|
 |
|
|
Abstract
Background
Chronic low back pain (CLBP) has a significant effect on quality of life and imposes a great economical burden on society. In a number of studies, validated questionnaires had been given to CLBP patients to determine their health-associated quality of life, sleep disturbance, and psychological status. However, such outcome studies had not been performed previously in Korea.
Methods
We used self-report questionnaires to compare CLBP patients with an age- and sex-matched healthy control group. Between September 2012 and August 2013, we enrolled 47 patients who had CLBP for more than 3 months (group P) and 44 healthy age- and sex-matched controls (group C), who completed the following self-report questionnaires: 36-Item Short Form Health Survey (SF-36), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Oswestry Disability Index (ODI), and Pittsburgh Sleep Quality Index (PSQI).
Results
The scores from the ODI, BDI, and BAI were significantly higher in group P than in group C. The SF-36 scores were significantly lower in group P than in group C, suggesting lower quality of life in group P. The incidence of depression and anxiety was significantly higher in group P than in group C. However, neither the PSQI score nor the incidence of sleep disturbance was significantly different between the groups.
Low back pain (LBP), the most common musculoskeletal disease, is experienced by 70-85% of the general population at some point in their lives [1]. Previous studies have shown that LBP plays a major role in the activities of daily living, losses in work days, and productivity [2]. The incidence of chronic low back pain (CLBP) has been reported to be 9% to 21% in the general population and has been increasing steadily [3,4]. As a result, disability associated with CLBP has been studied extensively, and psychosocial factors that may contribute to pain and disabilities have also been studied systematically [5,6,7,8,9].
Growing evidence suggests that depression, anxiety, and sleep disturbance correlate well with the degree of pain [5,10,11,12]. In addition, numerous studies have shown a high prevalence of depression, anxiety, and sleep disturbance in patients with chronic musculoskeletal pain including low back pain, osteoarthritis, rheumatoid arthritis and fibromyalgia [13,14,15,16].
Recent studies have also demonstrated that general health related quality of life in patients with LBP showed a significant correlation with pain and disability [17], an impairment mostly from the physical aspect in lumbar radiculopathy patients [18].
The impact of chronic pain on psychological symptoms such as depression, anxiety and sleep disturbance, and quality of life has been the subject of interest in western countries. Therefore, disease-specific validated questionnaires have been developed for clinical purposes. However, there has never been research conducted on health associated quality of life, sleep disturbance and psychological status using a generic questionnaire aimed at Korean LBP patients, nor has there been research conducted using a disease-specific questionnaire which has been validated and translated into the Korean language.
Therefore, in this study, we compared CLBP patients with an age- and sex- matched normal healthy control group in aspects of disability, depression, anxiety, quality of life and sleep disturbance via self-administered questionnaires that are available in Korean and have been validated to have reliability in LBP patients in previous studies [19,20,21,22,23]. The questionnaires employed in this study are the 36-Item Short Form Health Survey (SF-36), Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), Oswestry Disability Index (ODI), and Pittsburgh Sleep Quality Index (PSQI).
This study enrolled 47 patients with CLBP (group P) who first visited an outpatient pain clinic between September 2012 and August 2013. Written informed consent was obtained from all patients after obtaining approval from the Institutional Review Board. All patients with CLBP were included even if they were receiving any prior conservative treatment. The exclusion criteria were (1) patients with LBP less than 3 months, (2) CLBP combined with other musculoskeletal diseases, (3) systemic medical disease such as cardiac disease, chronic renal failure, fibromyalgia and dysthyroidism, (4) history of back surgery, (5) primary psychiatric disorder such as depression, anxiety, or insomnia, and (6) individual who is incapable of understanding and answering the questionnaires. All spine pathologies were confirmed by magnetic resonance imaging.
The control group (group C) was composed of healthy volunteers without any LBP who visited our hospital for a medical check up and were age- and sex- matched with the study group. The exclusion criteria for group C were (1) presence of musculoskeletal disease, (2) any systemic disease, or (3) any history of psychiatric diseases. Among the 47 matched individuals in the control group, 1 individual did not complete the survey and 2 individuals were suffering from other musculoskeletal diseases. Therefore, 44 individuals were included as group C.
Participants were evaluated with the BDI, BAI, ODI, SF-36, and PSQI. Detailed instructions and information on how to complete the questionnaires were provided.
The ODI measures the extent to which the functional level of a patient is limited by LBP. Jeon et al. [19] conducted the cross-cultural adaptation for translating the English original version of the ODI into a Korean version. The ODI of the Korean version showed satisfactory reliability, and the Cronbach's alpha value and the test-retest correlation reliability were 0.9168 and 0.9332 respectively [19].
Depression in patients with CLBP was assessed with the BDI, a standardized questionnaire for the evaluation of cognitive, affective and somatic symptoms of depression. The Korean version of the BDI showed significant positive internal consistency (r = 0.88), and test-retest reliability (r = 0.60) [20]. A score of 16 has been suggested as an optimal cut-off value for the screening of depression in Korea [20].
The BAI is a 21-item self-report questionnaire designed to evaluate anxiety symptoms. Each question is on a four-point scale that adds up to a total score of 0 to 63, with 0 representing no anxiety and 63 representing severe anxiety. A Korean language version has been shown to have reliability and validity across both patients and the general population [21].
The Korean version of the SF-36 was used to assess the quality of life of the participants. It contains 36 items for a general health survey. The Korean version of the SF-36 was found to have satisfying content validity and discriminant validity. Cronbach's alpha coefficients were from 0.9298 to 0.9383 [22]. The test-retest reliability coefficients ranged from 0.710 to 0.895. The 36 items and scales are constructed using the Likert method of summated ratings. The SF-36 contains eight itemized categories and 36 questions. The eight categories are: 1) physical functioning (walking, lifting); 2) role function-physical (limitations in ability to perform usual activities); 3) bodily pain (level of bodily pain or discomfort); 4) general health perceptions (global evaluation of health); 5) vitality (energy level or fatigue); 6) social functioning (impact of health or emotional problems on social activities); 7) role function-emotional (impact of emotional problems on work or daily activities) and 8) mental health (anxiety, depression, sense of psychological well-being). The first four categories are the physical component, while the last four categories show the mental component of the survey. These ratings are summed to yield raw scale scores for each health concept and are converted to a 0 to 100 scale, with 100 indicating the best possible score.
The PSQI is a 19-item, self-reported, questionnaire-based assessment of sleep patterns to measure subjective sleep quality. It has been widely used by various researchers to monitor and evaluate insomnia among patients [9,10,12]. Sohn et al. [23] analyzed the reliability and validity of the Korean version of the PSQI and evaluated its usefulness. The PSQI of the Korean version showed high reliability, and the Cronbach's coefficient and test-retest correlation coefficient were 0.84 and 0.65, respectively. The contents of the PSQI includes subjective sleep duration, sleep quality, sleep latency, habitual sleep efficiency, sleep disturbances, use of sleep medication and daytime dysfunction [23]. For our assessment, sleep disturbance was defined as a score greater than 5.
To evaluate the homogeneity of groups C and P, demographic data including age, sex, educational status, marital status, occupational status, smoking, and drinking was compared. For the age, which is a continuous variable, the Mann-Whitney U test was used, and for the others, which are nominal variables, the chi-square test was used. In comparing the ODI, BDI, BAI, SF-36, and PSQI scores of groups C and P, ANCOVA was used in order to exclude the influence of educational status on the questionnaire scores, which was significantly different between the two groups. The 8 detailed categories of the SF-36 were compared between the two groups. To identify the correlation between the ODI, BDI, BAI, SF-36 and PSQI, Spearsman correlation analysis was used. We used power analysis to identify the proper sample size. Based on an α error level of 0.05, and a β error level of 0.2, 35 patients were required to detect a mean difference of 30 and standard deviation of 15 between groups in SF-36 scores. For all the analysis SPSS 12.0 (SPSS Inc, Chicago, IL, USA) was used.
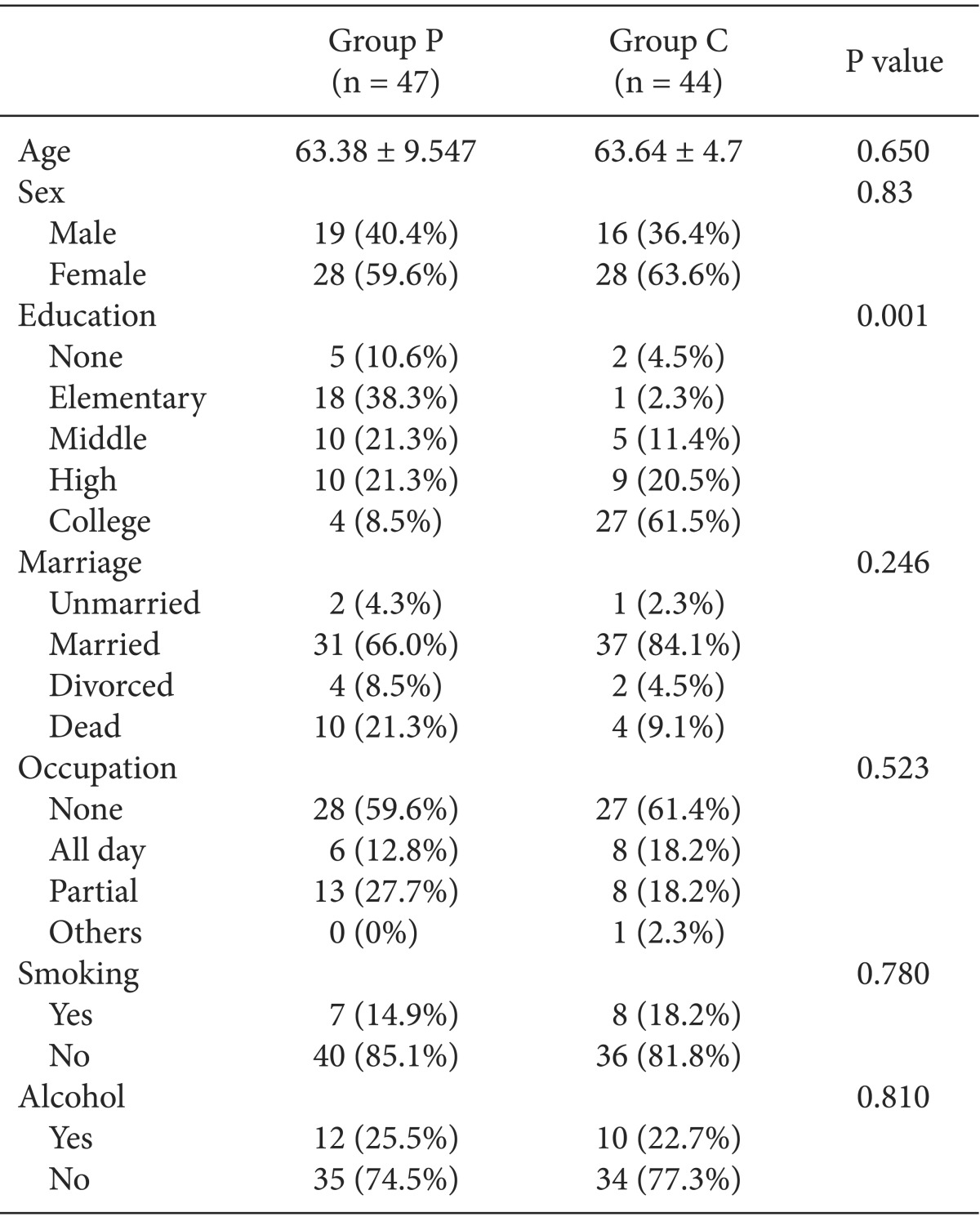
Group P and C did not show any statistically significant differences in the aspects of age, sex, marital status, occupational status, smoking, and drinking. However, the educational status between the two groups was significantly different (P = 0.000; Table 1).
Accordingly, ODI, BDI, BAI, SF-36, and PSQI were analyzed by ANCOVA and the expected mean values were compared excluding the influence of educational status.
The diagnosis of group P includes spinal stenosis (39/47), discogenic LBP (3/47), facet joint pain (3/47), and compression fracture (2/47).
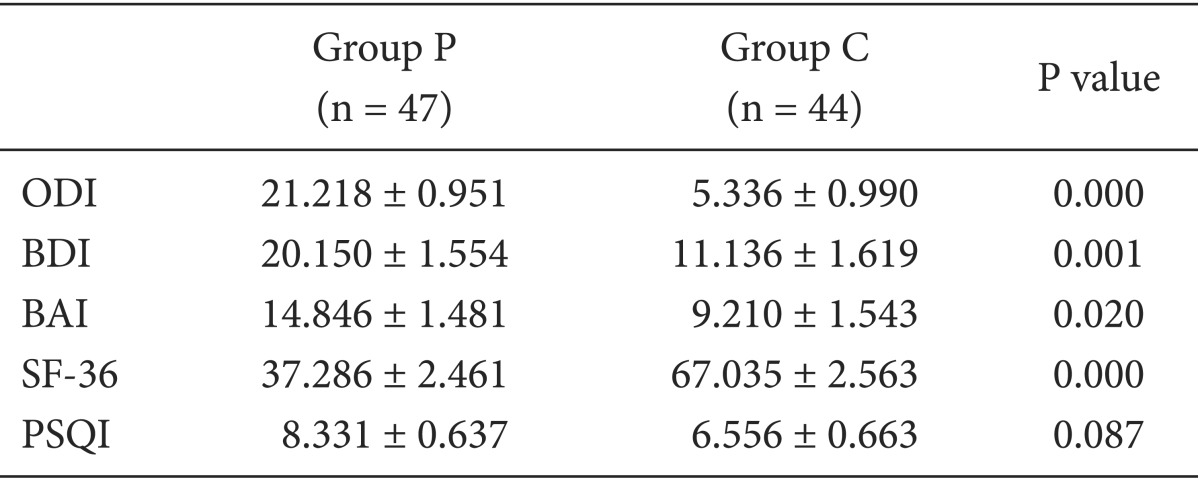
The expected mean ODI score of group P was higher compared to that of group C (21.22 vs 5.34, P = 0.000). The expected mean BDI and BAI scores were also higher in group P compared to group C (20.15 vs 11.14, P = 0.001 and 14.85 vs 9.21, P = 0.020, respectively). In addition, group P revealed significantly lower scores on the SF-36 than group C, which indicates the impairment of quality of life (37.29 vs 67.04, P = 0.000). While all the other scores demonstrated significant differences between the two groups, PSQI scores between the two groups did not differ significantly (8.33 vs 6.56, P = 0.087, Table 2).
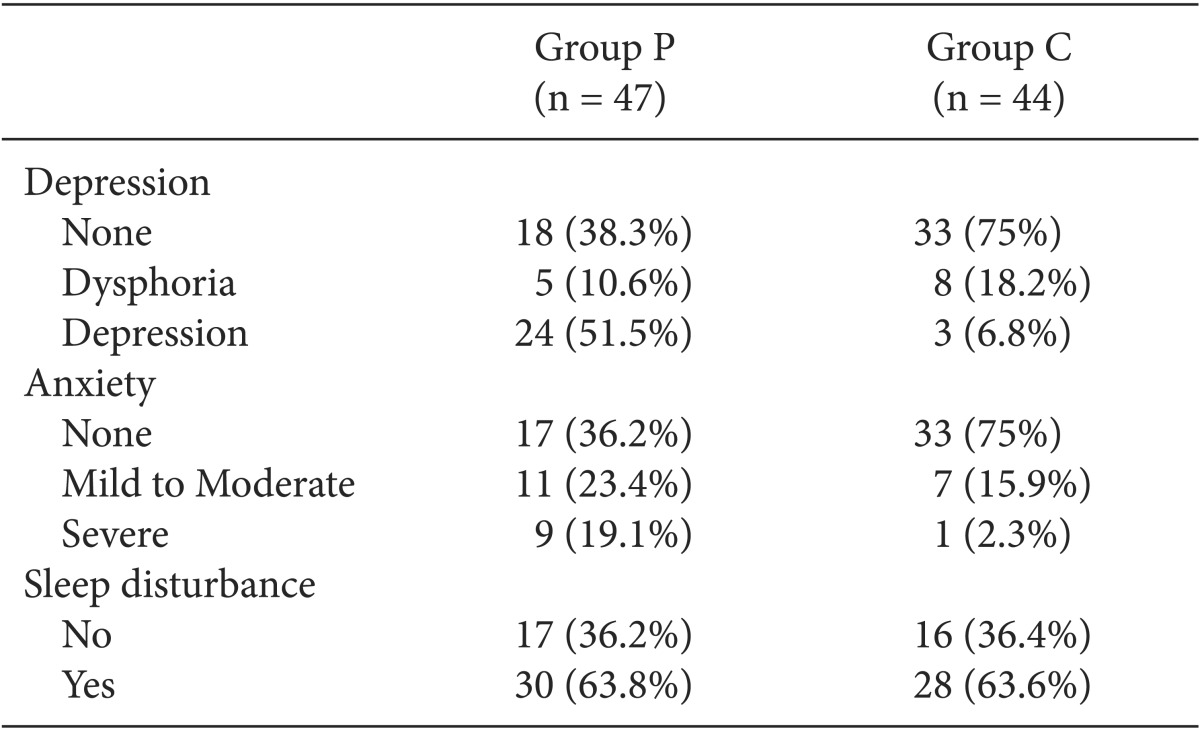
The incidence of depression (51.5 vs 6.8%, P = 0.000) and anxiety (42.5 vs 18.2%, P = 0.000) was higher in group P than in group C, with statistical significance. There was no significant difference in the incidence of sleep disturbance between the two groups (63.8 vs 63.6%, P = 0.985, Table 3).
There was no significant correlation between age and BDI, BAI, and PSQI scores. Nor was any significant correlation found between pain duration and BDI, BAI, and PSQI scores. However, the pain duration showed a negative correlation with SF-36. BDI, BAI, and PSQI scores showed a positive correlation with ODI, while SF-36 showed a negative correlation with ODI (Table 4).
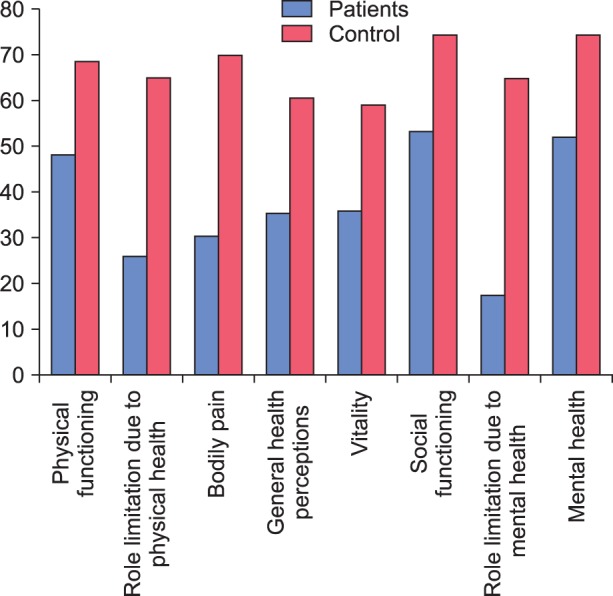
The detailed categories of the SF-36 were compared between the two groups, and all 8 categories demonstrated significant differences. Each of the 8 scores was lower in group P compared with group C, including physical functioning (48.34 vs 68.82, P = 0.001), role limitations due to physical health (25.89 vs 64.96, P = 0.000), bodily pain (30.47 vs 69.86, P = 0.000), general health perceptions (35.44 vs 60.69, P = 0.000), vitality (35.84 vs 58.88, P = 0.000), social functioning (53.30 vs 74.48, P = 0.000), role limitations due to mental health (17.27 vs 64.85, P = 0.000), and mental health (51.96 vs 74.23, P = 0.000, Fig. 1).
Using self-report questionnaires is a potential way to measure functional disability and psychological status. In this study, we used disease specific Korean versions of questionnaires which have been validated and they revealed considerable functional disability with impairment of psychological status and low quality of life.
The incidence of disability related to CLBP is known to be 65% and factors associated with disability include work situation, low self efficacy, and depression [2]. Soysal et al. [24] compared preoperative CLBP outpatients with a healthy control group and concluded that disability assessed by ODI score was higher in the order of preoperative patient, outpatient, and control. We found that patients who had experienced LBP for 3 months or longer had considerable functional disability (mean ODI score, 21.218 ± 0.951).
Depression and anxiety are the most frequently mentioned psychiatric illnesses in CLBP patients. Polatin et al. [7] described that 59% of 200 CLBP patients, who were starting a functional rehabilitation program, met the diagnostic criteria for psychiatric illnesses. Major depression and anxiety were two common diagnoses among them [7]. The prevalence of depression and anxiety were reported as 55 and 48.57% respectively among Pakistan population with CLBP [25]. The authors also reported a strong relation between gender and the incidence of both depression and anxiety. Soysal et al. [24] showed that BDI scores were significantly higher in CLBP patients than in chronic neck pain patients or a healthy control group. The current study also demonstrated significantly higher incidence of depression (51.5 vs 6.8%) and anxiety (42.5 vs 18.2%) in CLBP patients. The scores on self-evaluated questionnaires for depression and anxiety were also significantly higher in group P compared to group C. This result suggests that LBP for more than 3 months places patients at greater risk of experiencing depression and anxiety, as do other diseases which lead to the development of chronic pain. The associated symptoms of depression and anxiety such as inability to concentrate, disturbed sleep, pessimistic mood, fatigue and loss of motivation may give rise to adverse influences on a patient's treatment and recovery process.
The quality of life in CLBP patients has been examined at great length in many previous studies, and depression and anxiety are major factors affecting quality of life for patients with chronic musculoskeletal pain [13]. Boskovic et al. [18] insisted that patients with chronic lumbar radiculopathy had significantly lower scores on the SF-36 questionnaire on the physical domain while their scores on the mental domain remained similar to those of the general healthy control group. Soysal et al. [24] reported that the quality of life which was evaluated by the SF-36 including all subcategories among CLBP and chronic neck pain patients showed significant impairment compared to a healthy control group. In our results, the quality of life assessed by the SF-36 has shown significant impairment among the CLBP patients. The mean scores for groups P and C were 37.286 ± 2.461 and 67.035 ± 0.663 respectively. The eight subcategories have also shown significant differences, not only the physical subdomain but also the mental subdomain, which indicates that both physical and psychological functioning is impaired with CLBP patients.
The sleep disturbance in CLBP patients has also been described in numerous studies. Artner et al. [26] reported the sleep deprivation incidence of CLBP patients as 42.22%. Higher pain intensity, failed back surgery syndrome, and a migrational background were related to the sleep deprivation [26]. It was demonstrated that sleep was significantly impaired among CLBP patients [27], with a close relationship between pain severity and sleep disturbance [12]. However, in this study, no significant difference in the incidence of sleep disturbance was found between group P and group C. Also, the mean PSQI scores were similar between groups P and C, 8.331 ± 0.0637 and 6.556 ± 0.663 respectively. The result of this study in the aspect of sleep disturbance showed some discrepancy with previous studies. The probable reason for this result is that most of the participants in group P were diagnosed with spinal stenosis (82.98%) which has been shown to have no significant impact on the sleep disturbance [26]. Most patients with spinal stenosis do not complain of severe pain when in a lyingposition, but only when standing or walking. Therefore, this low level of pain with lying down might have little influence on sleep.
The correlation between disablility and depression, anxiety, and sleep disturbance has been well demonstrated by previous studies [6,9,28]. In addition, strong negative correlation between disability and quality of life has been reported [17]. According to our result, the correlation was found between ODI and BDI, BAI, and PSQI, using correlation analysis.
This result implies that the severity of depression, anxiety and sleep disturbance is proportional to the severity of disability, therefore, the intensity of pain including functional disability is directly related to the risk of causing depression, anxiety, and sleep disturbance. The duration of pain and the ODI score demonstrated a negative correlation with the SF-36. This result means that longer duration of pain and severity of disability shows inverse proportion with the quality of life.
Our study includes several important limitations. First, this study was performed in a single pain clinic with a small number of participants, so our results may not be generalizable. Second, our patient group did not include enough subgroups of CLBP, most participants were diagnosed with spinal stenosis, with a small number of patients with discogenic or facet joint problems. Third, the recruitment methodology showed several drawbacks with a relatively small sample size of both groups and unhomogenicity of the control group in their educational level. Fourth, our assessments of psychological status, sleep disturbance and SF-36 were obtained by participants' self-reported questionnaires, therefore, response bias could not be excluded.
Our findings suggest the importance of evaluating and managing the psychosocial illness and impairment in quality of life in CLBP patients and imply that these should be thought of as part of regular follow up. Psychological support and treatment is an important step in the patients with CLBP to minimize depression, and anxiety and improve quality of life. Although significant sleep disturbance was not found in CLBP patients in the current study, we still need to pay attention to the nature of sleep. A multidisciplinary approach including rehabilitation and psychiatry is critical to result in good therapeutic outcome.
Future investigations with large-scale samples are required to estimate generalizability, and systemic cohort studies aimed at diverse spine diseases in relation to psychosocial factors such as culture, ethnicity, and occupation would be beneficial.
References
1. Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999; 354: 581-585. PMID: 10470716.


2. Salvetti Mde G, Pimenta CA, Braga PE, Corrêa CF. Disability related to chronic low back pain: prevalence and associated factors. Rev Esc Enferm USP 2012; 46(Spec No): 16-23. PMID: 23250253.



3. Webb R, Brammah T, Lunt M, Urwin M, Allison T, Symmons D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine (Phila Pa 1976) 2003; 28: 1195-1202. PMID: 12782992.


4. Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, et al. The rising prevalence of chronic low back pain. Arch Intern Med 2009; 169: 251-258. PMID: 19204216.



5. Hagen EM, Svensen E, Eriksen HR, Ihlebaek CM, Ursin H. Comorbid subjective health complaints in low back pain. Spine (Phila Pa 1976) 2006; 31: 1491-1495. PMID: 16741460.


6. Guclu DG, Guclu O, Ozaner A, Senormanci O, Konkan R. The relationship between disability, quality of life and fear-avoidance beliefs in patients with chronic low back pain. Turk Neurosurg 2012; 22: 724-731. PMID: 23208904.


7. Polatin PB, Kinney RK, Gatchel RJ, Lillo E, Mayer TG. Psychiatric illness and chronic low-back pain. The mind and the spine--which goes first? Spine (Phila Pa 1976) 1993; 18: 66-71. PMID: 8434327.


8. Rush AJ, Polatin P, Gatchel RJ. Depression and chronic low back pain: establishing priorities in treatment. Spine (Phila Pa 1976) 2000; 25: 2566-2571. PMID: 11034638.


9. van de Water AT, Eadie J, Hurley DA. Investigation of sleep disturbance in chronic low back pain: an age- and gender-matched case-control study over a 7-night period. Man Ther 2011; 16: 550-556. PMID: 21652257.


10. Alsaadi SM, McAuley JH, Hush JM, Maher CG. Prevalence of sleep disturbance in patients with low back pain. Eur Spine J 2011; 20: 737-743. PMID: 21190045.


11. Grovle L, Haugen AJ, Ihlebaek CM, Keller A, Natvig B, Brox JI, et al. Comorbid subjective health complaints in patients with sciatica: a prospective study including comparison with the general population. J Psychosom Res 2011; 70: 548-556. PMID: 21624578.


12. Marin R, Cyhan T, Miklos W. Sleep disturbance in patients with chronic low back pain. Am J Phys Med Rehabil 2006; 85: 430-435. PMID: 16628150.


13. Börsbo B, Peolsson M, Gerdle B. Catastrophizing, depression, and pain: correlation with and influence on quality of life and health - a study of chronic whiplash-associated disorders. J Rehabil Med 2008; 40: 562-569. PMID: 18758674.


14. Celiker R, Borman P, Oktem F, Gökçe-Kutsal Y, Başgöze O. Psychological disturbance in fibromyalgia: relation to pain severity. Clin Rheumatol 1997; 16: 179-184. PMID: 9093801.


15. Lin EH, Tang L, Katon W, Hegel MT, Sullivan MD, Unützer J. Arthritis pain and disability: response to collaborative depression care. Gen Hosp Psychiatry 2006; 28: 482-486. PMID: 17088163.


16. Meeks TW, Dunn LB, Kim DS, Golshan S, Sewell DD, Atkinson JH, et al. Chronic pain and depression among geriatric psychiatry inpatients. Int J Geriatr Psychiatry 2008; 23: 637-642. PMID: 18041102.


17. Kovacs FM, Abraira V, Zamora J, Teresa Gil del Real M, Llobera J, Fernandez C, et al. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine (Phila Pa 1976) 2004; 29: 206-210. PMID: 14722416.


18. Bosković K, Todorović-Tomasević S, Naumović N, Grajić M, Knezević A. The quality of life of lumbar radiculopathy patients under conservative treatment. Vojnosanit Pregl 2009; 66: 807-812. PMID: 19938759.


19. Jeon CH, Kim DJ, Kim SK, Kim DJ, Lee HM, Park HJ. Validation in the cross-cultural adaptation of the Korean version of the Oswestry Disability Index. J Korean Med Sci 2006; 21: 1092-1097. PMID: 17179693.



20. Jo SA, Park MH, Jo I, Ryu SH, Han C. Usefulness of Beck Depression Inventory (BDI) in the Korean elderly population. Int J Geriatr Psychiatry 2007; 22: 218-223. PMID: 17044132.


21. Yook SP, Kim JS. A clinical study on the Korean version of Beck Anxiety Inventory: comparative study of patient and non-patient. Korean J Clin Psychol 1997; 16: 185-197.
22. Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M. Development of the Korean version of Short-Form 36-Item Health Survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med 2004; 203: 189-194. PMID: 15240928.


23. Sohn SI, Kim do H, Lee MY, Cho YW. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 2012; 16: 803-812. PMID: 21901299.


24. Soysal M, Kara B, Arda MN. Assessment of physical activity in patients with chronic low back or neck pain. Turk Neurosurg 2013; 23: 75-80. PMID: 23344871.


25. Sagheer MA, Khan MF, Sharif S. Association between chronic low back pain, anxiety and depression in patients at a tertiary care centre. J Pak Med Assoc 2013; 63: 688-690. PMID: 23901665.

26. Artner J, Cakir B, Spiekermann JA, Kurz S, Leucht F, Reichel H, et al. Prevalence of sleep deprivation in patients with chronic neck and back pain: a retrospective evaluation of 1016 patients. J Pain Res 2013; 6: 1-6. PMID: 23300350.


27. Marty M, Rozenberg S, Duplan B, Thomas P, Duquesnoy B, Allaert F. Quality of sleep in patients with chronic low back pain: a case-control study. Eur Spine J 2008; 17: 839-844. PMID: 18389288.



28. Tetsunaga T, Misawa H, Tanaka M, Sugimoto Y, Tetsunaga T, Takigawa T, et al. The clinical manifestations of lumbar disease are correlated with self-rating depression scale scores. J Orthop Sci 2013; 18: 374-379. PMID: 23443204.


Fig. 1
Comparison between quality of life in patients with group P (chronic low back pain patients for 3 months or longer) and group C (healthy control participants). All 8 subscales of Short Form 36 Item Health Survey (SF-36) demonstrated significant lower scores in group P compared to group C.
- TOOLS