 |
 |
|
|
Living donor liver transplantation (LDLT) across ABO-incompatible blood types used to be discouraged because of the increased risk of acute and antibody-mediated rejection, graft loss, infection, and poor subsequent clinical outcomes. Several strategies for overcoming ABO-incompatible LDLT, such as plasmapheresis, splenectomy, rituximab, mycophenolate mofetil, and intravenous immunoglobulin (IVIG), have reduced ABO incompatibility-related complications [1]. However, little is known about combined ABO- and Rh-incompatible LDLT. We here describe a successful LDLT procedure that was performed between an O Rh- patient with hepatocellular carcinoma (HCC) and a B Rh+ donor.
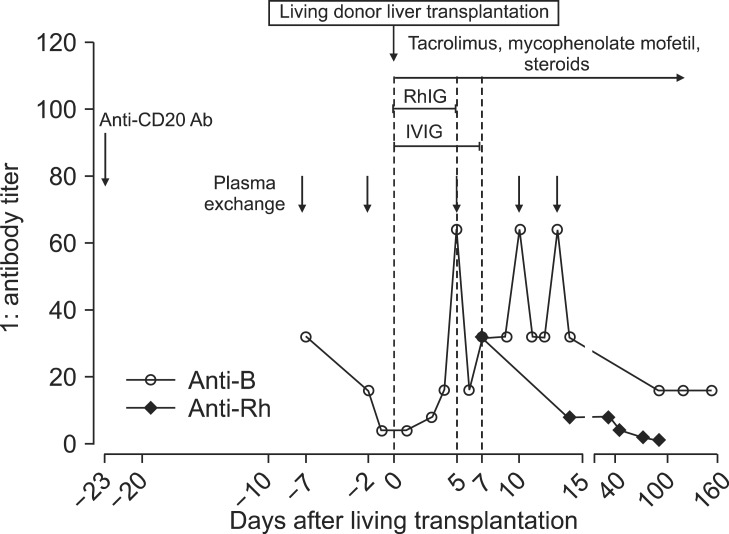
The patient was a 45-year-old man whose blood type was O Rh-. He presented with a history of hepatitis B and HCC. His Child-Pugh score was 6 points (class A), and his Model for End-Stage Liver Disease score was also 6 points. Three weeks before LDLT, 546 mg (300 mg/m2) rituximab (MabThera; Roche, Basel, Switzerland), a monoclonal antibody raised against CD20, was administered once (Fig. 1). Plasma exchange (PE) was performed two and seven days before transplantation. His initial anti-B titer was 1 : 32, but fell to 1 : 4 on the day of LDLT (Fig. 1).
In accordance with our institution's anesthetic protocol for LDLT, general anesthesia was administered in the following order: induction of thiopental sodium, fentanyl, and vecuronium; mechanical ventilation after endotracheal intubation; and maintenance with sevoflurane, fentanyl, and vecuronium. During the procedure, electrocardiography, pulse oximetry, end-tidal carbon dioxide, and cerebral oximetry were monitored. Hemodynamic parameters were monitored by measuring the invasive arterial pressure, central venous pressure, and pulmonary arterial pressure. Because the volume of the right hepatic lobe was 814 ml and the remnant liver volume was 30% on donor liver volumetry determined using computerized tomography, LDLT was performed using a right lobe graft from the patient's son, whose blood type (B Rh+) was incompatible with the patient (O Rh-). The graft-to-recipient bodyweight ratio was 1.095 (0.8 kg/73 kg × 100). No incompatible nor allergic blood transfusion reactions were observed after 2 units of O- packed red blood cells (RBC), 1.5 units of B+ fresh frozen plasma (FFP), and 10 units of B+ cryoprecipitate were intraoperatively administered. The transplantation was uneventful, and the patient was transferred to the surgical intensive care unit.
Postoperatively, 3000 IU Rho(D) immunoglobulin (RhIG; WinRho SDF; Cangene, Winnipeg, Canada) was intramuscularly administered on the day of the transplantation and on each of the following four days after the operation (Fig. 1). In addition, 500 IU RhIG was administered on day 7 after the operation because eight units of B+ platelet concentration (PC) was transfused on that day. The routine administration of immunosuppressive agents consisting of tacrolimus, mycophenolate mofetil, and steroids was also commenced (Fig. 1). IVIG was administered on the day of transplantation and for the following seven days (Fig. 1). PE was performed 5, 10, and 13 days after surgery and anti-B titers remained < 1 : 16 over the following 160 days after the operation (Fig. 1). The patient was discharged without complications, and his hepatic and hematologic findings were within acceptable ranges through the five month period after LDLT.
In ABO-incompatible LDLT, several studies report that the use of monoclonal antibodies against CD20- B cells, high-dose IVIG, and PE are important strategies for preventing allograft rejection and reducing the isoagglutinin titer [2]. In our current case, rituximab was administered once at three weeks before LDLT to induce B-cell depletion [2]. PE was performed 2 and 7 days before and then 5, 10, and 13 days after LDLT to decrease the ABO-incompatible antibody titer [3]. IVIG was administered from the day of transplantation and throughout the seven day period post-operation to prevent rebounding of the isoagglutinin titer [3]. In addition, routine immunosuppressive agents consisting of tacrolimus, mycophenolate mofetil, and steroids were immediately started after LDLT.
In addition to ABO incompatibility, Rh incompatibility between the donor and recipient might have been another issue in our current case of LDLT. There is documented evidence to suggest that leukoreduction or immunosuppression might decrease the risk of alloimmunization to RBC antigens. Some of the reported low rates of D-alloimmunization occurred in patients who received D-mismatched transfusions and immunosuppressive drugs during liver transplantation [4]. Because even a small amount of residual D+ RBC can cause alloimmunization, prophylactic 3000 IU RhIG was intramuscularly administered on the day of transplantation in our present case and over the following four days; 3000 IU RhIG was expected to suppress the immunizing potential of the 30 ml aliquot of D+ RBC. The Rh antibody titer was checked every week post-operation. The initial Rh antibody titer was 1 : 32 at seven days postoperation and remained at 1 : 2 for two months.
Blood transfusions should be carefully administered during Rh-incompatible LDLT. Transfused RBC should be Rh-compatible with the recipient's blood type. PC, FFP, and cryoprecipitate, on the other hand, should be Rh-compatible with the donor's blood type. Prophylactic RhIG is recommended for treating Rh+ RBC contamination in PC, which can lead to alloimmunization. However, the transfusion of FFP or cryoprecipitate does not require prophylaxis. In our present patient, 500 IU RhIG was administered for B+ PC transfusion on day 7 after the operation based on the assumption that eight units of PC would contain about 5 ml Rh+ RBC [5].
In conclusion, we performed a successful ABO- and Rh- incompatible LDLT between an O Rh- recipient and B Rh+ donor. In addition to applying important interventions when performing ABO-incompatible LDLT, such as administering monoclonal antibodies against CD20- B cells, PE, and high-dose IVIG, RhIG should also be administered to prevent D-alloimmunization because of the possibility of residual D+ RBC in the graft and PC.
References
1. Egawa H, Tanabe K, Fukushima N, Date H, Sugitani A, Haga H. Current status of organ transplantation in Japan. Am J Transplant 2012; 12: 523-530. PMID: 22054061.


2. Ikegami T, Taketomi A, Soejima Y, Yoshizumi T, Uchiyama H, Harada N, et al. Rituximab, IVIG, and plasma exchange without graft local infusion treatment: a new protocol in ABO incompatible living donor liver transplantation. Transplantation 2009; 88: 303-307. PMID: 19667930.


3. Raut V, Uemoto S. Management of ABO-incompatible living-donor liver transplantation: past and present trends. Surg Today 2011; 41: 317-322. PMID: 21365409.


4. Casanueva M, Valdes MD, Ribera MC. Lack of alloimmunization to D antigen in D-negative immunosuppressed liver transplant recipients. Transfusion 1994; 34: 570-572. PMID: 8053037.


5. Menitove JE. Immunoprophylaxis for D- patients receiving platelet transfusions from D+ [correction of D-] donors? Transfusion 2002; 42: 136-138. PMID: 11896325.


Fig. 1
Treatment for ABO-incompatible transplantation consisted of the use of monoclonal antibodies against CD20 (rituximab), plasma exchange, intravenous immunoglobulin (IVIG), and immunosuppressants. The initial anti-B titers were 1 : 32; after plasma exchange, the anti-B titer was 1 : 4 during transplantation. Plasma exchange was performed three times postoperatively and the anti-B titer remained at < 1 : 16 for 160 postoperative days. Rho(D) immunoglobulin (RhIG) was administered to prevent D-alloimmunization on the day of the transplantation and throughout the following four days post-operation.
- TOOLS








