|
 |
|
|
Abstract
Background
The Glidescope® videolaryngoscope is a new device for tracheal intubation that provides an improved view of the larynx. This study was performed to compare the Glidescope with the McGrath videolaryngoscope in terms of time to intubation (TTI) and number of attempts.
Methods
Patients were randomly allocated to one of two groups, Glidescope or McGrath group, by using computer-generated numbers. Tracheal intubation was attempted by an anesthesiologist with extensive experience using these two devices. The operator recorded ease of visualization of glottic structures based on the classification described by Cormack and Lehane. Number of failures, number of attempts and their duration, total intubation time, and events during the whole procedure were recorded. The duration of one attempt was defined as the time elapsed between picking up the endotracheal tube and verification of tracheal intubation with visualization of three expiratory carbon dioxide waveforms. TTI was defined as the sum of the duration of all intubation attempts (as many as three), excluding preoxygenation procedures.
Results
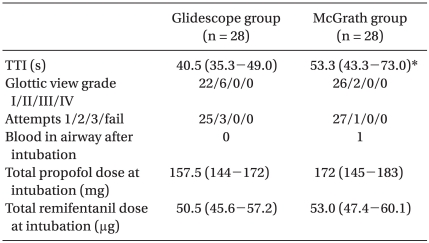
TTI was significantly shorter for the Glidescope® compared to the McGrath® laryngoscope (40.5 vs. 53.3 s, respectively, P < 0.05). However, glottic views obtained at intubation were similar between the two groups. Number of intubation attempts was not significantly different between the two groups (1.03 ± 0.19 vs 1.10 ± 0.32, respectively) (mean ± SD).
The Glidescope® videolaryngoscope (GVL; Verathon Inc., Bothell, USA) is a new device for tracheal intubation that provides an improved view of the larynx [1]. GVL consistently yields a comparable or superior glottic view compared with direct laryngoscopy despite limited or lack of prior experience with the device [2].
The McGrath® Series 5 is a self-contained videolaryngoscope (Aircraft Medical, Edinburgh, UK), which has been used successfully in the management of both normal and difficult airways [3-6].
The aim of this study was primarily to compare the Glidescope with the McGrath with regard to time to intubation (TTI) and number of attempts, and secondarily to determine whether the Glidescope could attenuate the hemodynamic response to orotracheal intubation compared with the McGrath.
After local ethics committee approval and informed consent had been obtained, American Society of Anesthesiologists Physical Status I or II patients, aged 18-65 yr and undergoing minor elective surgery were considered for the study. During preoperative visits, the anesthesiologist noted age, sex, weight, height, Mallampati class, mouth opening, and thyromental distance. Exclusion criteria included patients with cardiovascular, respiratory, hepatic, renal or neuromuscular diseases; uncooperative patients; those with a history of gastroesophageal reflux or an increased risk of aspiration; and patients with coagulation disorders. Patients with a history of previous difficult intubation or suspected difficult intubation were also excluded. This was defined as the presence of a Mallampati class IV, retrognathia, restricted neck movements, or more than two of the following criteria: Mallampati class III, mouth opening less than 35 mm, or a thyromental distance of less than 65 mm. All of these parameters were measured by an experienced anesthesiologist.
Patients were randomly allocated to one of two groups, the Glidescope or McGrath group, using computer-generated numbers. Anesthetic management and intraoperative care were standardized. When patients arrived at the operating room, they were placed in the "sniffing position" with their head on a pillow and routinely monitored including the attachment of a Bispectral Index (BIS) (Aspect Medical Systems, USA) sensor. Baseline values of systolic arterial pressure (SAP), mean arterial blood pressure (MAP), heart rate, oxyhemoglobin saturation, and BIS were measured. Anesthesia was induced with a target-controlled infusion (TCI) of remifentanil set at an initial effect site concentration of 2-3 ng/ml. The infusion device was Orchestra┬« Base Primea (Fresenius Kabi, France) whose PK was the Minto model [7], which adjusts for age, weight, and sex. The device has an equilibration constant (Keo) of 0.595-0.007x (age-40)/min and a simultaneous infusion of TCI 2% propofol using the PK parameter set of Schnider et al. [8] set at an initial effect site concentration of 4-6 ┬Ąg/ml. In order to maintain oxygenation, the patient's lungs were ventilated with 100% oxygen using a standard facemask. Once full neuromuscular blockade was achieved one minute after a 0.9 mg/kg dose of rocuronium (judged by lack of response to peripheral nerve stimulation) and the BIS value was < 60, tracheal intubation was attempted by one of three anesthesiologists with extensive experience using the Glidescope and McGrath. The operator recorded ease of visualization of glottic structures based on the classification described by Cormack and Lehane [9]. Endotracheal tubes (ETT) with a 7.5 mm and 7.0 mm internal diameter for male and female, respectively, were used. ETT was prepared with a stylet, because a styletted ETT is highly desirable to intubate the trachea when Glidescope and McGrath are used [10]. Any attempt that lasted more than 120 s or was associated with peripheral oxygen saturation less than 92% was stopped. More than four attempts or 120 s were regarded as failure of intubations. Number of failures, number of attempts and their duration, total intubation time, and events during the whole procedure were recorded. The duration of one attempt was defined as the time elapsed between picking up the ETT and verification of tracheal intubation with visualization of three expiratory carbon dioxide waveforms during mechanical ventilation, with a tidal volume of 10 ml/kg at a respiratory rate of 20 breaths/min.
TTI was defined as the sum of the duration of all intubation attempts (as many as three), excluding the preoxygenation procedures. Failure to intubate was defined as the inability to place the endotracheal tube into the trachea after three attempts. If failure to secure the airway occurred, then conventional difficult intubation protocols were prepared.
SAP, MAP, and heart rate were measured and recorded in the operating room three times: at baseline, at intubation and 3 min after intubation.
For sample size calculation, a pilot study was conducted in 10 patients from the McGrath group. The mean value of total intubation time was 49 ┬▒ 15.0 s. For power calculation, equal standard deviation for both groups was assumed. To show a difference of 12 seconds between the two groups and with ╬▒ = 0.05, two tailed and a power of 80%, 26 patients per group were needed.
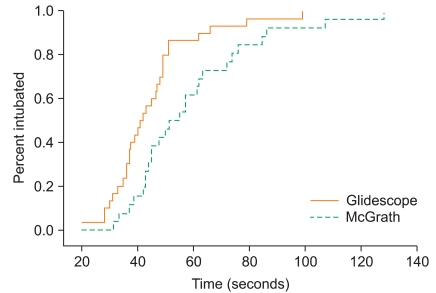
Data were expressed as median and interquartile range or as categorical distributions. Statistical analyses were performed using the Statistical Package for Social Sciences software (SPSS 12.0 for Windows; SPSS Inc., IL, USA) and SigmaStat (SIGMASTAT 3.1; Systat Software, Inc., CA, USA). Between-group comparisons for numerical data were analyzed with the Mann-Whitney Rank Sum Test. Kaplan-Meier plots were constructed to graphically represent the temporal component of intubation. Nonparametric data were analyzed using the Žć2 and Fisher's exact test (when appropriate), and hemodynamic data were analyzed using the Kruskal-Wallis One Way Analysis of variance, with a Dunn multiple comparison test for intergroup comparison. A P < 0.05 was regarded as statistically significant.
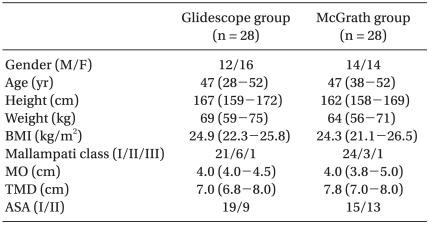
Fifty-six patients were enrolled in this study. Patient demographic data were statistically similar between the two groups in terms of age, weight, height, BMI and ASA (Table 1).
TTI was significantly shorter for the Glidescope® compared to the McGrath® laryngoscope (P < 0.05) (Table 2). To compare the temporal component of the success of intubation, Kaplan-Meier plots were constructed (Fig. 1). Glottic views obtained at intubation were similar between the two groups (Table 2). The number of intubation attempts was not significantly different between the two groups (Table 2).
There were no significant differences of total doses of propofol and remifentanil at intubation (Table 2).
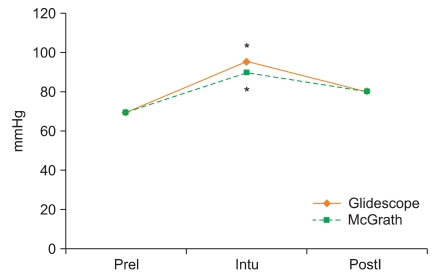
Baseline hemodynamics did not differ between the two groups. There were significant differences in SAP and HR of both groups after intubation when compared to baseline values (P < 0.05) (Fig. 2 and 3). However, there was no significant difference between the groups. After tracheal intubation, SAP and HR returned to baseline within 3 min in both groups (Fig. 2 and 3).
This study, which compares the Glidescope with the McGrath in terms of TTI and number of attempts, demonstrates that the Glidescope reduces total intubation time in comparison with the McGrath, judged by TTI (40.5 vs 53.3 s, respectively).
The Kaplan-Meier plot showing the percentage of patients intubated as time progressed demonstrates the superiority of the Glidescope at all time points. At 40 seconds, only 16% of patients were intubated in the McGrath group, while 50% of patients were already intubated in the Glidescope group.
Van Zundert et al. [10] reported that using a styletted ETT with the Glidescope and the McGrath increased first pass success rates in healthy adult patients (from 53 to 76 and from 52 to 74, respectively). Sun et al. [11] found a first pass success rate of 94% when using the Glidescope with a styletted ETT. Similarly, Shippey et al. [3] reported a first pass success rate of 93% when using the McGrath with a styletted ETT. They believed that mounting the tube onto a stylet and angling the distal tip upwards by 60-70┬░ at the proximal end of the cuff allowed easier insertion of the tube into the larynx, and using a stylet and correctly shaping the tracheal tube was mandatory to assist tracheal intubation with the McGrath. Maassen et al. [12] confirmed that a styletted ETT was highly desirable to intubate the trachea in morbidly obese patients when the Glidescope and McGrath were used. In this study, we used the styletted ETT and found the first pass success rate of the Glidescope and McGrath was 25/28 (89%) and 27/28 (96%), respectively.
Median time to intubation using the Glidescope and the McGrath was 40.5 s and 53.3, respectively, which is comparable to times achieved with other studies [1,10,13]. Rai et al. [1] concluded that the Glidescope provided an improved view of the larynx and allowed for successful tracheal intubation. Malik et al. [14] compared the Glidescope with a standard Macintosh laryngoscope in patients with cervical spine immobilization. They found that the Glidescope groups had significantly lower Cormack and Lehane scores compared with the Macintosh. Shippey et al. [5] reported that the Cormack and Lehane grade view I was 88.9% and grade II was 11.1%. Tracheal intubation was successful in all patients. In our study, the Cormack and Lehane grade I was 22/28 (78.6%) and grade II was 6/28 (21.4%) in the Glidescope group, while the Cormack and Lehane grade I was 26/28 (96.3%) and grade II was 2/28 (3.7%) in the McGrath group.
Xue et al. [15] demonstrated that hemodynamic responses to orotracheal intubation using a Glidescope and a Macintosh direct laryngoscope were similar, and the Glidescope had no special advantages over the Macintosh direct laryngoscope in attenuating these responses. Malik et al. [14] also reported that the Glidescope failed in attenuating hemodynamic responses to orotracheal intubation. In our study, there were significant increases in SAP and HR in both the Glidescope and McGrath groups. However, after tracheal intubation, SAP and HR returned to baseline within 3 min in both groups. These finding may be the result of intense tracheal stimulus caused by orotracheal intubation with both devices.
This study had several limitations. There may have been bias, as it was impossible to blind the anesthesiologist to the device being used. Second, all intubations were performed by experienced anesthesiologists; therefore, results may differ in the hands of less experienced users. Finally, our study population consisted of elective surgical patients with normal airways; thus, no conclusion can be made for patients in whom difficult intubation is expected.
In conclusion, the results of this study demonstrated that the Glidescope reduced total intubation time in comparison with the McGrath, in terms of TTI in patients with normal airways. Hemodynamic responses to intubation using the Glidescope and the McGrath were similar; therefore, the Glidescope had no special advantages over the McGrath in attenuating these responses.
References
1. Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance. Anaesthesia 2005; 60: 60-64. PMID: 15601274.


2. Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (Glidescope) in 728 patients. Can J Anaesth 2005; 52: 191-198. PMID: 15684262.


3. Shippey B, Ray D, McKeown D. Use of the McGrath videolaryngoscope in the management of difficult and failed tracheal intubation. Br J Anaesth 2008; 100: 116-119. PMID: 17959584.



4. Noppens RR, M├Čbus S, Heid F, Schmidtmann I, Werner C, Piepho T. Evaluation of the McGrath Series 5 videolaryngoscope after failed direct laryngoscopy. Anaesthesia 2010; 65: 716-720. PMID: 20528841.


5. Shippey B, Ray D, McKeown D. Case series: The McGrath videolaryngoscope-an initial clinical evaluation. Can J Anaesth 2007; 54: 307-313. PMID: 17400984.


6. Osborn IP, Behringer EC, Kramer DC. Difficult airway management following supratentorial craniotomy: a useful maneuver with a new device. Anesth Analg 2007; 105: 552-553. PMID: 17646543.


7. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology 1997; 86: 10-23. PMID: 9009935.


8. Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology 1998; 88: 1170-1182. PMID: 9605675.


9. Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105-1111. PMID: 6507827.


10. van Zundert A, Maassen R, Lee R, Willems R, Timmerman M, Siemonsma M, et al. A Macintosh laryngoscope blade for videolaryngoscopy reduces stylet use in patients with normal airways. Anesth Analg 2009; 109: 825-831. PMID: 19690253.


11. Sun DA, Warriner CB, Parsons DG, Klein R, Umedaly HS, Moult M. The Glidescope Video Laryngoscope: randomized clinical trial in 200 patients. Br J Anaesth 2005; 94: 381-384. PMID: 15567809.



12. Maassen R, Lee R, Hermans B, Marcus M, van Zundert A. A comparison of three videolaryngoscopes: the Macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesth Analg 2009; 109: 1560-1565. PMID: 19713258.


13. Walker L, Brampton W, Halai M, Hoy C, Lee E, Scott I, et al. Randomized controlled trial of intubation with the McGrath Series 5 videolaryngoscope by inexperienced anaesthetists. Br J Anaesth 2009; 103: 440-445. PMID: 19605408.



14. Malik MA, Maharaj CH, Harte BH, Laffey JG. Comparison of Macintosh, Truview EVO2, Glidescope, and Airwayscope laryngoscope use in patients with cervical spine immobilization. Br J Anaesth 2008; 101: 723-730. PMID: 18784069.



15. Xue FS, Zhang GH, Li XY, Sun HT, Li P, Li CW, et al. Comparison of hemodynamic responses to orotracheal intubation with the GlideScope videolaryngoscope and the Macintosh direct laryngoscope. J Clin Anesth 2007; 19: 245-250. PMID: 17572317.


Fig.┬Ā2
Graph demonstrating changes in systolic arterial pressure with Glidescope and McGrath. PreI: baseline values, Intu: values immediately after intubation, PostI: values at 3 min after intubation. *P < 0.05 compared with baseline values.

Fig.┬Ā3
Graph demonstrating changes in heart rate with Glidescope and McGrath. PreI: baseline values, Intu: values immediately after intubation, PostI: values at 3 min after intubation. *P < 0.05 compared with baseline values.
- TOOLS