 |
 |
| Korean J Anesthesiol > Volume 76(5); 2023 > Article |
|
Abstract
In the last quarter of a century, the backdrop of appropriate ambulatory and office-based surgeries has changed dramatically. Procedures that were traditionally done in hospitals or patients being admitted after surgery are migrating to the outpatient setting and being discharged on the same day, respectively, at a remarkable rate. In the face of this exponential growth, anesthesiologists are constantly being challenged to maintain patient safety by understanding the appropriate patient selection, procedure, and surgical location. Recently published literature supports the trend of higher, more medically complex patients, and more complicated procedures shifting towards the outpatient arena. Several reasons that may account for this include cost incentives, advancement in anesthesia techniques, enhanced recovery after surgery protocols, and increased patient satisfaction. Anesthesiologists must understand that there is a lack of standardized state regulations regarding ambulatory surgery centers and office-based surgery centers. Current and recently graduated anesthesiologists should be aware of the safety concerns related to the various non-hospital-based locations, the sustained growth and demand for anesthesia in the office, and the expansion of mobile anesthesia practices in the US in order to keep up and practice safely with the professional trends. Continuing procedural ambulatory shifts will require ongoing outcomes research, likely prospective in nature, on these novel outpatient procedures, in order to develop risk stratification and prediction models for the selection of the proper patient, procedure, and surgery location.
The landscape of ambulatory and office-based surgeries has been changing over the last twenty-five years. Procedures that were traditionally done in hospitals are migrating to the outpatient setting at a remarkable rate. This rapid expansion, in turn, has increased awareness to patient safety considerations for outpatient procedures that includes understanding the appropriate patient, procedure, and location where the procedure will be performed. In addition, one must also consider the choice of anesthesia techniques, personnel, available resources, and emergency preparedness.
Surgical procedures within the United States (US) are increasingly shifting to outpatient or non-hospital locations, as seen in the expected 4% annual expansion rate of the ambulatory surgery center (ASC) market over the ten-year period from 2017 to 2027 [1–3]. In 2018, Young et al. [4] reported that there were millions of procedures performed annually in the ambulatory setting as of 2014. There is an expected increase to 144 million procedures by 2023 [5]. In 2005, hospital-based outpatient departments (HOPDs) were performing 59% of outpatient cases versus 41% by ASCs. By 2020, this proportion has reversed with HOPDs performing 40% of cases, ASCs with 36%, and offices with 24% [5]. On average, an important contribution towards the shift in procedural location is that surgeries performed at ASCs cost 60% of HOPDs. More complex patients (American Society of Anesthesiologists [ASA] Physical Status [PS] III or higher) are having their surgeries and procedures performed in the ambulatory setting as well [6]. The outpatient facility may be a stand-alone ASC, a facility attached to a hospital outpatient department, or even an office. Some of these environments may not have the necessary equipment to monitor complex patients or to deal with a medical emergency [7]. Understanding these factors within the outpatient procedural or surgical setting is the key to patient safety. Anesthesiologists play an important role in selecting patients that are appropriate for the outpatient setting that may reduce the likelihood of complications and readmission rates via adequate pain control, use of multimodal anesthesia, adequate post-operative nausea and vomiting (PONV), and ensuring that patients are medically optimized before their procedure.
Concurrently, several incentives have arisen to drive procedures from the ASC to the office-based surgery (OBS) center. According to the Healthcare Cost and Utilization Project, some of the most common ambulatory procedures include ophthalmologic lens and cataract procedures, musculoskeletal procedures, cholecystectomies, hernia repairs, breast procedures, tonsillectomies, myringotomies, hysterectomies, pacemaker management and implantations, vascular stent procedures, and spine laminectomies [8]. Another report by VMG Health on ambulatory centers performing 2 million cases in 2022 cited these top outpatient procedures: gastroenterology, 32%; ophthalmology, 26%; pain management, 22%; and orthopedics, 21% [9]. The largest drivers of this trend away from hospitals include increased patient satisfaction, reduced healthcare costs, and improved productivity [10–12]. Enhanced recovery after surgery (ERAS) protocols have helped enhance patients’ experience and same-day discharge. For example, more orthopedic surgeries (total joints, minimally invasive spine surgery, and single and multi-level fusions) are being performed in the ambulatory setting [3]. As one report in 2021 estimated, patients may save about $680 USD per procedure in the ambulatory setting when compared to inpatient procedures [13]. Over the next few years, outpatient orthopedic procedures are expected to grow at 6.5% compounded annual growth rate [14].
For cardiovascular procedures, there is less movement from the inpatient to outpatient setting as a result of the patients being older, having more comorbidities, and frequently requiring admission to the hospital. The patients need complex coordinated medical care and often intensive care units, and thus are less likely to be appropriate candidates for the outpatient setting. However, certain cardiology procedures could expand to ambulatory settings (electrophysiology and other interventional cardiology procedures), if there are coordinated guidelines and procedures in place to transfer patients to a tertiary care facility should they require a higher level of care. Similarly, vascular procedures are also being performed in the outpatient setting (inferior vena cava [IVC] filter placement and peripheral vascular interventions [PVI]). Interventional radiology (IR) procedures have benefits like reduced hospital stays and costs, due to the minimally invasive nature of their procedures, with a projected growth of nearly 6.5% from 2023 to 2028 [15]. Examples of IR procedures include central venous line placements, arterial embolization, IVC filter placement, vascular interventions for fibroids and scrotal varicoceles, image-guided biopsy or drainage, image-guided approaches for cancer biopsy, treatment, and surveillance, and vertebroplasties and kyphoplasties for pain related to spinal metastases [16]. Gynecological procedures are expected to decline in the inpatient setting by nearly 30% as obstetricians and gynecologists are performing more procedures (hysteroscopies and sling procedures) in their offices [3]. Gastroenterology may be one of the fastest growing markets, with a 20% growth from 2015 to 2016 [3]. Upper endoscopies with anesthesia services represent about 7.3% of all procedures done according to one industry report [17]. Dental procedures have among the largest market share through 2023, the majority of which are performed in office-based settings [5]. Ophthalmology is growing their market by doing more procedures in the outpatient setting, with and without anesthesia services [18]. Plastic surgery has been one of the pioneers for performing outpatient procedures, and they continue to see exponential growth to the outpatient setting [19]. Urology is observing a shift in reimbursements from hospital-based procedures to office-based ones, resulting in changes in the types of procedures being performed in the office that were historically performed in ASCs or HOPDs [20].
Khandwala and Jayachandran [21] performed a small prospective feasibility study in 2012 that demonstrated that office-based sling procedures are safe and feasible. A recent retrospective analysis by Cappuccio et al. [22] from 2021 examined data from 2008 to 2015, consisting of over 41,000 patients undergoing hysterectomy for endometrial cancer. They discovered that there was a 41% shift in volume from inpatient to outpatient centers. This was associated with a cost reduction of $2,500 per hysterectomy. The authors mentioned that performing hysterectomies robotically in mid-sized hospitals were important factors associated with same-day discharge. However, patients undergoing abdominal hysterectomy or other concomitant procedures, with advanced age, of African American race, and with higher co-morbidities were more likely to be admitted.
Morgan et al. [23] studied a large retrospective analysis from 2010 to 2013 from a national data set on inpatient and outpatient hysterectomies from over 386,000 patients. The authors identified an outflow of cases to the outpatient setting, with inpatient and outpatient rates of 26.6 per 10,000 and 13.3 per 10,000 women changing to 15.4 per 10,000 and 19.6 per 10,000 women, respectively.
In 2020, a retrospective military study by Fielden et al. [24] on the benefits of office versus operating room (OR) hysteroscopy was done on 280 patients from 2015 to 2018. They compared admission time, procedure time, reimbursement, and costs for each type of hysteroscopy treatment group to develop a time-cost-benefit-value (TCBV). The TCBV was defined as any cost savings plus difference in reimbursement rates when Medicare increased office reimbursements in 2017. On average, the office had a one-hour clinic time versus 6.2 h for admission in the hospital. The average procedure time was 41%–61% shorter in the clinic versus in the OR. The authors had limited data on total actual office appointment time (57 of 235 cases) whereas they had the entire data for the OR cases (45). On average, 11% (26 of 235) of patients in the clinic could not complete the procedure. This was due to extensive pathology (16 of 235 cases), inability to tolerate the procedure (6 of 235 cases), and inability to visualize (4 of 235 cases). However, they could not track all of the direct and indirect costs of the OR and clinic and therefore were unable to calculate true TCBVs. They focused on disposable costs and labor — places that employed civilian anesthesiologists would face higher costs than active-duty staff.
Spine surgery is an incredibly lucrative procedure for spine surgeons and there is a desire to discharge patients on the same day to reduce hospital costs and hospital length of stay. However, same-day discharge for spine surgery is debatable. A 2018 large-scale retrospective case control study review by Arshi et al. [25] examined a national private insurance database from 2011 to 2016 to analyze the inpatient versus outpatient complication rates of anterior cervical discectomy and fusion (ACDF) surgeries. The authors were able to identify 770 patients who were discharged on the same day versus 26,826 patients who were admitted after surgery. They reported that outpatient ACDF was associated with a greater risk of perioperative surgical complications, including revision posterior or anterior surgery, requiring postoperative laminectomy, and a higher risk of perioperative renal failure. They assert that proper patient selection is crucial to reduce the risk of these complications. Conversely, Yerneni et al. [26] performed a retrospective meta-analysis of outpatient ACDF articles and found no statistically significant differences between inpatient and outpatient ACDF in terms of overall complications such as stroke, thrombolytic events, dysphagia, and hematoma. They report that outpatient ACDFs were more likely to have lower reoperation rates, mortality, and hospitalization duration. Their analysis was limited by the lack of high-quality evidence in the literature.
Other authors reported a reduction in costs for outpatient ACDF, an increasing shift in outpatient ACDF volume, and low likelihood of complications. Martin et al. [27] performed a retrospective review of a national insurance database of outpatient ACDF trends and costs from 2007 to 2014, demonstrating lower costs for outpatient surgery at 90 days, lower incidences of 30-day complications, and a higher morbidity for inpatient surgery. DelSole et al. reported in a 2019 meta-analysis substantial growth in spine surgery from 1994 through 2016 [28]. Their data reflected low likelihood of complications after same-day discharge. A 2020 retrospective review of Medicare patients undergoing ACDF identified 264,000 surgeries from 2012 to 2017 [29]. Their data demonstrated a significant increase of 185% in ASC ACDF volume from 2015 to 2017.
A common urology procedure typically performed in the hospital is the ureteral (JJ) stent placement. There is a push in urology to move some of these stent placements in the clinic for the right patient. In 2019, Doersch et al. [30] examined clinic versus OR ureteral (JJ) stent placements (under nitrous oxide and/or local anesthesia [LA] versus general anesthesia [GA], respectively) in New York. Outcomes compared were complications, unanticipated hospitalizations, and stent failures. Overall, there were low complication rates (unanticipated hospitalizations or stent failures) — 4.1% in the clinic setting versus 7.9% in the OR setting. The authors could not find any identifiable risk factors that affected the complication rates; the clinic versus OR setting was not predictive of complications.
Another type of office procedure is the magnetic resonance imaging prostate partial gland cryoablation. A 2020 feasibility study by Basourakos et al. [31] examined patients who underwent this procedure under LA. The authors found adequate outcomes of cancer remission without an increase in urinary or sexual function compared to the baseline. Additionally, in-office costs were significantly lower than when doing the procedure under GA in the OR at an ASC ($4,400 versus $8,400). While disposable costs for both in-office and OR procedures were similar ($3,086), the fixed costs for in-office procedures were $305 while for OR procedures ranged from $1,859 to $6,049. The larger fixed costs for the OR were from driven from the need to perform the procedure under GA and longer operative times (90–150 min versus 16–58 min).
For women undergoing complex female pelvic floor reconstruction surgery, Dutta et al. [32] created in 2020 an ERAS protocol for same-day discharge and studied whether this would result in a reduction in hospital resources without compromising patient safety outcomes. Their ERAS protocol involved pre-operative hydration, urinary analgesia, non-narcotic analgesia, involvement of the family, and communication. The authors found no differences in demographics, operative details, complications, overall revenues or expenses, emergency room visits, or unexpected clinic visits when comparing pre-ERAS protocol versus post-ERAS protocol. They did find a significant difference in the bed-unit cost ($210 versus $533) and the amount of prescribed narcotics in favor of the post-ERAS group. The post-ERAS group did have significantly more patients undergo the procedure in an ambulatory setting (73.6% versus 48.8%) and who were discharged on the same day (80.2% versus 50%).
Partial nephrectomies are moving towards a same-day discharge. Wood et al. [33] conducted a retrospective analysis over six years from 2015 to 2021 comparing a before and after implementation of a same-day discharge protocol for partial nephrectomy. On a before and after same-day discharge protocol comparison, their study found 78% of post-anesthesia care unit (PACU) patients were discharged on the same day compared to 0%, had similar safety profile, and no difference in readmission rates, but same-day discharge patients were more likely to return to the office for an unplanned visit (17.8% versus 6.8%). On a cost basis, same-day discharge patients incurred higher costs from the lengthier PACU stay by $1,622 per patient; on the other hand, total healthcare costs were lower for same-day discharge patients ($5,222 versus $8,425 per patient).
Vascular surgery outpatient procedures have also increased while inpatient services have declined. Jones et al. [34] examined cases from 2006 to 2011, demonstrating a significant shift of PVI to the outpatient setting. The authors identified nearly 40,000 Medicare patients and found that there was a large reduction in the rate of PVIs in the hospital: 209.7 to 151.6 per 100,000 beneficiaries. Meanwhile outpatient hospitals and office-based laboratories (OBLs) saw a huge increase: 184.7 to 228.5 per 100,000 beneficiaries and 6 to 37.8 per 100,000 beneficiaries, respectively.
Looking at the trends of ambulatory shifts, Schramm et al. [35] reviewed Medicare claims from 2011 to 2017 for PVI, demonstrating a large increase in office-based billing and steep decreases in hospital inpatient and outpatient billing. Over this time period, the largest proceduralist growth was in the radiology group versus cardiology or vascular surgery. Overall, all OBL claims sent in by surgery, cardiology, and radiology showed significant advancement during this time. Another report by Smith et al. [36] reviewed Medicare payments from 2013 to 2015 for vascular procedures (atherectomy, diagnostic angiography, stent placement, and percutaneous transluminal angioplasty) and found a 64% increase of procedure in office volume. A more recent study by Mukherjee et al. [37] surveying cases from 2011 to 2014 demonstrated a 60% increase in outpatient PVI, with office procedures increasing by as much as 298%.
An examination of 6,200 procedures on nearly 2,800 patients from 2011 to 2015 by Aurshina et al. [38] found that low risk patients were able to safely undergo minimally invasive, noncomplex vascular procedures with low risk for morbidity and mortality. The authors looked at procedures performed at an OBL. The majority of their patients were ASA PS I and II. They found no patients with any deaths, major bleeding, myocardial infarction, or stroke within 72 h of the procedure. A study in 2016 by Alsheekh et al. [39] reported that vascular surgeons were safely able to place IVC filters in patients in their offices.
IR procedures are also moving into the outpatient arena. Wang et al. [40] investigated the cost of endovascular intervention versus hysterectomy to treat uterine leiomyoma along with hospital length of stay. The authors examined outpatient data from over 227,000 patients from California (2005–2011) and Florida (2005–2014). They compared three groups: hysterectomy, myomectomy, and uterine artery embolization (UAE) for treatment of uterine leiomyoma. Patients who received a hysterectomy had slightly longer mean length of stay versus the other two treatment groups. The cost of an UAE was significantly cheaper, $3,772, versus hysterectomy, $5,409, and versus myomectomy, $6,318. Their study found that 75% of the patients undergoing an UAE were discharged on the same day versus 55% of the patients undergoing hysterectomy.
Ahn et al. [41] published a 2017 case series on 5,134 outpatients who underwent endovascular procedures. They examined the first 5,134 consecutive patients in the office from 2006 to 2013 to assess for complication and success rates. The five types of procedures in descending order of proportion were venous interventions, arterial interventions, diagnostic angiograms, dialysis access interventions, and venous catheter management. There were low complication rates: 1%, 1.5%, 3%, 1.1%, and 0.7%, respectively. Nine patients out of 5,134 died within 30 days of their procedure but were not deemed to be procedure-related.
Offices may provide improved patient satisfaction as there can be reduced delays for IR procedures. In 2020, Hickey et al. [42] studied the impact of an OBL versus hospital setting on procedure start delays. They looked at 176 mapping and treatment angiograms from 2019 to 2020. There were no differences in mapping or treatment angiograms between each site. There were longer start delays in the hospital versus the office (28.6 min versus 0.8 min). Procedures also took longer on average in the hospital versus the office (2 h, 1.8 min versus 1 h, 44 min). It follows that patients would have higher satisfaction since there were less delays and shorter procedure duration. Additionally, there were cost savings associated with office-based procedures as more of the procedure payment stays with the radiology practice rather than going towards the hospital facility fee.
Patient safety in dental offices has been wrought with controversy in the past. Specifically, pediatric deaths in dental offices from 1980 to 2011 were reported on by Lee et al. [43]. There were 44 deaths: two in ages 0–23 months, 21 in ages 2–5 years, eight in ages 6–12, 13 in ages 13–21 years, and. The type of anesthesia used was reported with the fatalities: 20 in a setting of moderate sedation, 10 in a setting of GA, 10 were not reported, and 4four with LA. The type of anesthesia provider was also reported- 25 deaths were in the setting of a pediatric/general dentist, 8 with an oral surgeon, 7 with anesthesia, and 4 were not reported. The procedure location was labeled with the fatalities: 31 deaths occurred in offices, six in hospital, and seven were not reported. However, a recent report by Gaiser et al. [44] examining online versus PubMed (https://pubmed.ncbi.nlm.nih.gov/, United States National Library of Medicine) published deaths in dental offices found that there may be an undercounting of deaths as well as underestimation of the risks from sedation and GA. More reported deaths under the age of 18 were seen in the non-expert online articles versus PubMed.
Within the adult world in the military health system, dental adverse event trends were examined by Stahl et al. [45]. They looked retrospectively from 2013 to 2016 and found a 32% increase in events in dentistry. Additionally, dental adverse outcomes were the highest compared to other specialties (32.7%). Of the adverse events, wrong-sided surgeries (WSS) and intraoperative/post-operative anesthesia or surgery issues were the highest fraction sentinel events (63% and 14%, respectively). Within WSS, wrong-sided anesthesia and wrong-tooth surgery comprised the largest percentages of events (40% and 32%, respectively). The dataset did not track total procedures, so no incidence rates were calculated. Root cause analyses (RCAs) performed afterwards found communication failure and inconsistent use of the universal protocol to be the leading reasons for WSSs.
A survey was conducted by Viswanath et al. [46] of 120 oral maxillofacial surgeons (OMFS) on ambulatory checklist adoption and malpractice claims in 2018. They found that 42% of respondents did not use a checklist in ambulatory surgery; even 45% of OMFS performing more than 30 procedures a week were not using a checklist. Up to 17% of OMFS nationally report at least one malpractice claim [47]. The authors concluded that OMFS should adopt ambulatory checklists more universally as well as conduct more research in this area.
A recent 2022 survey of American Association of Pediatric Dental program directors found that more than two-thirds of the program directors felt that there was a lack in safety knowledge and information among residents [48]. A limited number of program directors were familiar with tools associated with safety, such as RCA and situation-background-assessment-recommendation.
A recent retrospective study on office ear, nose, and throat (ENT) procedures was undertaken by Benito et al. [49] They examined sialendoscopies in the office versus sialithotomies in the OR from 2011 to 2016. The authors found similar demographics, sialolith numbers, and sizes. There were similar symptom improvement as well as recurrence rates. However, within the office they found a significantly shorter duration of procedure compared to the OR (39 min versus 277 min). Additionally, there was a significant reduction in procedure and hospital charges ($719 versus $13,950).
Another study by Mastrolonardo et al. [50] examined the types of anesthesia for OR sialendoscopies from 2017 to 2019. They found that when doing the procedure with monitored anesthesia care compared to GA, there was a decreased median hospital time (141 min), anesthesia time (46 min), operative time (24 min), time in the OR (43 min), and recovery time (56 min). There were no differences in the rates of symptom resolution, complications, and repeat medical or surgical interventions.
A contemporary review by Schimberg et al. [51] of laryngopharyngeal surgery cost comparison between the office and the OR was published in 2019. They found 13 studies to include, all of which described lower costs in the office, nearly 95% reduction per procedure. The types of surgeries included laser surgery, biopsy, vocal fold injection, or esophageal dilation. The lowest cost was associated with LA instead of procedures performed with an anesthesiologist. The added benefit was that the patients can often return to work the same day. The authors noted vast differences between charges that hospitals submitted for billing and the actual costs of the procedure, as well as wide variation on total costs per procedure. There appeared to be a lack of transparency with regards to this information within and across the healthcare systems internationally.
A retrospective cohort analysis conducted by Stagg et al. [18] of 531,000 ophthalmologic surgeries from 2001 to 2014 in the US reported that outpatient cataract surgery increased from 43.6% in 2001 to 73% in 2014. Current literature also shows reports that commonly performed ophthalmology procedures are also trending toward the office setting. As of 2019, office procedures are safe, more financially viable, and may offer more convenience for the proceduralists and better patient satisfaction [52].
Gastrointestinal (GI) procedures have served as one of the pioneers for procedures performed in the outpatient setting. Predmore et al. [53] reported Medicare data with respect to ASA PS I and II patients who received anesthesia for GI procedures. From 2010 to 2013, 6.6 million GI outpatient procedures showed an increase in the use of anesthesia from 33.7% to 47.6% among Medicare patients and 38.3% to 53% among private insurance patients. Another report by Adams et al. [54] demonstrated substantial growth of anesthesia services for GI procedures performed at the Veterans Administration hospital from 2000 to 2013. Similarly, a retrospective analysis by Eberth et al. [55] on the trend of gastroenterology procedures reported a substantial shift from hospitals to ASCs from 2001 to 2010.
A major part of the shift towards outpatient gastroenterology cases is due to a reduction in healthcare costs. Blue Cross Blue Shield insurance-approved charges are shown in Fig. 1. Office-based procedures provided significant cost savings to the healthcare system. For a typical GI procedure, the reimbursement to the hospital or HOPD was $2,753, to the ASC was $2,277, and to the office was $1,678.
Plastic surgery is another pioneer in outpatient and office-based procedures. Ballard et al. [56] reported in 2019 that the majority of breast surgery augmentation procedures were performed in freestanding outpatient (47%) and office (34%) centers from 2011 to 2015. The authors also reported a low rate of adverse events (7%) and reoperation rates (2%). Another retrospective analysis from 2011 to 2018 of aesthetic plastic surgery conducted by Khetpal et al. [19] also demonstrated the consistent trend of significant increases in breast reduction and abdominoplasty cases seen in the ASC.
Supporting the trend of plastic surgery cases being performed in the office, Osman and Shapiro [57] reported in their review that there were 72% of 17.5 million aesthetic procedures being done in the office-based setting annually. A common surgical technique is the use of tumescent lidocaine that has a somewhat large safety margin; however, fat embolism is a concern and has been associated with deaths [58]. A 2017 survey of plastic surgeons by Mofid et al. [59] found that out of 198,857 cases of gluteal fat grafting, there were 32 fatalities and 103 nonfatal pulmonary emboli. There may be a higher mortality incidence associated with gluteal fat grafting than with other cosmetic procedures.
A 2018 retrospective analysis was conducted by McLaughlin et al. [60] of 76,000 patients who underwent partial or total thyroidectomy from 2005 to 2014. They uncovered a steady increase in patients undergoing outpatient surgery annually with a relatively low risk of complications. When comparing outpatient versus inpatient thyroid surgery, there are cost savings associated with outpatient surgery, decreased hospital length of stay, and increased patient satisfaction [61]. Proper patient selection was key to the success of creating and maintaining an outpatient program. The authors identified important contraindications to outpatient thyroid surgery that include complex medical problems, anticipated difficult surgical dissection, anticoagulated patients, lack of home support, and patient anxiety about same-day discharge. This, in turn, was used to develop a protocol to improve patient safety and satisfaction. In 2021, Rosen et al. [62] performed a retrospective analysis in Alabama analyzing outpatient versus inpatient thyroid surgery and associated costs and outcomes from 2011 to 2017. Of 870 isolated total thyroidectomies, 42% were outpatient surgeries and there were no significant differences in complications between the two groups. The outpatient group had average cost savings of $2,300 per patient compared to the inpatient group.
Most surgical procedures require the use of anesthesia services regardless of the location of the procedures being performed. As surgical procedures migrate from inpatient hospitals to outpatient centers and offices, anesthesia providers must follow suit. Mobile anesthesia is a relatively new concept that provides services to office-based surgery sites [63]. This concept brings the OR to the office and the patient. For instance, a medium sized mid-west anesthesia practice specializing in mobile anesthesia, called Mobile, provides offices with anesthesiologists and pre- and post-procedure nurses. They transport portable anesthesia machines with all of the ASA standard monitoring equipment, airway management supplies, anesthesia medications, emergency medications for advanced cardiopulmonary life support and malignant hyperthermia (MH), pediatric-related equipment, and anesthesia electronic medical record (EMR) documentation. Examples of specialties that perform procedures in the office include ENT, gastroenterology, pain medicine, gynecology, urology, dentistry, vascular surgery, orthopedic surgery, podiatry, and plastic surgery (Table 1).
A large retrospective analysis of nearly 90,000 cases from 2016 to 2019 from a mobile anesthesia practice in New York was conducted by Shapiro et al. [63]. This practice staffed both ASC and OBS sites. Their four-year EMR data reflected a steady increase in OBS cases and an exponential growth in ASC volume. The top five procedures in the ASC were cataract removal, lumbar epidural steroid injections, shoulder arthroscopy, knee arthroscopy, and lumbar disc decompression (Table 2). The top five procedures in the OBS were colonoscopy, prostate biopsy, angioplasty, urethrocystoscopy, and uterine fibroid embolization. The case mix was widely different between the two, almost exclusive of each other. OBS had slightly older group of patients and slightly higher classification with patients considered ASA III or greater. Overall complications in the OBS were zero in 89% of cases versus 83% of ASC cases, which was a significant difference. Major complications were rare and there was no significant difference between OBS and ASC sites. OBS had significantly fewer minor complications compared to ASCs. There was a low incidence of overall complications observed in the OBS procedures.
As demonstrated above, the scope of procedures being performed in the outpatient setting is becoming more complex. This, in turn, brings with it a patient population with more complicated medical issues. Just as cardiovascular risk factors and atherosclerotic cardiovascular disease have increased over time, Smilowitz et al. [64] assert that one can only assume the same for the outpatient population. While examining a US inpatient study sample from 2004 to 2013, the authors found that patients with more than two cardiovascular risk factors increased from 40% to 48%, the percent of patients with coronary artery disease increased from 17% to 18% over this time period, peripheral vascular disease increased from 6.3% to 7.4%, and patients with a reported prior stroke increased from 3.5% to 4.7%, respectively.
A 2021 study by Hajmohamed et al. [65] reported a changing landscape in outpatient surgery with regard to morbid obesity and surgical complications. They conducted a retrospective analysis examining 7,100 patients from 2017 to 2018, reporting that a similar proportion of patients from each group had to be readmitted within three days (0.48% versus 0.46%). After multivariate analysis in which the body mass index (BMI) was evaluated as a continuous variable, a BMI of 40 + was not associated with medical complications, surgical complications, or readmissions. The authors state that there is insufficient evidence regarding postoperative complications in these patients undergoing GA for outpatient surgery.
The effect of increased BMI can be seen in anesthesia-related closed claims. A retrospective analysis by Ranum et al. [66] from 2007 to 2014 of nearly 1,000 closed claims at ASCs and hospitals found that 19% of ASC claims and 33% of hospital claims were high severity injuries. High severity included injuries like loss of one or two limbs, brain damage, paraplegia or quadriplegia, or severe brain damage, death, or lifelong care. The four top injury claims were dental injuries, perioperative pain, nerve damage, and death. While no comorbidity was implicated in the vast majority of the claims (71% and 65% for ASC and hospital, respectively), obesity (13% and 20% for ASC and hospital, respectively) was the most common comorbidity that impacted both ASC and hospital closed claims.
Patients with high BMI are also at high risk for obstructive sleep apnea (OSA) and are at increased jeopardy of suffering postoperative complications after receiving sedation or postoperative analgesia. Goldberg et al. [67] used the validated STOP-BANG (Snoring history, Tired during the day, Observed stop breathing while asleep, high blood Pressure, BMI more than 35 kg/m2, Age more than 50 years, Neck circumference more than 40 cm, and male Gender) questionnaire to evaluate their patient population who required intravenous (IV) anesthesia or sedation for risk of OSA. Of the 153 patients, 12 (8%) were at moderate to high risk of OSA. With this new data, they changed the sedation plan for four patients due to the elevated OSA risk.
Bongiovanni et al. [68] appreciated the change of the overall health and cormorbidities in patients undergoing outpatient procedures and performed an analysis of over a 1.2 million ambulatory surgeries in California taking place from 2009 to 2011. The authors analyzed the rate of 30-day unplanned hospital visits, emergency room visits, and hospital admissions. The data showed that the risk of unplanned hospital visits was 4.8%, ER visit was 3.1%, and hospital admission was 1.7%. The independent risk factors included increasing age, increasing comorbidities, location of procedure, and type of surgery. Cardiovascular and urological procedures had the highest rate of unplanned hospital visits at 30 days.
Rajan et al. [7] performed a 2021 review of patient selection in ambulatory surgery and assert that many factors need to be considered in patient selection. This includes the type of procedure being performed, type of facility (hospital versus free-standing versus office), patient medical history, social history and non-medical factors, and the type of anesthesia being administered. Facility type and procedure type are important to consider because the facility may not be able to offer higher acuity services such as lab or blood bank services, expert consultation for the care of sicker patients, or formal transfer policies and procedures in the case of an emergency. The authors provide some recommendations for proper patient selection: ASA III patients who are stable, ASA IV patients who are stable undergoing low-risk procedures, graded consideration for obesity, screening for and optimizing patients with sleep apnea, asymptomatic cardiac patients who do not require testing, excluding patients with severe chronic obstructive pulmonary disease, excluding patients with end-stage renal disease not on dialysis, and ensuring that there is MH treatment cart and non-triggering agents if caring for patients with MH.
The use of regional anesthesia in ambulatory surgery provides clear benefits to the patient including lower pain scores, reduced narcotic pain medicine usage, shorter recovery times, and decreased hospital length of stays. Gabriel and Ilfeld [69] identified nearly 13 million ambulatory surgeries from 2010 to 2015 from the National Anesthesia Clinical Outcomes Registry (NACOR) that demonstrated that the employment of peripheral nerve blocks has rapidly increased over time. Uncontrolled pain can prevent timely discharge after recovery or even result in an unplanned hospital admission. Pavlin et al. [70] reported that high pain scores can lead to higher and more frequent doses of narcotics in recovery, increased risk of PONV, and a resultant delay in discharge. The authors stated that pain scores had a positive predictive effect on recovery times, with increasing times with increasing pain scores. Patients who received LA and ketorolac were less likely to have high pain scores, and patients received less fentanyl if they also received ketorolac intraoperatively.
In recent years the influence of pain on PACU stay and hospital length of stay has been confirmed with other types of surgeries that incorporate ERAS protocols, like non-opioid analgesics, dexamethasone, and regional anesthesia. Non-opioid analgesics like acetaminophen, non-steroidal anti-inflammatory drugs (NSAIDs), ketamine, and dexmedetomidine have consistently positive effects on pain control and reducing hospital length of stay [71–74]. Dexamethasone has been shown to reduce pain as well as nausea incidence [75]. Use of regional anesthesia has good evidence to reduce pain scores, nausea and vomiting rates, and PACU length of stay [76]. High pain scores after breast surgery have been associated with higher rates of post-discharge nausea and vomiting that Stjernberg et al. [77] thought was due to higher opioid consumption.
A 2016 retrospective study by Herzig et al. [78] analyzed adverse events among Medicare beneficiaries who were discharged with opioids versus NSAIDs (13,385 versus 4,677) and found that there were significantly more morbidity and mortality within 30 days of discharge. Specifically, among opioid users, there were significantly higher rates of death (1.8% versus 1.1%), healthcare utilization (19% versus 17.4%), and any potential adverse event (25.2% versus 21.3%) — higher relative risk [RR] of a fracture or fall (4.5% versus 3.4%, RR) 1.3), nausea or vomiting (9.2% versus 7.3%, RR 1.3), and constipation (8% versus 6.2%, RR 1.3). There were no differences in the risk of delirium, acute kidney injury, or gastritis.
The landscape of surgical and noninvasive procedures being performed has been evolving and shifting over the last quarter century. Anesthesiologists are constantly being challenged to maintain patient safety commensurate with this exponential growth. The literature supports the trend of higher ASA PS scored patients and more complicated procedures shifting towards the outpatient arena (i.e., ASCs and offices). Several reasons that may account for these include cost incentives (for patients and healthcare systems), advancement in anesthesia techniques, ERAS protocols, and increased patient satisfaction. Recently published literature shows positive patient outcomes or no difference in complication rates for patients to have same-day discharge procedures versus hospital admissions, but the appropriate patient and procedure has to be selected [4]. Additionally, the use of checklists and accreditation status of the surgical office plays an important impact on patient safety [79]. Anesthesiologists must understand that there is a lack of standardized state regulations regarding ASCs and OBSs. As of 2022, there is still wide variation per the Federation of State Medical Boards: 17 do not regulate OBS centers [80]. The next generation of anesthesiologists, as well as currently practicing anesthesiologists, should be aware of the safety concerns related to the various locations (HOPD, ASC, and OBS), the sustained growth and demand for anesthesia in the office, and the expansion of mobile anesthesia practices around the US in order to keep up and practice safely with the professional trends [81]. A critical factor to ensuring safety with the continued migration of procedures from the hospital to the outpatient and office-based setting is to establish a culture of safety. Multidisciplinary teams can come together, such as the Cincinnati Children’s Hospital’s endeavor to bring pediatric anesthesiologists to the dental clinics. Their goal was to improve patient outcomes and access to in-office GA for dental procedures without increasing adverse events [82]. They increased the number of successful case completions, complete radiographs, and reduced the number of failed sedations.
Continuing growth trends will require ongoing research regarding patient safety, satisfaction, and outcomes, and efficiency costs between outpatient and inpatient procedures. Does the cost of the limited number of complications and readmissions outweigh the benefits of the shift from the inpatient to outpatient setting? Are we educating the next generation of anesthesiologists about the necessary safety measures when providing anesthesia in the varied non-hospital-based locations? Additional research outcomes, likely prospective in nature, must be performed on these novel outpatient procedures, to develop risk stratification and prediction models for the selection of the proper patient, procedure, and location, in order to ensure safety in anesthesia practice.
Fig. 1.
Average Blue Cross Blue Shield approved charges (USD) for a typical GI procedure by site. USD: United States dollar, GI: gastroenterology.
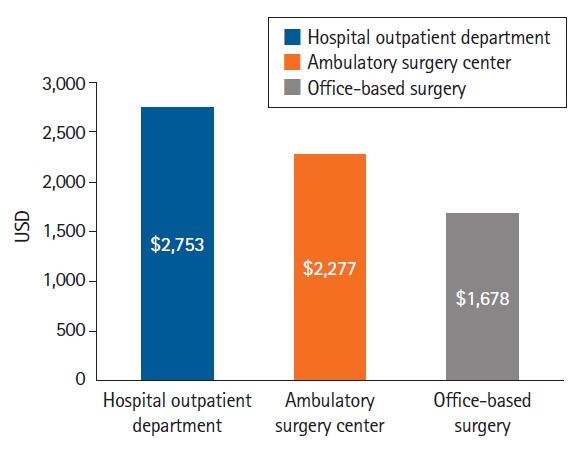
Table 1.
Examples of Procedures Done in the Office in the Mid-west USA
Table 2.
Top Procedures from a Mobile Anesthesia Practice
References
1. AORN. Growth in ambulatory surgery centers in U.S. continues upward trend - outpatient surgery magazine [Internet]. Denver (CO): Outpatient Surgery Magazine; 2022 June 21 [cited 2023 Feb 1]. Available from https://www.aorn.org/outpatient-surgery/article/2022-Q1-growth-centers
2. Hollenbeck BK, Dunn RL, Suskind AM, Zhang Y, Hollingsworth JM, Birkmeyer JD. Ambulatory surgery centers and outpatient procedure use among Medicare beneficiaries. Med Care 2014; 52: 926-31.



3. Dyrda L. 10 key trends for ASCs and outpatient surgery in the next 10 years [Internet]. Chicago (IL): Becker’s ASC Review; 2018 Apr 2 [cited 2023 Feb 1]. Available from https://www.beckersasc.com/asc-news/10-key-trends-for-ascs-and-outpatient-surgery-in-the-next-10-years.html
4. Young S, Shapiro FE, Urman RD. Office-based surgery and patient outcomes. Curr Opin Anaesthesiol 2018; 31: 707-12.


5. US outpatient surgical procedures market by surgical procedure type, patient care setting - US forecast to 2023 [Internet]. Dublin: Research and Markets; 2019 Jan [cited 2023 Feb 1]. Available from https://www.researchandmarkets.com/reports/4746620/us-outpatient-surgical-procedures-market-by
6. Jani SR, Shapiro FE, Gabriel RA, Kordylewski H, Dutton RP, Urman RD. A comparison between office and other ambulatory practices: analysis from the National Anesthesia Clinical Outcomes Registry. J Healthc Risk Manag 2016; 35: 38-47.

7. Rajan N, Rosero EB, Joshi GP. Patient selection for adult ambulatory surgery: a narrative review. Anesth Analg 2021; 133: 1415-30.


8. Karaca Z, McDermott KW. High-volume invasive, therapeutic ambulatory surgeries performed in hospital-owned facilities, 2016. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality; 2019 Sep 18 [updated 2020 Sep 21; cited 2023 Feb 1]. Available from https://hcup-us.ahrq.gov/reports/statbriefs/sb252-Invasive-Ambulatory-Surgeries-2016.pdf
9. Newitt P. 100+ stats on ASCs [Internet]. Chicago (IL): Becker’s ASC Review; 2022 Apr 8 [cited 2023 Feb 1]. Available from https://www.beckersasc.com/asc-news/100-stats-on-ascs.html
10. O’Donnell EA, Fury MS, Maier SP 2nd, Bernstein DN, Carrier RE, Warner JJ. Outpatient shoulder arthroplasty patient selection, patient experience, and cost analyses: a systematic review. JBJS Rev 2021; 9: e20.00235.

11. Ferrari D, Lopes TJ, França PF, Azevedo FM, Pappas E. Outpatient versus inpatient anterior cruciate ligament reconstruction: a systematic review with meta-analysis. Knee 2017; 24: 197-206.


12. Mullins J, Pojskić M, Boop FA, Arnautović KI. Retrospective single-surgeon study of 1123 consecutive cases of anterior cervical discectomy and fusion: a comparison of clinical outcome parameters, complication rates, and costs between outpatient and inpatient surgery groups, with a literature review. J Neurosurg Spine 2018; 28: 630-41.


13. Shifting common outpatient procedures to ASCs can save consumers more than $680 per procedure [Internet]. Minneapolis (MN): UnitedHealth Group. 2021 Sept [cited 2023 Feb 1]. Available from https://www.unitedhealthgroup.com/content/dam/UHG/PDF/2021/Site-of-Service-Research-Brief.pdf
14. Condon A. 3 key trends driving ASC market growth [Internet]. Chicago (IL): Becker’s ASC Review; 2021 Oct 7 [cited 2023 Feb 1]. Available from https://www.beckersasc.com/asc-news/3-key-trends-driving-asc-market-growth.html
15. Interventional radiology market - growth, trends, COVID-19 impact, and forecasts (2023-2028) [Internet]. Hyderabad: Mordor Intelligence; 2023 [cited 2023 Feb 1]. Available from https://www.mordorintelligence.com/industry-reports/interventional-radiology-market
16. Arnold MJ, Keung JJ, McCarragher B. Interventional radiology: indications and best practices. Am Fam Physician 2019; 99: 547-56.

17. Definitive Healthcare. Top 20 anesthesia procedures and services [Internet]. Framingham (MA): Definitive Healthcare; 2022 Oct 19 [cited 2023 Feb 1]. Available from https://www.definitivehc.com/resources/healthcare-insights/top-anesthesia-procedures-services
18. Stagg BC, Talwar N, Mattox C, Lee PP, Stein JD. Trends in use of ambulatory surgery centers for cataract surgery in the United States, 2001-2014. JAMA Ophthalmol 2018; 136: 53-60.



19. Khetpal S, Lopez J, Prsic A. Trends in the use of ambulatory surgery centers for medically necessary aesthetic plastic surgery procedures among Medicare beneficiaries. Plast Reconstr Surg 2021; 147: e916-8.

20. Henry MA, Howard DH, Davies BJ, Filson CP. Physician reimbursement for prostate biopsies falls as procedures shift from offices to facilities. Urology 2018; 115: 96-101.


21. Khandwala S, Jayachandran C. TVT-secur in office sling procedure under local anesthesia: a prospective 2-year analysis. Female Pelvic Med Reconstr Surg 2012; 18: 233-8.


22. Cappuccio S, Li Y, Song C, Liu E, Glaser G, Casarin J, et al. The shift from inpatient to outpatient hysterectomy for endometrial cancer in the United States: trends, enabling factors, cost, and safety. Int J Gynecol Cancer 2021; 31: 686-93.


23. Morgan DM, Kamdar NS, Swenson CW, Kobernik EK, Sammarco AG, Nallamothu B. Nationwide trends in the utilization of and payments for hysterectomy in the United States among commercially insured women. Am J Obstet Gynecol 2018; 218: 425.e1-18.



24. Fielden AD, Braden JM, Brooks D, Dunlow SG, Lockrow EG, Endicott S. Evaluating the impact of office hysteroscopy in a military treatment facility. Mil Med 2020; 185: e1686-92.



25. Arshi A, Wang C, Park HY, Blumstein GW, Buser Z, Wang JC, et al. Ambulatory anterior cervical discectomy and fusion is associated with a higher risk of revision surgery and perioperative complications: an analysis of a large nationwide database. Spine J 2018; 18: 1180-7.



26. Yerneni K, Burke JF, Chunduru P, Molinaro AM, Riew KD, Traynelis VC, et al. Safety of outpatient anterior cervical discectomy and fusion: a systematic review and meta-analysis. Neurosurgery 2020; 86: 30-45.



27. Martin CT, D’Oro A, Buser Z, Youssef JA, Park JB, Meisel HJ, et al. Trends and costs of anterior cervical discectomy and fusion: a comparison of inpatient and outpatient procedures. Iowa Orthop J 2018; 38: 167-76.


28. DelSole EM, Makanji HS, Kurd MF. Current trends in ambulatory spine surgery: a systematic review. J Spine Surg 2019; 5(Suppl 2): S124-32.



29. Lopez CD, Boddapati V, Lombardi JM, Sardar ZM, Dyrszka MD, Lehman RA, et al. Recent trends in medicare utilization and reimbursement for anterior cervical discectomy and fusion. Spine J 2020; 20: 1737-43.


30. Doersch KM, Thai KH, Machen GL, Bird ET, Reilly TP, el Tayeb MM. A comparison of clinical outcomes of operating room versus office-based ureteral stenting with the novel use of nitrous oxide sedation. Urology 2019; 132: 37-42.


31. Basourakos SP, al Hussein Al Awamlh B, Bianco FJ, Patel NA, Laviana A, Margolis DJ, et al. Feasibility of in-office MRI-targeted partial gland cryoablation for prostate cancer: an IDEAL stage 2A study. BMJ Surg Interv Health Technol 2020; 2: e000056.



32. Dutta R, Xu R, Cui T, Bubnov AS, Matthews CA. Safety and economics of an enhanced recovery after surgery protocol in pelvic reconstructive surgery. Int Urogynecol J 2022; 33: 1875-80.




33. Wood A, Jivanji D, Kaplan-Marans E, Katlowitz E, Lubin M, Teper E, et al. Same-Day discharge after robot-assisted partial nephrectomy: is it worth it? J Endourol 2023; 37: 297-303.


34. Jones WS, Mi X, Qualls LG, Vemulapalli S, Peterson ED, Patel MR, et al. Trends in settings for peripheral vascular intervention and the effect of changes in the outpatient prospective payment system. J Am Coll Cardiol 2015; 65: 920-7.


35. Schramm KM, Dewitt PE, Dybul S, Rochon PJ, Patel P, Hieb RA, et al. Recent trends in clinical setting and provider specialty for endovascular peripheral artery disease interventions for the Medicare population. J Vasc Interv Radiol 2020; 31: 614-21.e2.


36. Smith ME, Sutzko DC, Beck AW, Osborne NH. Provider trends in atherectomy volume between office-based laboratories and traditional facilities. Ann Vasc Surg 2019; 58: 83-90.


37. Mukherjee D, Hashemi H, Contos B. The disproportionate growth of office-based atherectomy. J Vasc Surg 2017; 65: 495-500.


38. Aurshina A, Ostrozhynskyy Y, Alsheekh A, Kibrik P, Chait J, Marks N, et al. Safety of vascular interventions performed in an office-based laboratory in patients with low/moderate procedural risk. J Vasc Surg 2021; 73: 1298-303.


39. Alsheekh A, Hingorani A, Marks N, Ascher E. The next frontier of office-based inferior vena cava filter placement. J Vasc Surg Venous Lymphat Disord 2016; 4: 283-5.


40. Wang C, Kuban JD, Lee SR, Yevich S, Metwalli Z, McCarthy CJ, et al. Utilization of endovascular and surgical treatments for symptomatic uterine leiomyomas: a population health perspective. J Vasc Interv Radiol 2020; 31: 1552-9.e1.


41. Lin PH, Yang KH, Kollmeyer KR, Uceda PV, Ferrara CA, Feldtman RW, et al. Treatment outcomes and lessons learned from 5134 cases of outpatient office-based endovascular procedures in a vascular surgical practice. Vascular 2017; 25: 115-22.



42. Hickey RM, Maslowski JM, Aaltonen ET, Horn JC, Patel A, Sista AK, et al. Yttrium-90 radioembolization in the office-based lab. J Vasc Interv Radiol 2020; 31: 1442-8.


43. Lee HH, Milgrom P, Starks H, Burke W. Trends in death associated with pediatric dental sedation and general anesthesia. Paediatr Anaesth 2013; 23: 741-6.



44. Gaiser M, Kirsch J, Mutzbauer TS. Using nonexpert online reports to enhance expert knowledge about causes of death in dental offices reported in scientific publications: qualitative and quantitative content analysis and search engine analysis. J Med Internet Res 2020; 22: e15304.



45. Stahl JM, Mack K, Cebula S, Gillingham BL. Dental patient safety in the military health system: joining medicine in the journey to high reliability. Mil Med 2020; 185: e262-8.



46. Viswanath A, Balint A, Johnson RE 3rd, Rosenberg MB, Oreadi D. Surgical safety checklists are underutilized in ambulatory oral and maxillofacial surgery. J Oral Maxillofac Surg 2018; 76: 267-72.


47. Holmes SM, Udey DK. Risk management in oral and maxillofacial surgery. Oral Maxillofac Surg Clin North Am 2008; 20: 119-26.


48. Boynton JR, Amini H, Claman DB, Hammersmith KJ, Peng J, McDaniel JC, et al. Safety training in US pediatric dentistry advanced education programs: a survey of program directors. Pediatr Dent 2022; 44: 198-206.

49. Benito DA, Shaver TB, Cox R, Strum DP, Mehta V, Shim T, et al. Cost-analysis of in-office versus operating room sialendoscopy: comparison of cost burden and outcomes. Am J Otolaryngol 2022; 43: 103424.


50. Mastrolonardo E, Stewart M, Alapati R, Thaler A, Zhan T, Curry JM, et al. Comparison of general anesthesia and monitored anesthesia care for sialendoscopy procedures. Am J Otolaryngol 2021; 42: 102809.


51. Schimberg AS, Wellenstein DJ, van den Broek EM, Honings J, van den Hoogen FJA, Marres HAM, et al. Office-based vs. operating room-performed laryngopharyngeal surgery: a review of cost differences. Eur Arch Otorhinolaryngol 2019; 276: 2963-73.




52. Durrie DS. Office-based cataract surgery may be next major trend in ophthalmology [Internet]. ThorofareHealio (NJ): Healio; 2019 Sep 4 [cited 2023 Feb 1]. Available from https://www.healio.com/news/ophthalmology/20190822/officebased-cataract-surgery-may-be-next-major-trend-in-ophthalmology
53. Predmore Z, Nie X, Main R, Mattke S, Liu H. Anesthesia service use during outpatient gastroenterology procedures continued to increase from 2010 to 2013 and potentially discretionary spending remained high. Am J Gastroenterol 2017; 112: 297-302.



54. Adams MA, Prenovost KM, Dominitz JA, Kerr EA, Krein SL, Saini SD, et al. National trends in use of monitored anesthesia care for outpatient gastrointestinal endoscopy in the veterans health administration. JAMA Intern Med 2017; 177: 436-8.



55. Eberth JM, Josey MJ, Mobley LR, Nicholas DO, Jeffe DB, Odahowski C, et al. Who performs colonoscopy? Workforce trends over space and time. J Rural Health 2018; 34: 138-47.




56. Ballard TN, Hill S, Nghiem BT, Lysikowski JR, Brandt K, Cederna PS, et al. Current trends in breast augmentation: analysis of 2011-2015 Maintenance of Certification (MOC) Tracer Data. Aesthet Surg J 2019; 39: 615-23.



57. Osman BM, Shapiro FE. Safe anesthesia for office-based plastic surgery: proceedings from the PRS Korea 2018 meeting in Seoul, Korea. Arch Plast Surg 2019; 46: 189-97.




58. Leonardi J. Woman died of pulmonary fat embolism after plastic surgery in Miami: autopsy [Internet]. Miramar (FL): NBC 6; 2022 Jul 14 [updated 2022 Jul 14; cited 2023 Feb 1]. Available from https://www.nbcmiami.com/news/local/woman-died-of-pulmonary-fat-embolism-after-plastic-surgery-in-miami-autopsy/2805712/
59. Mofid MM, Teitelbaum S, Suissa D, Ramirez-Montañana A, Astarita DC, Mendieta C, et al. Report on mortality from gluteal fat grafting: recommendations from the ASERF task force. Aesthet Surg J 2017; 37: 796-806.



60. McLaughlin EJ, Brant JA, Bur AM, Fischer JP, Chen J, Cannady SB, et al. Safety of outpatient thyroidectomy: review of the American College of Surgeons National Surgical Quality Improvement Program. Laryngoscope 2018; 128: 1249-54.



61. Philteos J, Baran E, Noel CW, Pasternak JD, Higgins KM, Freeman JL, et al. Feasibility and safety of outpatient thyroidectomy: a narrative scoping review. Front Endocrinol (Lausanne) 2021; 12: 717427.



62. Rosen P, Bailey L, Manickavel S, Gentile C, Grayson J, Buczek E. Ambulatory surgery vs overnight observation for total thyroidectomy: cost analysis and outcomes. OTO Open 2021; 5: 2473974X21995104.




63. Shapiro FE, Park BH, Levy TS, Osman BM. The assessment of a growing mobile anesthesia practice from 2016 to 2019: a retrospective observational cohort study of 89,999 cases comparing ambulatory surgery (ASC) and office-based surgery (OBS) centers using a high-fidelity, anesthesia-specific electronic medical record (EMR). J Healthc Risk Manag 2022; 41: 27-35.



64. Smilowitz NR, Gupta N, Guo Y, Beckman JA, Bangalore S, Berger JS. Trends in cardiovascular risk factor and disease prevalence in patients undergoing non-cardiac surgery. Heart 2018; 104: 1180-6.



65. Hajmohamed S, Patel D, Apruzzese P, Kendall MC, de Oliveira G. Early postoperative outcomes of super morbid obese compared to morbid obese patients after ambulatory surgery under general anesthesia: a propensity-matched analysis of a national database. Anesth Analg 2021; 133: 1366-73.


66. Ranum D, Beverly A, Shapiro FE, Urman RD. Leading causes of anesthesia-related liability claims in ambulatory surgery centers. J Patient Saf 2021; 17: 513-21.


67. Goldberg JM, Silver MI, Johnson MP. Prevalence of obstructive sleep apnea risk according to the STOP-BANG questionnaire in an oral surgery office-based anesthesia patient population. J Oral Maxillofac Surg 2020; 78: 2156-9.


68. Bongiovanni T, Parzynski C, Ranasinghe I, Steinman MA, Ross JS. Unplanned hospital visits after ambulatory surgical care. PLoS One 2021; 16: e0254039.



69. Gabriel RA, Ilfeld BM. Use of regional anesthesia for outpatient surgery within the United States: a prevalence study using a nationwide database. Anesth Analg 2018; 126: 2078-84.


70. Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg 2002; 95: 627-34.


71. Barrington JW, Hansen RN, Lovelace B, Böing EA, Chughtai M, Newman JM, et al. Impact of intravenous acetaminophen on lengths of stay and discharge status after total knee arthroplasty. J Knee Surg 2019; 32: 111-6.


72. Shah SB, Chawla R, Pahade A, Mittal A, Bhargava AK, Kumar R. Comparison of pectoralis plane blocks with ketamine-dexmedetomidine adjuncts and opioid-based general anaesthesia in patients undergoing modified radical mastectomy. Indian J Anaesth 2020; 64: 1038-46.



73. Martinez L, Ekman E, Nakhla N. Perioperative opioid-sparing strategies: utility of conventional NSAIDs in adults. Clin Ther 2019; 41: 2612-28.


74. Brinck EC, Tiippana E, Heesen M, Bell RF, Straube S, Moore RA, et al. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst Rev 2018; 12: CD012033.



75. Dissanayake R, Du HN, Robertson IK, Ogden K, Wiltshire K, Mulford JS. Does dexamethasone reduce hospital readiness for discharge, pain, nausea, and early patient satisfaction in hip and knee arthroplasty? A randomized, controlled trial. J Arthroplasty 2018; 33: 3429-36.


76. Alrayashi W, Zurakowski D, Sullivan CA, Berde CB, Askins N, Sinnott S, et al. The effect of suprainguinal fascia iliaca block on the recovery of patients after arthroscopic hip surgery. Paediatr Anaesth 2019; 29: 829-34.


77. Stjernberg M, Schlichting E, Rustoen T, Valeberg BT, Småstuen MC, Raeder JC. Postdischarge pain, nausea and patient satisfaction after diagnostic and breast-conserving ambulatory surgery for breast cancer: a cross-sectional study. Acta Anaesthesiol Scand 2022; 66: 317-25.



78. Herzig SJ, Anderson TS, Jung Y, Ngo L, Kim DH, McCarthy EP. Relative risks of adverse events among older adults receiving opioids versus NSAIDs after hospital discharge: a nationwide cohort study. PLoS Med 2021; 18: e1003804.



79. Shapiro FE, Punwani N, Rosenberg NM, Valedon A, Twersky R, Urman RD. Office-based anesthesia: safety and outcomes. Anesth Analg 2014; 119: 276-85.


80. FSMB. Office-based surgery (OBS)- board-by-board statutes, regulations, and policies [Internet]. Euless (TX): Federation of State Medical Boards; 2020 May [updated 2023 Mar 31; cited 2023 Feb 1]. Available from https://www.fsmb.org/siteassets/advocacy/policies/office-based-surgery-overview.pdf









