rating scale, and he was able to stand and walk. Tulgar et al. [
4] reported an intermediate SESPB in pilonidal sinus surgery that provided adequate postoperative analgesia. In another clinical study, Kaya et al. [
6] achieved adequate analgesia using an intermediate SESPB in anorectal surgery. We believe that this analgesic efficacy could be attributed to the caudalŌĆōcranial spread of the solution between the erector spinae muscles and the involvement of the dorsal ramus of the spinal nerves in this region, as demonstrated in our study. This approach may provide adequate analgesia during surgeries involving the lower lumbar and sacral vertebrae, lumbar pain management, and orthopedic surgical interventions.
Tulgar described the administration of the erector spinae block at the sacral region for the first time in a letter and called it the ŌĆ£sacral erector spinae plane block.ŌĆØ In another letter published in 2020, Hamilton [
18] explained that erector spinae muscle fibers are more superficial above the multifidus in the sacral region, and thus, the name should be changed to ŌĆ£sacral multifidus block.ŌĆØ Piraccini and Taddei [
19] also argued that from an anatomical point of view, the name ŌĆ£sacral multifidus blockŌĆØ is more appropriate for the block. Although different definitions and names have been proposed, we believe that the clinical procedures described in previous studies all fall within the definition of the SESPB used in our study.
Our study was performed on four embalmed cadavers donated to the Anatomy Department of our institution. We would like to express our gratitude and commemorate these individuals for their contribution to our study.
The significant limitations of this study were the low number of cadavers owing to insufficient cadaver donation in our country and the implementation of ESPBs on embalmed cadavers. Although cadaveric study enabled us to explore the morphometry of the procedure methodology, comparing the results to those of living individuals is not straightforward. Nonetheless, this is unlikely to change our results because similar distributions have been reported in a recent study on ESPB interventions performed on fresh and embalmed cadavers [
12]. Our results revealed that the distribution of the radiopaque dye administered at the median and intermediate crests demonstrated significantly different characteristics. Additionally, the distribution of local anesthetic agents may differ in living bodies because of the differences in the density of solutions with and without radiopaque dye ingredients. Moreover, changes in the intra-abdominal pressure during breathing, blood circulation, muscle contraction, and body position can alter the spread
in vivo [
16].
In conclusion, this cadaveric and radiologic study demonstrated the anterior transition of the radiopaque dye solution only with the median SESPB approach. Although the intermediate SESPB approach demonstrated craniocaudal muscular spread, no anterior transition was observed. We believe that future combined studies should be conducted to investigate the methodology of ESPB procedures, as there are some inconsistencies among the results of previous studies.