1. Webb CA, Mariano ER. Best multimodal analgesic protocol for total knee arthroplasty. Pain Manag 2015; 5: 185-96.


2. Kehlet H, Andersen L├ś. Local infiltration analgesia in joint replacement: the evidence and recommendations for clinical practice. Acta Anaesthesiol Scand 2011; 55: 778-84.


3. Tripuraneni KR, Woolson ST, Giori NJ. Local infiltration analgesia in TKA patients reduces length of stay and postoperative pain scores. Orthopedics 2011; 34: 173.


4. Perlas A, Kirkham KR, Billing R, Tse C, Brull R, Gandhi R, et al. The impact of analgesic modality on early ambulation following total knee arthroplasty. Reg Anesth Pain Med 2013; 38: 334-9.


6. Steckelberg RC, Funck N, Kim TE, Walters TL, Lochbaum GM, Memtsoudis SG, et al. Adherence to a multimodal analgesic clinical pathway: a within-group comparison of staged bilateral knee arthroplasty patients. Reg Anesth Pain Med 2017; 42: 368-71.


7. Thobhani S, Scalercio L, Elliott CE, Nossaman BD, Thomas LC, Yuratich D, et al. Novel regional techniques for total knee arthroplasty promotereduced hospital length of stay: an analysis of 106 patients. Ochsner J 2017; 17: 233-8.


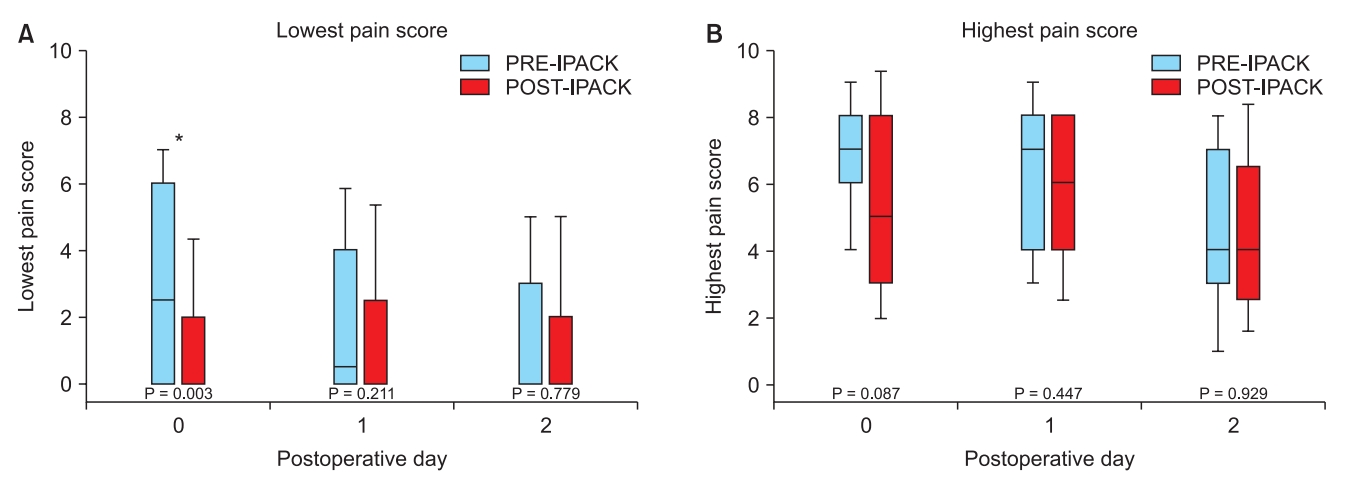
8. Kim DH, Beathe JC, Lin Y, YaDeau JT, Maalouf DB, Goytizolo E, et al. Addition of infiltration between the popliteal artery and the capsule of the posterior knee and adductor canal block to periarticular injection enhances postoperative pain control in total knee arthroplasty: a randomized controlled trial. Anesth Analg. 2018, Advance Access published on Sep 12, 2018. doi: 10.1213/ANE.0000000000003794.
9. Walters TL, Howard SK, Kou A, Bertaccini EJ, Harrison TK, Kim TE, et al. Design and implementation of a perioperative surgical home at a veterans affairs hospital. Semin Cardiothorac Vasc Anesth 2016; 20: 133-40.


10. Mariano ER, Walters TL, Kim TE, Kain ZN. Why the perioperative surgical home makes sense for veterans affairs health care. Anesth Analg 2015; 120: 1163-6.


11. Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf 2014; 23: 290-8.


12. Mariano ER, Kim TE, Wagner MJ, Funck N, Harrison TK, Walters T, et al. A randomized comparison of proximal and distal ultrasoundguided adductor canal catheter insertion sites for knee arthroplasty. J Ultrasound Med 2014; 33: 1653-62.


13. Mudumbai SC, Walters TL, Howard SK, Kim TE, Lochbaum GM, Memtsoudis SG, et al. The Perioperative Surgical Home model facilitates change implementation in anesthetic technique within a clinical pathway for total knee arthroplasty. Healthc (Amst) 2016; 4: 334-9.


14. Mudumbai SC, Auyong DB, Memtsoudis SG, Mariano ER. A pragmatic approach to evaluating new techniques in regional anesthesia and acute pain medicine. Pain Manag 2018; 8: 475-85.


16. Memtsoudis SG, Poeran J, Zubizarreta N, Cozowicz C, M├Črwald EE, Mariano ER, et al. Association of multimodal pain management strategies with perioperative outcomes and resource utilization: a population-based study. Anesthesiology 2018; 128: 891-902.


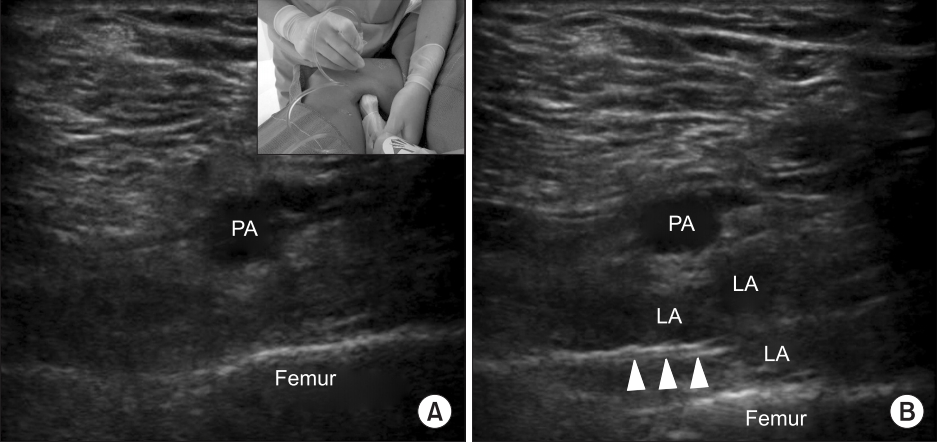
18. Niesen AD, Harris DJ, Johnson CS, Stoike DE, Smith HM, Jacob AK, et al. Interspace between popliteal artery and posterior capsule of the knee (IPACK) injectate spread: a cadaver study. J Ultrasound Med 2019; 38: 741-5.


19. Mudumbai SC, Kim TE, Howard SK, Workman JJ, Giori N, Woolson S, et al. Continuous adductor canal blocks are superior to continuous femoral nerve blocks in promoting early ambulation after TKA. Clin Orthop Relat Res 2014; 472: 1377-83.


20. Yajnik M, Hill JN, Hunter OO, Howard SK, Kim TE, Harrison TK, et al. Patient education and engagement in postoperative pain management decreases opioid use following knee replacement surgery. Patient Educ Couns 2019; 102: 383-7.


22. Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA 1999; 282: 1458-65.


23. Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ Jr. An educational intervention decreases opioid prescribing after generalsurgical operations. Ann Surg 2018; 267: 468-72.