|
 |
| Korean J Anesthesiol > Volume 76(4); 2023 > Article |
|
Abstract
Background
Methods
Results
NOTES
Funding
The authors wish to acknowledge the financial support made by the Catholic Medical Center Research Foundation during the program year of 2020 (52020B000100025).
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Kwon Hui Seo (Data curation; Formal analysis; Investigation; Writing ã original draft)
Ji Hyung Hong (Conceptualization; Data curation; Formal analysis; Funding acquisition; Writing ã review & editing)
Mi Hyoung Moon (Data curation; Investigation)
Wonjung Hwang (Methodology; Resources)
Sea-Won Lee (Investigation)
Jin Young Chon (Supervision)
Hyejin Kwon (Data curation)
Sook Hee Hong (Supervision)
Sukil Kim (Methodology)
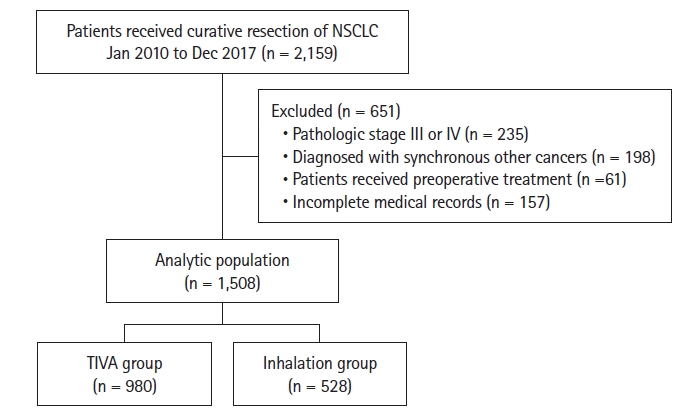
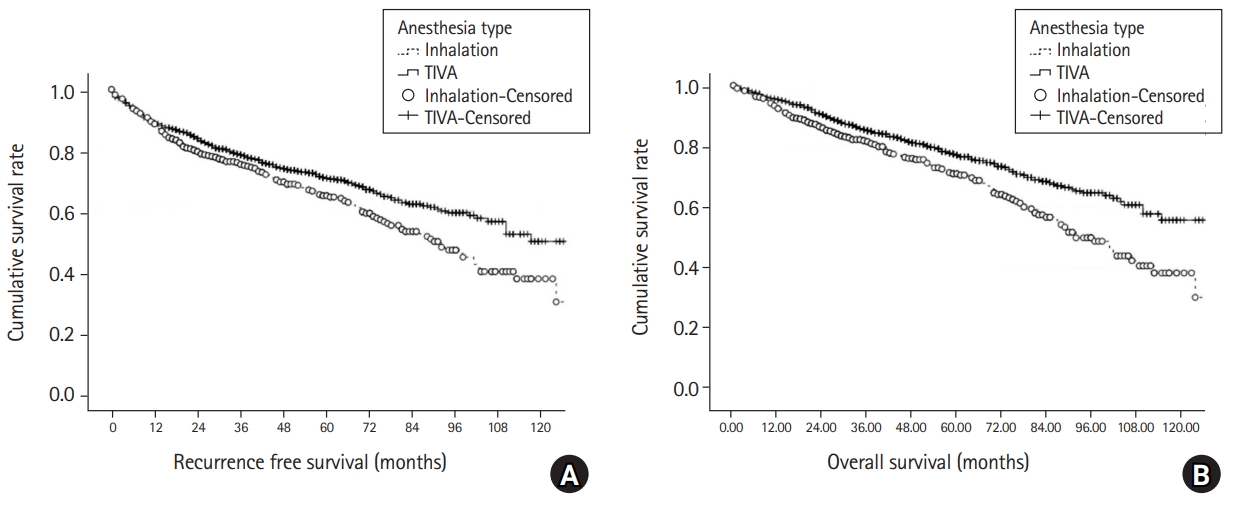
Fig.ô 2.
Tableô 1.
Values are presented as median (Q1, Q3) or number of patients (%). TIVA: total intravenous anesthesia, BMI: body mass index, ASA physical status: American Society of Anesthesiologists physical status, HBP: hypertension, DM: diabetes mellitus, COPD: chronic obstructive pulmonary disease, RUL: right upper lobe, RML: right middle lobe, RLL: right lower lobe, LUL: left upper lobe, LLL: left lower lobe, TNM: tumor, nodes, and metastases, PRC: packed red cells.
Tableô 2.
RFS: recurrence-free Survival, HR: hazard ratio, BMI: body mass index, ASA PS: American Society of Anesthesiologists physical status, HBP: hypertension, DM: diabetes mellitus, COPD: chronic obstructive pulmonary disease, RUL: right upper lobe, RML: right middle lobe, RLL: right lower lobe, LUL: left upper lobe, LLL: left lower lobe, PRC: packed red cells, TIVA: total intravenous anesthesia.
Tableô 3.
OS: overall survival, HR: hazard ratio, BMI: body mass index, ASA PS: American Society of Anesthesiologists physical status, HBP: hypertension, DM: diabetes mellitus, COPD: chronic obstructive pulmonary disease, RUL: right upper lobe, RML: right middle lobe, RLL: right lower lobe, LUL: left upper lobe, LLL: left lower lobe, PRC: packed red cells, TIVA: total intravenous anesthesia.