|
 |
|
|
Abstract
Background
The purpose of this study is to compare the anesthetic characteristics in elderly patients who remain in sitting position for 2 min compared with patients that are placed in supine position after induction of spinal anesthesia.
Methods
Fifty-seven patients scheduled for transurethral surgery were randomized to assume supine position immediately after 6.5 mg hyperbaric bupivacaine were injected (L group) or to remain in the sitting position for 2 minutes before they also assumed the supine position (S group). Analgesic levels were assessed bilaterally, using pin-prick. Motor block was scored using a 12-point scale. The mean arterial pressure and heart rate were also recorded.
Results
Sensory block levels were significantly lower at all time points for the L group. However, there were no significant differences in the degree of the motor block and hemodynamic changes between the two groups. However, in the L group, ephedrine or atropine were administered to three patients.
As the average life span has been recently increased due to an advancement of medical service quality and the rise of attention on health conditions, the aging population started to rapidly increase. Korea is now regarded to have entered an era of aging society, as of after 2000; according to 10.7% of proportion of the senior aged more than 65 out of total population recorded in 2009 that was increased by 3.8% from 6.9% 10 years ago [1]. Hereupon, it is required to properly consider advantages and disadvantages between general anesthesia and regional anesthesia, and to provide an understanding of anatomy, pharmacological changes of medicine, and physiological changes of old age in order to reduce the frequency of complications or after effects of surgery or anesthesia, since an increase of aging population serves as a major risk factor for increasing the number of patients suffering from chronic diseases and perioperative mortality [2].
Spinal anesthesia uses only a small amount of local anesthetics compared to the one needed for epidural anesthesia, and entails relatively simple procedures and fast onset of effect from anesthesia. In addition, the rate of occurrence of thromboembolism and cardiovascular complications is reduced after surgery, compared to the general anesthesia and the amount of blood transfusion and hemorrhage in perioperative period, leading to a decrease in the rate of pneumonia and respiratory failure in case of patients suffering from chronic lung diseases [3]. Therefore, in general cases, spinal anesthesia is most likely selected for surgery of urology for elderly patients.
For the elderly patients, dermatome is more extended and duration is prolonged. In addition, this frequently causes hypotension and bradycardia [4]. Such cardiovascular changes serve as a major reason for increasing the rate of morbidity and mortality. Therefore, it is required to consider a safe method for anesthesia that can maintain perioperative and postoperative hemodynamic stability.
Therefore, this study is intended to compare the level of sensory block, motor block and hemodynamic changes of elderly patients who remain in sitting position for 2 min compared with patients that are placed in supine position after given a low dose of bupivacaine.
After hospital ethics committee's approval and written informed consent, American Society of Anesthesiologists physical status I-II patients, aged 65 years and above, scheduled for transurethral (prostate or bladder tumor) surgery under spinal anesthesia were included in this prospective, randomized, double-blind study. Patients with other neurological diseases, spine abnormalities or absolute or relative contraindication on spinal anesthesia were excluded from this study.
All patients were premedicated with glycopyrrolate 0.2 mg intramuscular. Ringer's lactate solution or normal saline, 8 ml/kg, was administered intravenously over a period of approximately 30 minutes. According to routine procedure, standard monitoring was used throughout the intraoperative period, including continuous ECG, heart rate, and non-invasive arterial blood pressure measured every five minutes, and continuous pulse oximetry.
Patents have randomly been divided into the L group (n = 29) and S group (n = 28). In the L group, patients underwent spinal anesthesia in lateral decubitus position. In the S group, spinal anesthesia was performed with the patient in sitting position. A midline lumbar puncture was performed using a 25-gauge Quincke spinal needle at L3-4 or L4-5 level. After confirming the CSF flow, spinal injection of 6.5 mg of 0.5% Bupivacaine (Marcaine®, AstraZeneca, Sweden) was performed over 10-15 s in both groups. Patients in the L group have been lied down immediately after injecting the solution, while those in the S group have maintained a seating position for two minutes and then lied down. Procedure has been carried out by one anesthesiologist and evaluated by another anesthesiologist that had not proceeded with spinal anesthesia and without having any knowledge of the experimental groups.
Five minutes after subarachnoid injection, patients have been evaluated for twenty minutes, in five-minute intervals, in the degree of sensory and motor block. Sensory block level has been evaluated in pin-prick test for both sides by using a 25G needle. Assessments of motor block were made immediately after the assessment of the analgesia. For motor block, it has been evaluated whether patients could flex hip, knee and ankle joints. It was rated per joint (0 = no, 1 = partial, 2 = complete motor block). The results obtained in both extremities were added, giving it a maximum score of 12.
If blood pressure was lower than 90 mmHg or reduced more than 20%, compared to the initial blood pressure as a hypotension, ephedrine was given if there was no change in the blood pressure after waiting for five minutes. If pulse rate was recorded lower than 50/min, it was regarded to be a case of bradycardia that 0.5 mg of atropine was given. The mean arterial pressure and pulse rate that have been compared were recorded at 5-minute intervals. The level of sensory block, motor block score, hypotension, bradycardia and the use of ephedrine and atropine were compared. For satisfaction of patients and surgeons, four grades were classified: excellent, good, fair, and poor. That evaluated the satisfaction of surgeons immediately after the surgery and patients right before coming to the ward.
SPSS (version 19.0, SPSS Inc, USA) has been used for statistical evaluation, and all data are expressed as the mean ┬▒ standard deviation. Age, weight, height, duration of procedure, the level of sensory block, the degree of motor block, and the peak sensory level were analyzed and compared using student t-test. The level of sensory block, degree motor block, mean arterial pressure, and pulse rate over time in both groups have been compared using repeated measures of ANOVA. Technical difficulty, hypotension, bradycardia, and whether to inject ephedrine and atropine were all compared using Fisher's exact test, and P value < 0.05 was considered statistically significant.
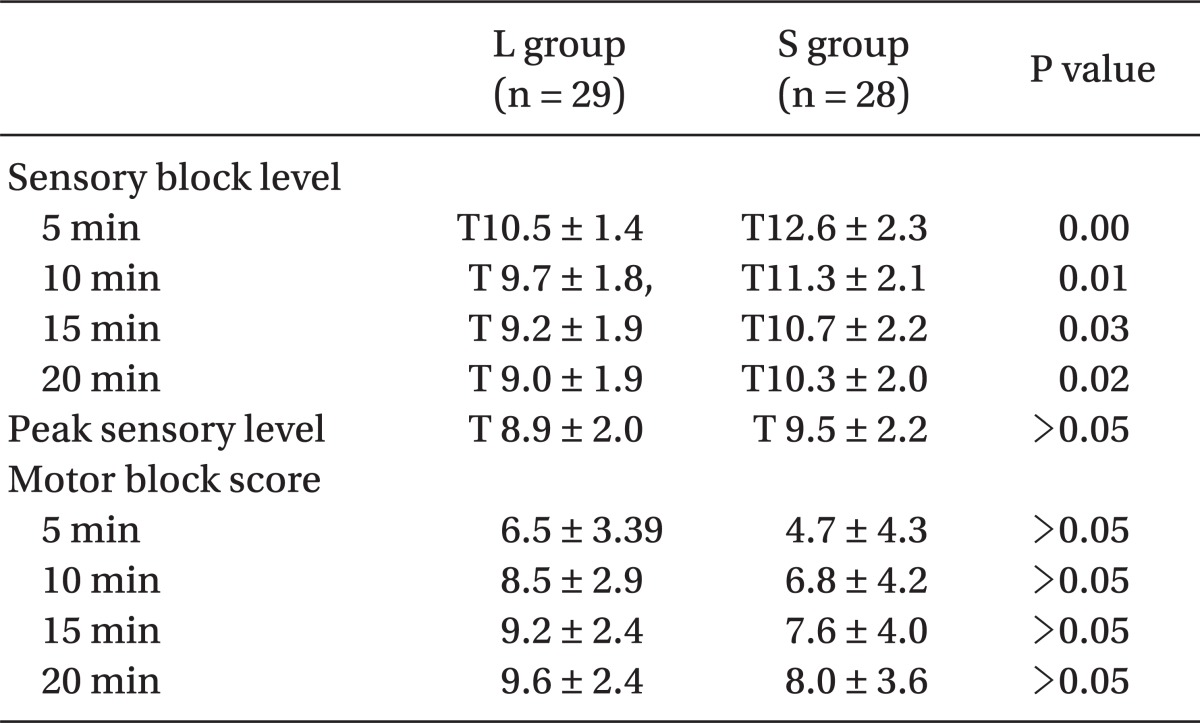
There was no significant differences on the age, weight, height, gender ratio, and duration of procedure (Table 1). Sensory block levels were significantly lower at all time points for the L group (P < 0.05). However, there were no significant differences in the changes of the level of sensory block between the two groups. In addition, there was no statistically significant difference on two groups in the peak sensory level and also on the motor scores on two groups in each time interval. In addition, there were no significant differences or changes in the degree of motor block in each time interval on both groups (Table 2).
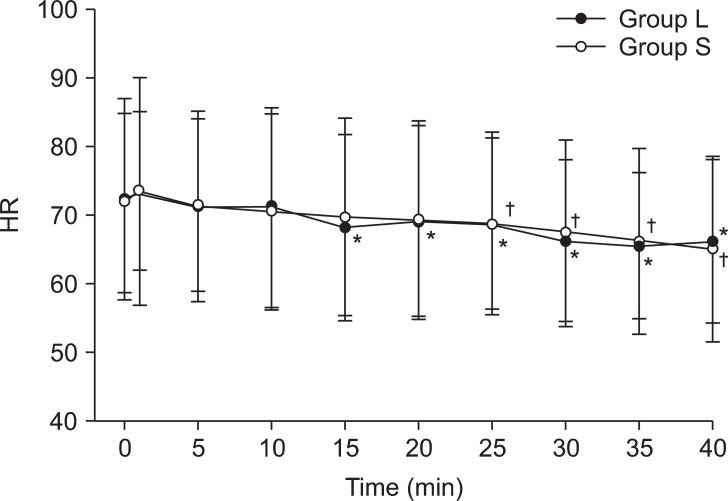
There was a decreasing trend on the mean arterial pressure and pulse rate after spinal anesthesia, but there were no significant differences on both groups in each time interval. However, as for mean arterial pressure, there was a trend of blood pressure starting to reduce five minutes after giving local anesthetics, followed by recovery after forty minutes in the L-group. In the S group, there was no such trend of decreasing blood pressure compared to that of the initial blood pressure (Fig. 1). In regards to the pulse rate, the L and S groups have shown significant differences after 15 minutes and 25 minutes, respectively (Fig. 2). In the L group, one patient had hypotension and bradycardia at the same time that ephedrine was injected, and two patients were with bradycardia that atropine was given. However, there was no statistically significant difference (Table 3). In addition, there was no significant difference satisfaction of patients and surgeons (Table 4).
The level of sensory block, followed by injection of local anesthetics, was influenced by various factors, including age, height, a concentration and gravity of local anesthetics, posture of patients, bevel direction of needles, and repetitive injection in spinal anesthesia [5]. If giving local anesthetics on young adults, then the analgesic level and an amount of anesthetics had relatively fixed proportions. However, degenerative changes of the central and peripheral nervous system [6], anatomical changes of lumbar and the thoracic vertebrae [7], and reduction of cerebrospinal fluid [8], sensory block level, followed by spinal anesthesia, which was shown 3-4 segments higher on the elderly patients that are aged > 65 compared to that of young patients [9-11]. The neurological changes, followed by an increase of the age, can influence the quality and period of sensory block and the required amount of local anesthetics.
An increase of the age and a high level of sensory block are major reasons for hypotension after spinal anesthesia. Hypotension is occurred due to the sympathetic nerve block that is 2-4 segments higher than the level of sensory block. According to Lee et al. [12], the ratio of occurrence of hypotension on the elderly patients aged more than 70 were 48%, which turned out to be significantly higher than the patients aged less than 60 by 4.2% after using 7 mg of 0.5% heavy bupivacaine. Therefore, the level of the sympathetic nerve block is important in the clinical perspective. It is important not to unnecessarily increase the height of block on the spinal anesthesia on the elderly patients. The advantage of using hyperbaric local anesthetic solutions is flexibility of controlling the level with posture. However, it is still controversial in terms of time period needed for seating position in order to restrict the height of anesthesia.
There are relatively insufficient amount of study in clinical influence on spinal anesthesia, compared to a fact that the extensive spread of sensory block and fast onset if giving epidural anesthesia for the elderly with bupivacaine. However, in spinal anesthesia, all different results have been reported in spread of sensory block. According to Racle et al. [9] that used hyperbaric bupivacaine, the onset of sensory block was faster in the group of elderly, but Veering et al. [10] have said that it became even more wide spread as the maximum sensory block period was delayed. In addition, previous studies have been carried out by using a large amount of bupivacaine on people in Western countries, who were tall, but there was a difficulty on applying them on people in Asian countries. We have confirmed that there was no difficulty in carrying out the surgery by using low-dose bupivacaine through the pilot study. Therefore, this study is intended to compare a degree of sensory and motor block, and hemodynamic changes of the elderly patients between maintaining a sitting position for two minutes after being given low dose bupivacaine at sitting position and lying immediately after injecting local anesthetics at lateral decubitus position. In the past, Sise [13] had insisted that the anesthetics started diffusing within two minutes after injection and completed diffusing within five minutes, providing almost no influence on blocked level even if the local anesthetics moved after these periods. However, according to the study conducted by Veering et al. [10], there was no difference of the degree of sensory and motor block on the group of patients taking a sitting position for two minutes even if they maintained a sitting position up to twenty minutes after spinal anesthesia. In this study, there was a significant difference on the level of sensory block on both groups, but no difference on a degree of motor block. In addition, there was no significant difference on the satisfaction of patients and surgeons on both groups. However, as the study has been proceeded by injecting low dose local anesthetics that did not influence on the satisfaction of patients and maintain hemodynamic stability, there was a case of entailing lower height compared to the one known to be proper for the surgery. There was a case that one patient from the L group suffered from inconvenience leading to inject 30 ug fentanyl for the smooth procedures of surgery. Therefore, it seems that proceeding the study with an increase amount of local anesthetics might be helpful to determine proper amount of anesthetics in a clinical environment.
Transurethral prostatectomy and bladder tumor resection has T10 segments for proper height of sensory block, and time needed for most of surgeries is within one hour. Therefore, it might be idealistic to maintain hemodynamic stability with fast recovery rate from anesthesia by keeping T10 of sensory block on spinal anesthesia for the elderly patients. In this study, the mean arterial pressure and pulse rate have been decreased after spinal anesthesia on both groups, but there was no difference from time interval on both groups. However, there was no hypotension or bradycardia at all on the group of patients maintaining a sitting position for two minutes, but three patients from the group taking a supine position required an injection of ephedrine and atropine. Even if there was no significant difference in both groups, if a sympathetic nerve block from spinal anesthesia caused hypotension, it might increase a chance of inefficient compensation, unlike young patients since the deterioration of function on autonomic nervous system differs by individuals. Therefore, it is expected that maintaining a sitting position for two minutes after spinal anesthesia is helpful for the elderly patients considering the safety of patients.
According to Kawamoto et al. [14], the increase of activation from parasympathetic nervous system after spinal anesthesia started to be shown after three minutes, while the activation of sympathetic nervous system started to be decreased after six minutes and maintained afterwards. They also insisted that blood pressure and pulse rate have been reduced at the same time, and the balance of autonomous nervous system was closely related to the level of sensory block. Hemmingsen et al. [15] have reported that the onset of hypotension was ten to fifteen minutes after spinal anesthesia. However, according to study conducted by Critchley et al. [16] dealing with the elderly patients, the blood pressure requiring treatment started within six to nine minutes. In our study, the blood pressure from the group of taking a sitting position started to be significantly reduced after five minutes compared to the initial blood pressure. However, it seems that severe hypotension requiring treatment had not been occurred since a small amount of bupivacaine was used.
Preference of anesthesiologists and patients physiological condition of patient, the gravity of local anesthetics influence the determination of posture needed for spinal anesthesia. In fact, the gravity of local anesthetics and posture of patients are closely related [8]. According to our study, there was no significant difference on the duration of procedure needed for both groups. However, number of needle insertion for spinal anesthesia was significantly more in patients from a supine position group than in patients from a sitting position for two minutes. It seems that anatomical changes of lumbar and thoracic vertebrae [7] and poor compliance for lateral decubitus position in elderly patients. In spinal anesthesia, on the elderly patients, an effort should be exerted to avoid unnecessary increase of a level of anesthesia and to secure the safety. Hereupon, in anesthesia on the elderly patients in a clinical environment, it is feasible to adjust the height of block in an appropriate level for surgery by controlling the time of maintaining a sitting position after injecting low dose local anesthetics and these results was helpful to maintain perioperative hemodynamic stability of patients.
References
1. Korea National Statistical Office. 2010 aged statistics. 2010, Daejeon, Statistics Korea. pp 14-24.
2. Forrest JB, Rehder K, Cahalan MK, Goldsmith Ch. Multicenter study of general anesthesia III: Predictors of severe adverse outcomes. Anesthesiology 1992; 76: 3-15. PMID: 1729933.

3. Kleinman W, Mikhail M. Edited by Morgan GE, Mikhail M, Murray MJSpinal, epidural & caudal blocks. Clinical anesthesiology. 2005, 4th ed. : New York, McGraw-Hill. pp 290-291.
4. Longnecker DE, Murphy FL. Introduction to anesthesia. 1997, 9th ed. Philadelphia, WB Saunders. pp 365-376.
5. Brown DL. Edited by Miller RDSpinal, epidural and caudal anesthesia. Miller's Anesthesia. 2010, 7th ed. : Philadelphia, Churchill livingstone. pp 1625-1626.

6. Dorfman LJ, Bosley TM. Age-related changes in peripheral and central nerve conduction in man. Neurology 1979; 29: 38-44. PMID: 570675.

7. Keorochana G, Taghavi CE, Tzeng ST, Morishita Y, Yoo JH, Lee KB, et al. Magnetic resonance imaging grading of interspinous ligament degeneration of the lumbar spine and its relation to aging, spinal degeneration, and segmental motion. J Neurosurg Spine 2010; 13: 494-499. PMID: 20887147.

8. Greene NM. Distribution of local anesthetic solutions within the subarachnoid space. Anesth Analg 1985; 64: 715-730. PMID: 3893222.

9. Racle JP, Benkhadra A, Poy JY, Gleizai B. Spinal analgesia with hyperbaric bupivacaine: influence of age. Br J Anaesth 1988; 60: 508-514. PMID: 3377926.


10. Veering BT, Immink-Speet TT, Burm AG, Stienstra R, Van Kleef JW. Spinal anesthesia with 0.5% hyperbaric bupivacaine in elderly patients: effects of duration spent in the sitting position. Br J Anaesth 2001; 87: 738-742. PMID: 11878525.


11. Cameron AE, Arnold RW, Ghorisa MW, Jamieson V. Spinal analgesia using bupivacaine 0.5% plain. Variation in the extent of the block with patient age. Anaesthesia 1981; 36: 318-322. PMID: 7224128.

12. Lee GY, Han JI, Lee CH. Spinal anesthesia with 0.5% hyperbaric bupivacaine in elderly patients: influence of aging in spread of analgesia and blood pressure. Korean J Anesthesiol 1999; 37: 436-441.

13. Sise LF. Spinal anesthesia for upper and lower abdominal operations. N Engl J Med 1928; 199: 59-66.

14. Kawamoto M, Tanaka N, Takasaki M. Power spectral analysis of heart rate variability after spinal anaesthesia. Br J Anaesth 1993; 71: 523-527. PMID: 8260301.


15. Hemmingsen C, Poulsen JA, Risbo A. Prophylactic ephedrine during spinal anaesthesia: double-blind study in patients in ASA groups I-III. Br J Anaesth 1989; 63: 340-342. PMID: 2803892.


16. Critchley LA, Stuart JC, Short TG, Gin T. Haemodynamic effects of subarachnoid block in elderly patients. Br J Anaesth 1994; 73: 464-470. PMID: 7755705.


Fig.┬Ā1
The mean arterial pressure (MAP) from time of induction of spinal anesthesia. Value are the mean ┬▒ SD. *P < 0.05 compared with the baseline in te L group. Group L: lateral position during spinal anesthesia, Group S: sitting position during spinal anesthesia.
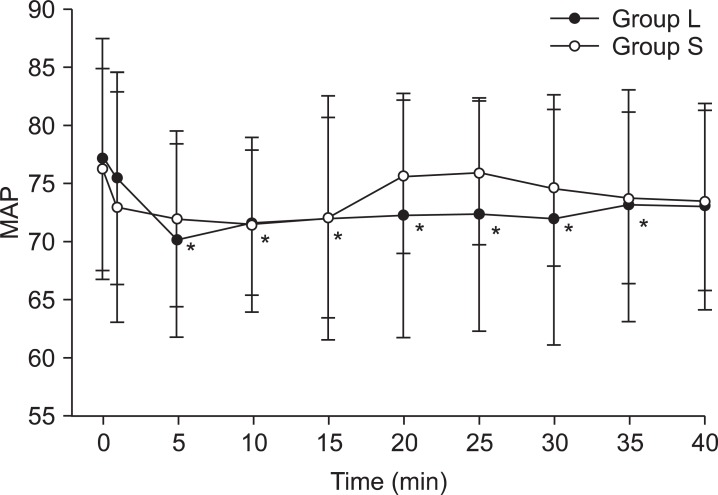
Fig.┬Ā2
The heart rate (HR) from time of induction of spinal anesthesia. Value are the mean ┬▒ SD. *P < 0.05 compared with the baseline in the L group, ŌĆĀP < 0.05 compared with baseline in S group. Group L: lateral position during spinal anesthesia, Group S: sitting position during spinal anesthesia.
- TOOLS
-
METRICS

-
- 3 Crossref
- Scopus
- 2,949 View
- 38 Download