|
 |
|
|
Abstract
Ingestion of disk batteries may have serious complications such as esophageal burn, perforation, and tracheoesophageal fistula, particularly when the battery is caught in the esophagus. Proper placement of the tracheal tube is critical when tracheoesophageal fistula was occurred from esophageal impaction the battery. Endoscopy of upper gastrointestinal tract in infants and children is an important and effective tool for the diagnosis and treatment of foreign body ingestion. But upper gastrointestinal endoscopy in infant and children has very high risk of tracheal compression and airway compromise. We present a case of ventilatory compromise during insertion of the upper gastrointestinal endoscopy in 16-month-old child with tracheoesophageal fistula secondary to disk battery ingestion.
Ingestion of foreign substances frequently occurs in infants older than 6 months, and although the intake of batteries is less than 2% of the foreign substances ingested, it is gradually increasing [1]. 80-90% of foreign substances pass through the alimentary canal without any problems, but 10-20% need to be removed via an endoscope [2]. When a substance is caught in the esophagus, it can cause serious complications; therefore, it must be endoscopically removed immediately. Symptoms such as dysdipsia, nausea, vomiting, and abdominal pain usually appear after ingesting batteries, but there have been cases with rash, coughing, wheezing, and dyspnea due to the patient absorbing the chemical components of the battery, which can delay a proper diagnosis by being misdiagnosed as another illness [3]. The main complication of battery ingestion is tracheoesophageal fistula (TEF), which is usually found by radiological postoperative evaluation. It is generally not assessed at the time of anesthesia due to urgency of the operation so it is necessary to be cautious when administrating anesthesia.
During the removal of a battery caught in the esophagus of an infant using an endoscope under general anesthesia, the authors of this paper experienced ventilatory compromise from TEF and physical pressure from the endoscope and thereby are reporting this case with a subsequent review of the literature.
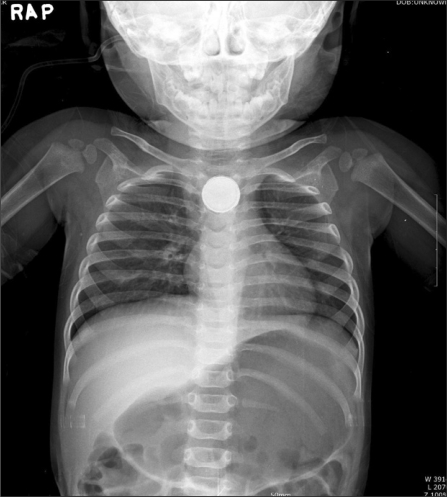
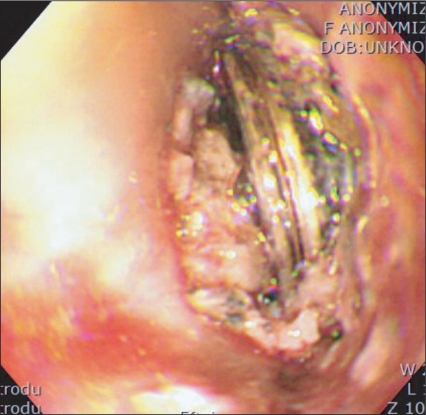
A 16-month old, baby girl, weighing 9.5 kg and measuring 74 cm, visited the hospital because of a cough. In a chest radiograph done under the suspicion of an upper respiratory infection, a round foreign object with a diameter of 21 mm was detected in the upper esophagus (Fig. 1). In a sleep endoscopy, it was confirmed to be a circular battery (Fig. 2), and ingestion was estimated to occur three days prior to the hospital visit, and it was determined that endoscopic removal would not be easy. Therefore, it was decided to immediately remove the battery under general anesthesia.
The infant had no underlying disease, and glycopyrrolate 0.05 mg was IM injected 30 minutes before arriving at the operating room as premedication for the anesthesia. The infant was monitored by ECG, non-invasive blood pressure (NIBP), and a pulse oximetry, and before anesthesia, her blood pressure was 85/61 mmHg; her heart rate was 160 beats/min with 100% oxygen saturation. 10 mg of Ketamine was IV injected and after loss of consciousness, 5 mg of Rocunium was IV injected. When the muscles were sufficiently relaxed, an uncuffed endotracheal tube with a 4 mm inside diameter was intubated. After intubation, both lungs were checked through a stethoscope and found to be normal, and the endotracheal tube was set to 11 cm in accordance with the top front teeth. Anesthesia was maintained by 2 L/min of air, 2 L/min of O2, and 2.0-3.5 vol% of sevoflurane. The tidal volume was 90 ml; respiratory rate was 18/min through volume-controlled mechanical ventilation to maintain an end-tidal CO2 (EtCO2) pressure of 35-40 mmHg and the peak inspiratory pressure (PIP) at this point was 19 cmH2O.
An adult endoscope with a 9 mm outer diameter was used for the removal procedure because the hospital did not have a pediatric endoscope with forceps. 2 minutes after inserting the endoscope, severe abdominal inflation was observed, and PIP increased up to 28-30 cmH2O with the tidal volume decreasing to less than 50 ml. The battery had caused an inflammatory change and conglutinated onto surrounding tissue in the esophagus, and 3 minutes after inserting the endoscope, oxygen saturation decreased to 80%, and EtCO2 pressure rose to 70 mmHg therefore the surgery was stopped and the endoscope was removed. By manual ventilation using 100% oxygen, oxygen saturation was recovered to 100% and EtCO2 pressure to 40 mmHg, and thereafter, the endoscope was reinserted.
In the second attempt of the procedure, manual ventilation was done instead of mechanical ventilation. However, 1 minute after the insertion of the endoscope, a sudden strong resistance was felt in the reservoir bag, and the tidal volume was less than 20 ml despite applying more than 35 cmH2O for the PIP. Oxygen saturation dropped below 60% so the procedure could not be continued; therefore, the endoscope was removed again. Here, a PIP of 25-30 cmH2O and a tidal volume of 50 ml were maintained. The endoscope was reinserted after recovering oxygen saturation to 100%, but due to the increased airway pressure, ventilation was not possible, and oxygen saturation dropped back down to less than 40%. The authors suspected the possibility of TEF considering the period of intake and the excessive air volume seen in the stomach in the chest radiograph taken before the surgery. Hence, the endotracheal tube was inserted until one lung ventilation was possible and then retreated while auscultating to secure onto the location where the pulmonary sound from both lungs became equal. The adjusted position of the endotracheal tube was 15 cm based on the top front teeth. A PIP of 25-30 cmH2O and a tidal volume of 80-100 ml were maintained. In the next insertion of the endoscope, A PIP of 30 cmH2O and a tidal volume of 50 ml were maintained but abdominal inflation was excessive so air in the stomach was partially removed with the endoscope, and the operating doctor was required to use the minimal amount of air for the surgery to proceed. A PIP of 25-30 cmH2O, a tidal volume of 50-80 ml, and oxygen saturation of 100% were maintained during the procedure, and the battery was removed.
After the removal of the battery, the vital signs were blood pressure 96/69 mmHg, heart rate 152 beats/min, and 100% oxygen saturation. The patient was not extubated but moved to postoperative intensive care, and after pediatrics observed vital signs for about 3 hours to verify that there were no abnormalities, extubation was done. Subsequent vital sign checks and physical exam were normal, and there were no abnormalities found in the blood test. Moreover, the right main bronchus appeared on the screen in the postoperative esophagography (Fig. 3), and the chest CT scan found TEF at 1.4 cm in the upper carina (Fig. 4). The guardian wanted to have surgery for TEF at another hospital; therefore, 3 days after the surgery, she was transferred.
The infant in this case only presented with intermittent coughing after ingesting a battery. It was found and removed 3 days after ingestion. Ingested batteries usually pass through the gastrointestinal tract and are defecated in a few days, but when it is caught in the esophagus, the moist environment of the esophagus allows for the discharge of substances inside the battery together with electrical discharges, which can cause tissue damage of the esophagus. In addition, necrosis can develop in the mucus membrane of the esophagus due to the pressure from the battery, and these can trigger complications such as esophageal burns, perforation, and TEF [4]. More severe complications arose in cases where the diameter of the battery was larger than 20 mm and the infant was younger than 4 years old [5]. The main factors that cause severe complications in battery ingestion were the size (larger than 20-30 mm) and components of the battery. Especially if the negative terminal of the battery is attached to the tissue, it can lead to more severe results [6]. In addition, lithium batteries cause the most severe damages, and it was reported that in a dog's esophagus, necrosis developed in the trachea within an hour [7]. In this case study, the corroded battery and inflamed mucous membrane of the esophagus were confirmed in endoscopy before the surgery, but TEF could not be tested and confirmed due to the urgency of the surgery. It is reported that esophageal burns start 4 hours after battery ingestion and perforations that form fistulas start in 6 hours [3]. Since the estimated ingestion period for this case was 3 days, it is enough time for TEF to develop.
The infant in this case study did not have respiratory difficulties before of the surgery, but ventilation failure during the surgery was because the endotracheal tube was fixed at 11cm at first. The TEF located approximately 2.6 cm under the end of the endotracheal tube allowed the inhalation gas for the anesthesia to flow into the stomach leading to abdominal inflation, and consecutively, the air injected for the endoscopic surgery flowed over to the respiratory tract to greatly increase the airway pressure. Afterwards, when the endotracheal tube was inserted deeply into the carina, the tube was located past the TEF so the influence of TEF was eliminated for the decrease in airway pressure. When there is TEF, it is important to position the endotracheal tube above the carina and below the TEF to maintain anesthesia [8]. This is because effective ventilation would not happen due to a loss of the tidal volume through the fistulous openings in the TEF, the contents of the stomach being aspirated into the lungs, and excessive positive pressure ventilation when inducing anesthesia can cause abdominal inflation and cardiovascular suppression [9].
However, in our case, ventilation was not completely recovered even when the endotracheal tube was inserted deeply to eliminate the influence of TEF, and this is thought to be from accompanying ventilation failure from the endoscope. This ventilation failure can be caused by pressure on the pharynx and the trachea from the weight of the endoscope [10], or motor abnormality of the diaphragm due to abdominal inflation from the injected air [11]. Wengrower et al. [12] reported that approximately 7% of infants who had endoscopic procedures under sedation or anesthesia exhibited temporary desaturation. There are reports that an infant with a similar height and weight developed ventilation failure from a TEE probe with outer diameter of 10 ├Ś 8 mm [13]. In our case, the fact that direct pressure on the respiratory tract was applied by using an adult endoscope with a 9 mm diameter and that air had to be injected continually since the battery had attached itself to the esophagus and was hard to remove could have been some other causes for the excessive airway pressure, ventilation failure, and hypoxemia. When upper gastrointestinal endoscopic procedures were done on 99 infants of 0.9-10.1 kg using an endoscope with a 5.2 mm outer diameter, only 1 infant with global developmental delay exhibited hypoxemia [14], and Gryboski recommended using endoscopes with a 5 mm outer diameter on infants with esophageal diseases [15]. It is important to use pediatric endoscopes with the smallest possible outer diameters to prevent hypoxemia during endoscopic procedures on infants.
Since the removal of foreign objects in the esophagus of infants are usually done under general anesthesia, anesthesiologists need to anticipate ventilation failure and hypoxemia from the physical pressure from the procedural equipment and the excessive injection of air and proceed with anesthesia under close cooperation with the operating surgeon. Especially when a battery has been ingested, it is necessary to be aware that there could be complications such as TEF in the location where the battery is depending on the battery's components, size, and ingestion period. Ingestion of a battery can cause serious ventilation failure and hypoxemia. In addition, to more effectively block the mutual flow of air and anesthetic gas towards either the esophagus or the trachea in the case of a potential TEF, a cuffed endotracheal tube should be chosen preferentially and special caution should be taken to fix the position of the tube and in selecting a suitable size for the endoscope used in the procedure.
References
1. Yardeni D, Yardeni H, Coran AG, Golladay ES. Severe esophageal damage due to button battery ingestion: can it be prevented? Pediatr Surg Int 2004; 20: 496-501. PMID: 15221361.

2. Faigel DO, Stotland BR, Kochman ML, Hoops T, Judge T, Kroser J, et al. Device choice and experience level in endoscopic foreign object retrieval: an in vivo study. Gastrointest Endosc 1997; 45: 490-492. PMID: 9199906.

3. Litovitz T, Schmitz BF. Ingestion of cylindrical and button batteries: an analysis of 2382 cases. Pediatrics 1992; 89: 747-757. PMID: 1557273.
4. Samad L, Ali M, Ramzi H. Button battery ingestion: hazards of esophageal impaction. J Pediatr Surg 1999; 34: 1527-1531. PMID: 10549763.

5. Litovitz T, Whitaker N, Clark L, White NC, Marsolek M. Emerging battery-ingestion hazard: clinical implications. Pediatrics 2010; 125: 1168-1177. PMID: 20498173.

6. Yoshikawa T, Asai S, Takekawa Y, Kida A, Ishikawa K. Experimental investigation of battery-induced esophageal burn injury in rabbits. Crit Care Med 1997; 25: 2039-2044. PMID: 9403755.

7. Tanaka J, Yamashita M, Yamashita M, Kajigaya H. Esophageal electrochemical burns due to button type lithium batteries in dogs. Vet Hum Toxicol 1998; 40: 193-196. PMID: 9682401.
8. Bernard JD. Edited by Miller RDPediatric anesthesia. Miller's anesthesia. 2010, 7th ed. : Philadelphia, Churchill-Rivingstone. p 2590.
9. Son YS, Chung KD, Cho HS, Lee SM, Park K, Lee JH, et al. Anesthetic experience of acquired distal tracheoesophageal fistula: a case report. Korean J Anesthesiol 2006; 50: 346-350.

10. Rimmer KP, Graham K, Whitelaw WA, Field SK. Mechanisms of hypoxemia during panendoscopy. J Clin Gastroenterol 1989; 11: 17-22. PMID: 2921488.

11. Lamireau T, Dubreuil M, Daconceicao M. Oxygen saturation during esophagogastroduodenoscopy in children: general anesthesia versus intravenous sedation. J Pediatr Gastroenterol Nutr 1998; 27: 172-175. PMID: 9702648.

12. Wengrower D, Gozal D, Gozal Y, Meiri Ch, Golan I, Granot E, et al. Complicated endoscopic pediatric procedures using deep sedation and general anesthesia are safe in the endoscopy suite. Scand J Gastroenterol 2004; 39: 283-286. PMID: 15074400.

13. Park SY, Park SK, Hong YS, Hong YW. Compromised ventilation caused by transesophageal echocardiography probe in pediatric patients undergoing congenital heart surgery - a case report -. Korean J Anesthesiol 2008; 54: 682-684.

14. Ruuska T, Fell JM, Bisset WM, Milla PJ. Neonatal and infantile upper gastrointestinal endoscopy using a new small diameter fibreoptic gastroscope. J Pediatr Gastroenterol Nutr 1996; 23: 604-608. PMID: 8985853.

15. Gryboski JD. The value of upper gastrointestinal endoscopy in children. Dig Dis Sci 1981; 26: 17S-21S. PMID: 6765050.

- TOOLS
-
METRICS

-
- 2 Crossref
- Scopus
- 3,548 View
- 39 Download