 |
 |
| Korean J Anesthesiol > Volume 73(3); 2020 > Article |
|
Abstract
Background
There have been reports of neurolytic transversus abdominis plane (TAP) block using different agents such as alcohol or phenol for the treatment of chronic abdominal pain caused by malignant abdominal wall invasion. However, to date, there have been no reports on neurolytic abdominal wall blocks for pain with non-cancer-related origin in cancer patients.
Case
We performed subcostal TAP neurolysis using ethanol in a patient with esophageal cancer with constant pain at the site of gastrostomy. After neurolysis, the patient’s overall pain decreased, with the exception of pain in the medial part of the gastrostomy site. We performed additional rectus sheath neurolysis using ethanol for the treatment of continuous pain at the medial site, and the effect of neurolysis has persisted for over 4 months.
Regional anesthesia techniques for the abdominal wall, such as rectus sheath block and transversus abdominis plane (TAP) block, are components of multimodal anesthesia that are utilized in various types of surgeries, including different abdominal surgeries with accompanying laparotomy (including major abdominal surgeries), hernia repair, and cesarean delivery.
In this perioperative setting, abdominal wall block techniques are known to improve the quality of analgesia and reduce postoperative opioid consumption [1]. More specifically, the recent use of ultrasonography in these block techniques allows accurate localization of the needle tip and real-time confirmation of drug spread, which consequently reduces side effects and increases efficacy [2]. In addition, there are cases of long-term analgesia provision via catheter placement, which is being utilized following abdominal surgery.
Meanwhile, there have been attempts to utilize these regional anesthetic techniques applied to the abdominal wall for chronic pain control. There have been reports of cases in which symptoms were successfully relieved via nerve block using local anesthetics as shown in a previous case series [3] that attempted TAP block using local anesthetics for the management of postoperative abdominal pain. Furthermore, there have been cases of attempted neurolysis for longer term treatment efficacy. Previous cases [4,5] have attempted TAP neurolysis using alcohol for the management of pain due to advanced cancer involving the abdominal wall, and another similar case [6] reported the use of phenol for TAP neurolysis. However, there has not been a case report describing neurolysis performed on the rectus sheath, and cases of alcohol-based neurolysis on the abdominal wall plane for management of non-cancer pain in cancer patient.
In this case report, we describe the case of a patient with persistent, intractable pain at the gastrostomy site despite long-term opioid use. We attempted alcohol-based TAP neurolysis and rectus sheath neurolysis, which successfully provided pain control without further opioid usage.
The patient provided written consent for the publication of this case.
A 70-year-old male patient visited our pain clinic in December 2017 with gastrostomy site pain that started after percutaneous radiological gastrostomy was performed in May 2017.
The patient did not have any previous medical history, except for esophageal cancer located 26–32 cm inferior to the upper incisors. He received concurrent chemotherapy for a month in January 2017 but exhibited worsening of dysphagia and a consequent tendency of aspiration. For proper feeding, he underwent percutaneous radiological gastrostomy in May 2017.
Although he experienced constant pain near the gastrostomy site immediately after the procedure, oncologist continued the use of the percutaneous endoscopic gastrostomy (PEG) tube due to the persistent tendency of aspiration. In June 2017, the patient was treated with a fentanyl patch 75 µg/h and short-acting fentanyl buccal Tab 400 µg for pain management and required hospitalization due to features of delirium suspected to originate from opioid treatment.
When he visited our pain clinic in December 2017, he was being fed via the PEG tube. There were no abnormal findings on the abdominal computed tomography images, and physical examination did not indicate infection of the gastrostomy site. The patient also underwent PEG tube exchange under image guidance to ensure proper positioning of the tube, prior to visiting our pain clinic.
The pain was localized to the gastrostomy site and nearby abdominal wall located left and inferior to the xiphoid process. In addition, the pain was dull, with no signs of tenderness or local inflammation (Fig. 1). The patient was given a combination of acetaminophen 325 mg and tramadol HCl 37.5 mg 4 times a day for pain management. Although the pain control was effective (numerical rating scale [NRS] score of 5/10) for ~2 h after drug intake, the patient sometimes experienced severe pain with an NRS score of 9/10.
In addition to the oral administration of acetaminophen and tramadol, we locally applied a lidocaine patch and lidocaine 2.5% and prilocaine 2.5% cream to the site, but this was not effective. The use of 10% lidocaine spray was effective for ~20 min after the use, and therefore was utilized together with other drugs.
Nevertheless, there was no persistent improvement in pain. In January 2018, we attempted left-sided subcostal TAP block using 0.8% mepivacaine 4 cm3, and triamcinolone 10 mg and additional local anesthetics infiltration at the gastrostomy site using 1% lidocaine 4 cm3, under ultrasonography guidance. Immediately after the procedure, the pain near the gastrostomy tube was alleviated by ≥ 50% but quickly became aggravated again. After 2 weeks, we performed additional left-sided subcostal TAP block and lidocaine local infiltration at the gastrostomy site. Previous procedures were repeated. However, substantial pain relief was unclear after the procedure, and we were forced to provide oral administration of acetaminophen 325 mg plus tramadol HCl 37.5 mg 3 times a day and short-acting oxycodone HCl 5 mg in case of severe pain. However, the pain control was not effective, and the patient visited the emergency center several times due to pain.
Subsequently, the patient’s dysphagia symptoms improved and the PEG tube was removed in May 2018. However, the patient continued to experience persistent abdominal wall pain near the gastrostomy site. This dull pain had an atypical tendency to worsen at night (NRS score of 9/10). As the pain relief from traditional medications (i.e., oxycodone HCl or acetaminophen 325 mg plus tramadol HCl 37.5 mg) was not effective, we considered additional opioid usage.
We explained to the patient that appropriate intake of the prescribed medication for pain control and dose titration are crucial. However, the patient strongly refused to use further opioid due to fear of using strong opioids—he reported a history of severe delirium caused by opioid usage (including high-dose fentanyl patch) prior to visiting our pain clinic, as well as side effects (i.e., constipation and drowsiness) after oral opioid usage after admission to our pain clinic. The patient continued to suffer from gastrostomy site pain and had difficulties in rehabilitation and daily activities (i.e., deep breathing and supraglottic swallowing) due to pain.
The effectiveness of oral medications, such as opioids, and of topical treatments, such as lidocaine patch, cream, and spray, was inappropriate. Whereas TAP block and local infiltration of lidocaine provided short-term pain relief by ≥ 50% without any side effects.
Therefore, we decided to perform left-sided TAP prognostic block and subsequent neurolytic block. We explained possible side effects (i.e., neuritis, deafferentation pain, or abdominal muscle weakness) and unclear long-term outcomes. The patient still wanted to undergo neurolytic TAP block.
We performed left-sided subcostal TAP using 0.5% bupivacaine 5 cm3 under ultrasonography guidance. The patient exhibited temporary pain relief (~5 h after procedure) and the pain worsened again, indicating positive outcome of prognostic block.
In June 2018 (7 days after), we performed left-sided subcostal TAP neurolysis. We identified the abdominal muscle layer and rectus sheath under ultrasonography guidance and injected 0.8% mepivacaine 3 cm3 using a 26-G spinal needle. We confirmed concordant pain relief after 5 min and injected 6 cm3 of 100% ethanol with the spinal needle (Fig. 2A). The total ethanol concentration for neurolysis was assumed to be 66%.
The patient did not experience any side effects except slight discomfort at the injection site immediately after alcohol injection and started to experience pain relief. The patient barely experienced any pain (NRS 0/10) immediately after neurolysis. On the outpatient visit 1 week later, he still experienced mild pain (NRS 3/10) near the medial tip of the gastrostomy site but had no pain in other sites. Pain relief was continuously observed until the 2-month outpatient follow-up, and we discontinued the use of opioids and utilized pregabalin 75 mg for abdominal pain control. However, 3 months after neurolysis, the patient started to experience abdominal pain at the medial tip of gastrostomy site (NRS 6/10), and we were forced to increase the pregabalin dose and use short-acting opioids such as oxycodone HCl.
The patient refused to use opioid again due to constipation and wanted other treatment option. We performed left-sided rectus sheath block using 0.5% bupivacaine 5 cm3 under ultrasonography guidance, and a positive outcome (pain relief) was observed.
On the 3rd month after the first neurolysis procedure, we performed rectus sheath neurolysis by injecting 0.8% mepivacaine 3 cm3 and then injecting 100% ethanol 7 cm3 (Fig. 2B). The total ethanol concentration for neurolysis was assumed to be 70%.
The patient did not experience discomfort during the procedure and started to experience pain relief. Pain at the medial tip of the gastrostomy site substantially reduced from NRS 6/10 to 2/10. Currently, he is under 4-month follow-up, with pregabalin 150 mg 2 times a day and no opioid usage.
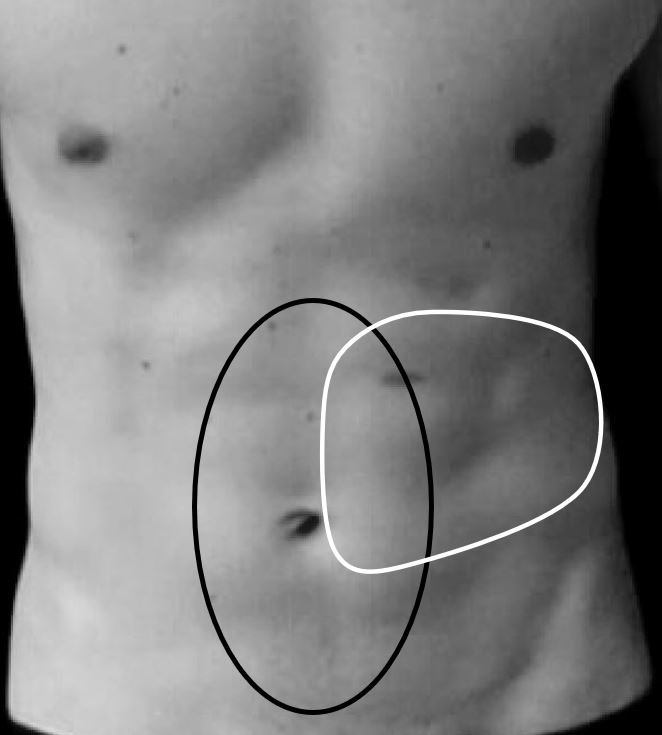
Subcostal TAP block acts on the fascial plane between the internal oblique and transversus abdominis, which contain the nerves from T7 to T10, to establish sensory block of the abdominal wall. Rectus sheath block acts on the terminal branches of the 7–11th intercostal nerves, which penetrate the posterior wall of the rectus abdominis muscle. Therefore, it provides better coverage of sense organs near the midline of abdomen relative to TAP block [7]. Based on the location of the pain in different patients, an appropriate method should be utilized to ensure analgesia of the whole abdomen (Fig. 3).
Thus, depending on the location of the pain, rectus sheath neurolysis can be considered a treatment option for intractable pain management, along with TAP neurolysis.
TAP neurolysis cases reported thus far have been focused on pain management in patients with cancerous invasion of the abdominal wall. On the other hand, we report the case of a cancer patient who received intervention for the management of treatment-associated pain.
The patient in this case report suffered from atypical pain due to gastrostomy performed as a supportive part of cancer treatment, not because of abdominal wall invasion by the cancer.
Pain at the gastrostomy site often occurs acutely, and multiple causes including leakage, local infection, gastric mucosa irritation caused by tube malposition, peritoneum irritation, and pain caused by progression of the primary cancer have been reported [8].
For the patient in our case report, we assessed for potential malposition and local infection at the time of PEG tube exchange. However, the patient experienced persistent, atypical pain even after tube removal.
From the characteristics of the pain, we hypothesized that the patient was suffering from somatic and/or neuropathic pain of unknown etiology rather than from visceral pain. We attempted to provide pain relief using various medications including opioids and topical agents. However, despite the clear side effects of opioids, appropriate pain control was not achieved. More specifically, the patient was undergoing rehabilitation of supraglottic swallowing due to symptoms of dysphagia and aspiration tendency. The abdominal pain was hindering deep breathing.
Therefore, in order to prolong the effectiveness of TAP block using local anesthetics, we attempted neurolysis using alcohol, one of the agents used for peripheral nerve neurolysis, and successfully provided effective pain control and opioid sparing for ~4 months after the initial neurolysis.
In a previously reported case, TAP neurolysis using 33% ethanol was performed in a hospice patient with periumbilical pain due to abdominal wall mass associated with metastatic colon cancer, and although the pain decreased from NRS 7/10 to 0/10 over 2 days, the patient died on the 5th postoperative day because of cancer progression [5].
In another case series, TAP neurolysis using 33%–70% ethanol achieved pain reduction ≥ 50% over 17 days to 3 months in cases of abdominal pain due to colon cancer involving abdominal wall or neuroendocrine tumor involving abdominal wall [4].
A case report of TAP neurolysis using phenol for pain extending from the umbilicus to the pubis due to epithelioid sarcoma involving the abdominal wall reported pain reduction from NRS 5/10 to 0/10 over a maximum of 3 weeks [6].
The previously reported cases used neurolysis to relieve pain due to cancer directly involving the abdominal wall. Whereas in our case, we used neurolysis to treat pain of non-cancerous origin, and pain reduction was achieved for up to 4 months.
In this case report, we utilized alcohol as a neurolytic agent. For TAP neurolysis, there are reports of the use of either alcohol or phenol, but no previous study has compared the effectiveness of the two agents. A previous study that performed splanchnic nerve neurolysis for abdominal pain control has demonstrated that there is no difference in effect of phenol and alcohol [9], but additional studies are required for neurolysis of the abdominal wall.
As of now, the neurolytic agent should be selected considering multiple factors, including the following: painful stimulation at the time of alcohol injection, possibility of neuritis, and the surgeon’s convenience based on characteristics (i.e., viscosity of phenol).
In conclusion, although additional studies for the selection of the neurolytic agent and procedure indication/efficacy are needed, we demonstrated that alcohol-based TAP neurolysis and rectus sheath neurolysis provide effective pain control and opioid sparing in a cancer patient with chronic treatment-related pain involving the abdominal wall.
Fig. 2.
(A) Transversus abdominis plane neurolysis ultrasonography image. EO: external oblique muscle, IO: internal oblique muscle. (B) Rectus sheath neurolysis ultrasonography image.
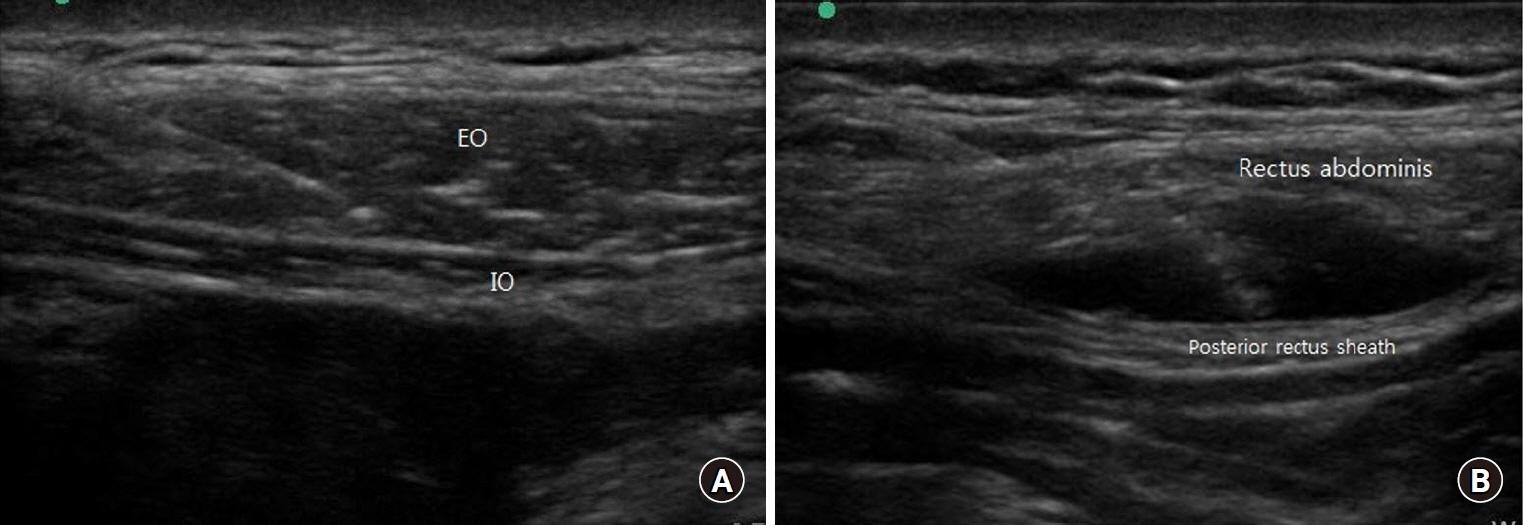
Fig. 3.
Comparison of sensory block areas between left-sided subcostal transversus abdominis plane (TAP) block and bilateral rectus sheath block. Black oval: rectus sheath block, White oval: left subcostal TAP block.
References
1. Johns N, O’Neill S, Ventham NT, Barron F, Brady RR, Daniel T. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta-analysis. Colorectal Dis 2012; 14: e635-42.


2. Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth 2005; 94: 7-17.


3. Baciarello M, Migliavacca G, Marchesini M, Valente A, Allegri M, Fanelli G. Transversus abdominis plane block for the diagnosis and treatment of chronic abdominal wall pain following surgery: a case series. Pain Pract 2018; 18: 109-17.


4. Hung JC, Azam N, Puttaniah V, Malhotra V, Gulati A. Neurolytic transversus abdominal plane block with alcohol for long-term malignancy related pain control. Pain Physician 2014; 17: E755-60.


5. Sakamoto B, Kuber S, Gwirtz K, Elsahy A, Stennis M. Neurolytic transversus abdominis plane block in the palliative treatment of intractable abdominal wall pain. J Clin Anesth 2012; 24: 58-61.


6. Gebhardt R, Wu K. Transversus abdominis plane neurolysis with phenol in abdominal wall cancer pain palliation. Pain Physician 2013; 16: E325-30.


7. Yarwood J, Berrill A. Nerve blocks of the anterior abdominal wall. Continuing Educ Anaesth Crit Care Pain 2010; 10: 182-6.












