|
 |
|
|
Abstract
An 86-year-old female with a history of right rotator cuff injury was admitted for arthroscopic shoulder surgery under general anesthesia. There were no remarkable immediate postoperative complications. However, while recovering in the general ward, she developed dyspnea with hypoxia. She was immediately treated with oxygen, and antibiotics after pneumomediastinum was confirmed on both chest x-ray and chest computed tomography. Subcutaneous emphysema on either face or neck followed by arthroscopic shoulder surgery was common, but pneumomediastinum with hypoxia is a rare but extremely dangerous complication. Thus we would like to report our case and its pathology, the diagnosis, the treatment and prevention, with literature review.
Respiratory complications such as pneumothorax and pneumomediastinum following arthroscopic shoulder surgery are rare but serious complications that required aggressive treatment.
An 86-year-old female patient underwent arthroscopic shoulder surgery for right rotator cuff injury and transferred to general ward after full recovery from general anesthesia at the post anesthetic care unit (PACU). Approximately 5 hours after the surgery, pneumomediastinum was developed.
While reviewing this case, we address the pathology, the diagnosis, the treatment and the prevention of pneumomediastinum occurring after arthroscopic shoulder surgery, including a literature review.
An 86-year-old female patient with right rotator cuff injury was admitted for arthroscopic shoulder surgery under general anesthesia. The patient was 148 cm in height and 54 kg in weight, with hypertension controlled by medication, and otherwise generally healthy condition. The physical examination and laboratory finding including a chest x-ray taken for preoperative evaluations were normal and pulmonary function was normal.
No premedication was given. Initial blood pressure was 170/85 mmHg, heart rate 67 beats/min, oxygen saturation 97%, and body temperature 36.0℃. Thiopental 250 mg, lidocaine 40 mg, and rocuronium 40 mg were administered intravenously. Endotracheal intubation was done successfully without complication. After intubation, the lung sound on both lung fields was remarkable and tube was fixed at 21 cm. For maintenance of anesthesia, oxygen 2 L/min, N2O 2 L/min, sevoflurane (1.2-2.0 vol%) were administered, and remifentanil was continuously infused 0.1-0.2 µg/kg/min. Volume-control ventilation was maintained with a tidal volume of 450 ml, with respiration rate of 12/min. Airway pressure was maintained to 20 cmH2O, whereas partial pressure of end-tidal carbon dioxide (PETCO2) was kept to 35-38 mmHg. When one hour passed after induction, PETCO2 was reduced to 32 mmHg and tidal volume and respiration rate were controlled to 450 ml and 10/min respectively. Airway pressure was maintained to 19 cmH2O.
The patient's position during surgery was a beach chair position. Blood pressure and heart rate were maintained 100-130/60-80 mmHg and 54-85 beats/min, respectively; there were no remarkable events throughout the entire surgical procedure. After the surgery, pyridostigmine 15 mg and glycopyrrolate 0.4 mg were given for reversal of muscle relaxation. Extubation was achieved after confirmation of self-respiration and consciousness recovery. The patient was transferred to the PACU. Total operation time was 145 minutes and, whereas total anesthesia time was 175 minutes. In the PACU, she had no any complaints and patient's oxygen saturation was maintained at 97% in room air for 10 minutes. She was transferred to the general ward. Postoperative pain control was achieved by fentanyl 800 µg and ketorolac 90 mg along with ramosetron 0.3 mg mixed to normal saline 80 ml. A patient-controlled analgesia device (Accufuser Plus®, Woo Young Medical, Korea; flow rate 1 ml/hr, bolus volume 1 ml, lock out time 15 min) was employed to deliver the medication intravenously for pain control.
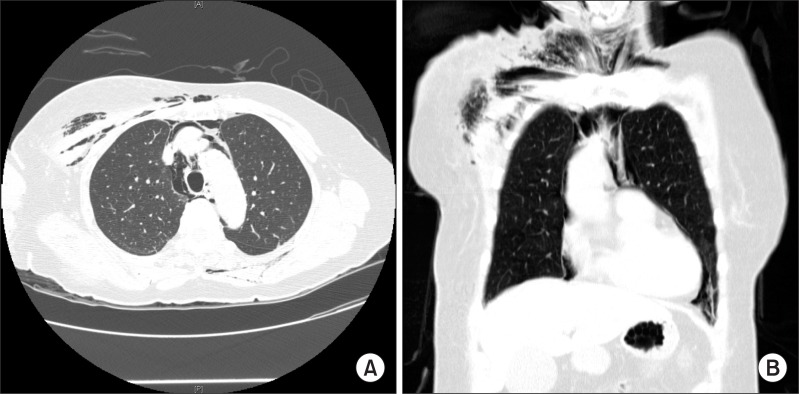
At 5 hours after the end of surgery, she complained of facial edema with a lot of sputum tingeing with a small amount of blood. Vital signs were 160/80 mmHg for blood pressure, 98 beats/min for heart rate, 36.3℃ for body temperature and 96% for oxygen saturation. After 30 minutes, she complained of severe respiratory difficulty and the oxygen saturation was decreased to 91-95%. 3 L/min of oxygen was supplied immediately by nasal cannula, and then the saturation on the pulse oximetry was maintained to 98%. A chest x-ray and a chest CT scan were taken for evaluation of dyspnea. On chest x-ray (Fig. 1) and chest CT scan, it was discovered that there were subcutaneous and intermuscular emphysema on the patient's face and neck, and pneumomediastinum (Fig. 2). Fiberoptic bronchoscopic examination was performed by an otolaryngologist with the patient in a waking state, and there were no remarkable findings except a mild laceration in the oral cavity.
Pneumomediastinum was confirmed so that an antitussive agent, antibiotics and 5 L/min of oxygen were administered for treatment. The patient's symptoms were improved on post-operative day 2, and oxygen supply was removed on post-operative day 3. She was discharged on post-operative day 7.
Postoperative pneumomediastinum can arise from several causes including spontaneous pneumomediastinum, complication by underlying disease, complication related to surgical procedure, and anesthetic complications.
Spontaneous pneumomediastinum can occur from rigorous exercise, spontaneous cough, and severe vomiting and it can be explained as increase of intra-alveolar pressure in these conditions which can induce alveolar rupture by pressure difference [1]. This condition is often observed when actively pushing a baby during the second stage of labor [2].
A pathologic situation such as mediastinitis can result in pneumomediastinum by a gas-forming microorganism during the infectious process or by direct-gas inflow to mediastinum by traumatic disruption of either cutaneous or mucosal barriers [3].
Pneumomediastium has been noted following orthognatic surgery [4], tonsillectomy [5], vesico-urethral reimplantation operation [6]. Subcutaneous and intermuscular emphysema, and pneumomediastinum following arthroscopic shoulder surgery have rarely been reported [7,8].
Lee et al. [7] reported three cases of subcutaneous emphysema and pneumomediastinum, partial lung collapse, and tension pneumothorax following arthroscopic shoulder surgery under general anesthesia. Calvisi et al. [8] discovered subcutaneous emphysema and pneumomediastinum after the shoulder arthroscopy under brachial plexus block. Improper size and position of endotracheal tube, sudden head position change during endotracheal intubation or anesthesia, and laryngeal, tracheal and bronchial injuries by other manipulations can be causes related to general anesthesia [9]. High tracheal pressure during anesthesia, alveolar damage due to high tracheal pressure by cough or vomiting when recovering from anesthesia and air leakage derived by alveolar damage can be other reasons [10].
In our case, tracheal or bronchial laceration was excluded as possible causes of pneumomediastinum since there were no other findings beyond mild laceration in the oral cavity. Perioperative airway pressure was maintained to less than 20 mmHg. Severe vomiting, cough or upper respiratory tract obstruction after anesthesia was not observed. Post-operative pneumothorax caused by either alveolar rupture or lung injury was also not considered. Therefore, other causes must be considered.
In arthroscopic shoulder surgery, the subarcromial space is dilated by fluid pressure through the arthroscopy infusion pump for good visualization. An infusion pump device works to maintain regular pressure with intermittent operation. When the power shaver applies frequent suction, the pressure in the subacromial space transiently drops and becomes negative pressure at that moment. Under this negative pressure, air may be trapped in the space through a lateral portal. Furthermore, the positive pressure by the infusion pump may deliver air into the surrounding tissue that can develop into subcutaneous emphysema if the power shaver is turned off [7].
The soft tissue structure of the neck is divided into three distinctive compartments: the previsceral, visceral and prevertebral space. The prevertebral space is connected laterally to axillary sheath and posterior angle of the neck. Both previsceral and prevertebral compartment terminate in upper part of thoracic spine and usually do not extend into mediastinum [3]. However, air can travel along through the axillary sheath to produce pressure in prevertebral space, then the prevertebral fascia becomes separated and air may be trapped into the mediastinum, which eventually produces pneumomediastinum [11]. Considering our patient's advanced age, pneumomediastinum may be related to tissue loosening caused by aging process. However, Lee et al. [7] and Calvisi et al. [8] presented patients in their 40s and 50s respectively, indicating less relation between the patient's age and occurrence of pneumomediastinum.
Although the relation between the patient's operating position and the risk of pneumothorax or pneumomediastinum is not clear [7], in the previous articles that reported post-operative pneumomediastinum, most operating positions were upright positions, such as lateral decubitus position or relatively sitting position. In our patient's case, the operating position was also a sitting position. The recent trend for arthroscopic shoulder surgery is the sitting position for good visualization of operating fields; therefore the relationship of pneumomediastinum to the position may be a serious problem. But, other articles reported that pneumomediastinum has been developed with other positions [4-6]. Therefore, operative position is less associated with pneumomediastinum. More studies about the relationship between the operating positions or operation types and the development of pneumomediastinum are needed.
The clinical symptoms of post-operative pneumomediastinum were chest pain, dyspnea, cough, fever, palpitation and cyanosis in severe cases [12]. The diagnosis is usually based on image studies like chest x-ray and CT scan. Esophagoscopic examination and esophagogram is employed to confirm esophageal rupture, and fiberoptic bronchoscopic examination is performed to check tracheobronchial rupture. In this case, esophagoscopic examination was not performed because there was no evidence of esophageal injury in the patient history, and no symptoms such as cough and vomiting.
Treatments for pneumomediastinum are to manage the main causes of the disease itself while providing supportive care. This entails 100% oxygen supply via non-rebreathing face mask, analgesics for pain control and antibiotics to prevent mediastinitis. The symptoms are generally expected to abate within 1 to 3 hospital days. Some researches note that 100% oxygen supplement would give better air absorption by nitrogen concentration gradient within pneumomediastinum [13], so our patient was treated 5 L/min of oxygen for three days with both antibiotics and analgesics. She was discharged after fully recovering without any other complications.
To minimize post-operative respiratory complications such as pneumomediastinum and pneumothorax, the following are recommended to orthopedic surgeons who perform arthroscopic shoulder surgery. These recommendations should be considered by anesthesiologists as well. Systolic blood pressure of around 100 mmHg and infusion pump pressure about 40 mmHg may help to decrease intraoperative bleeding and reduce risk of fluid extravasation. Nevertheless, if the patient complains respiratory symptoms after surgery, physical and imaging evaluation as described must be performed immediately [8].
In conclusion, in arthroscopic shoulder surgery, pneumomediastinum may occur due to actual physical damage such as esophageal laceration or tracheal rupture, as well as from the surgeon's manipulation during or after the surgery. This can be prevented by adequate management of surgical procedures. If the symptoms develop, prompt diagnosis and treatment is urgent.
References
1. Rose WD, Veach JS, Tehranzdeh J. Spontaneous pneumomediastinum as a cause of neck pain, dysphagia, and chest pain. Arch Intern Med 1984; 144: 392-393. PMID: 6696577.


2. Baillie S, Newbury J. Pneumomediastinum and subcutaneous emphysema in labour: Two case reports. Aust N Z J Obstet Gynaecol 2009; 49: 697-698. PMID: 20070728.


3. Maunder R, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med 1984; 144: 1447-1453. PMID: 6375617.


4. Kim T, Kim JY, Woo YC, Park SG, Baek CW, Kang H. Pneumomediastinum and pneumothorax after orthognatic surgery, a case report. Korean J Anesthesiol 2010; 59: S242-S245. PMID: 21286451.



5. Kim JP, Park JJ, Kang HS, Song MS. Subcutaneous emphysema and pneumomediastinum after tonsillectomy. Am J Otolaryngol 2010; 31: 212-215. PMID: 20015746.


6. Kim JB, Lee JM, Im KS, Kim DY, Hong SH, Jung HJ. Spontaneous subcutaneous emphysema and pneumomediastinum after vesico-urethral reimplantation under general anesthesia. Korean J Anesthesiol 2006; 51: 116-119.

7. Lee HC, Dewan N, Crosby L. Subcutaneous emphysema, pneumomediastinum, and potentially life-threatening tension pneumothorax. Pulmonary complications from arthroscopic shoulder decompression. Chest 1992; 101: 1265-1267. PMID: 1582282.


8. Calvisi V, Lupparelli S, Rossetti S. Subcutaneous emphysema and pneumomediastinum following shoulder arthroscopy with brachial plexus block: a case report and review of the literature. Arch Orthop Trauma Surg 2009; 129: 349-352. PMID: 18283470.


9. Yoon YC, Kim SJ, Jeong CW, Bae HB, Kwak SH. Tracheal laceration found after endotracheal general anesthesia, case report. Anesth Pain Med 2009; 4: 83-86.
10. Smelt GJ. Subcutaneous emphysema: pathological and anaesthetic, but not surgical. J Laryngol Otol 1984; 98: 647-654. PMID: 6736764.


11. Lau KY. Pneumomediastinum caused by subcutaneous emphysema in the shoulder. A rare complication of arthroscopy. Chest 1993; 103: 1606-1607. PMID: 8486054.


12. Chon SH, Wee JS, Lee CB, Kim H, Kim YH. Clinical analysis of spontaneous pneumediastinum. Korean J Thorac Cardiovasc Surg 2006; 39: 56-59.
13. Kim DH, Park JH, Chei CS, Hwang SW, Kim HY, Yoo BH. Spontaneous pneumomediastinum: clinical investigation. Korean J Thorac Cardiovasc Surg 2006; 39: 220-225.
- TOOLS