 |
 |
|
|
Abstract
We report a rare case of pseudoaneurysm of the inferior epigastric artery and inguinal hematoma extending to the scrotum following the removal of a femoral venous catheter in a 24-year-old male patient undergoing two consecutive neurosurgical procedures.
Femoral venous (FV) access can substitute subclavian vein (SCV) or internal jugular venous (IJV) access, especially for neurosurgical procedures, even though catheterization from the FV approach has a higher chance of mechanical complication such as injuring arteries and hematoma formation than the IJV or SCV approach [1,2]. Compared to the incidence of vascular injury (0.3-1%)[3], inferior epigastric artery (IEA) injury associated with femoral catheterization has been rarely reported. In general, iatrogenic IEA injuries presented serious retroperitoneal or scrotal hematoma, and often fatal complications such as hypovolemic shock [4] during surgical procedures in the abdominal wall [5]. We present a case of pseudoaneurysm of the IEA and massive inguinal and scrotal hematoma following the removal of a femoral venous catheter during two consecutive neurosurgical operations.
A 24-year-old man with a history of craniectomy due to an intracranial hemorrhage was admitted for cranioplasty. General anesthesia was administered and femoral venous catheterization using the Seldinger method was performed. The anesthesiologist staff checked the inguinal ligament and palpated the femoral artery at about 2 cm inferior to the inguinal ligament. The operator punctured the medial skin to the palpated femoral artery. At a depth of 2 cm from the skin, the femoral vein was punctured and venous catheterization was successfully done with a 7 Fr. two-lumen catheter (ARROWgard Blue®, Arrow International, Reading, PA, USA) on the first attempt. The first surgery, lasting 5 hours and 25 minutes, was uneventful and there were no signs of swelling or petechia around the catheter insertion site postoperation. However, a routine postoperative brain CT revealed an epidural hematoma and emergent removal of the hematoma was accomplished. The total anesthesia time of the second surgery was 3 hours and 15 minutes. During both operations, hemodynamic variables were well maintained, and fluids including 4 units of packed red blood cells were administrated via a femoral venous catheter.
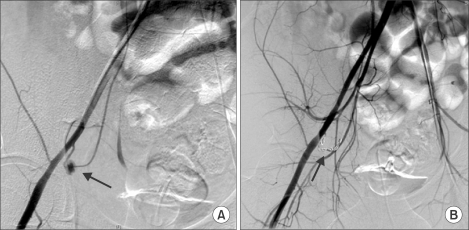
On postoperative (post-op) day 1, the femoral catheter was removed and physical compression and compressive dressing on the puncture site were performed. Two hours after removal of the catheter, the patient complained of severe scrotal pain and swelling. Urologic ultrasound and CT (Fig. 1) scans in the inguinal area and scrotum showed a large hematoma in the right inguinal area, which extended into the scrotum (2 × 3 cm within scrotum) via a spermatic cord from the inguinal canal, as well as extravasating contrast within the hematoma suspected of originating from the right common femoral artery. An emergent right common iliac artery angiography showed a 0.3 cm-sized pseudoaneurysm located at the distal 2 cm of the inferior epigastric artery orifice arising from the right external iliac artery (Fig. 2). Embolization with 9 pieces of Tornado microcoils (Cook, Bloomington, USA) was performed at the bilateral necks of the pseudoaneurysm. For care of the scrotal hematoma, surgical exploration was not attempted and instead conservative treatments of bed rest and scrotal elevation were provided. On post-op day 4, a urologic ultrasound scan showed a large hematoma still persisting in the scrotum and pushing the right testis laterally; however, no abnormalities of the scrotum and epididymis were observed.
On post-op day 14, hypoechoic lesions with heterogenous echotexture in the right scrotum were noted on an ultrasound scan, which suggested the gradual resolving of the hematoma. The patient was free of pain, but petechia and mild swelling on the scrotum, penis, and inguinal area remained. During the following 3 weeks, the patient's condition continued to improve and he was subsequently discharged.
Femoral vein access is an effective alternative to both internal jugular and subclavian access, especially for neurosurgical procedures [6]. We report a case of pseudoaneurysm of the IEA and inguinal hematoma extending to the scrotum following the removal of a femoral venous catheter, which indwelled and functioned well during two consecutive neurosurgical procedures. Femoral venous catheterization was performed successfully on the first attempt, and a considerable volume of crystalloid and blood components was administered through it while the two operations were performed.
According to a review of IEA pseudoaneurysms by Georgiadis et al. [5], most occur during surgical procedures in the abdomen, such as retention sutures over inguinal ligament, laparoscopy, paracentesis, drainage insertion or needle biopsy. Injury to the IEA can be attributed to its anatomical travelling course. In general, the IEA arise from the external iliac artery immediately above the inguinal ligament. After leaving the external iliac artery, the IEA curves forward in the subperitoneal tissue, and then ascends obliquely along the medial margin of the abdominal inguinal ring and behind the entrance of the spermatic cord. There is, however, variability in its origin [7]. In our patient, the angiograph showed unusual downward travelling of the IEA about 2 cm from the orifice of the IEA and then an upward turn, where the pseudoaneurysm was identified (Fig. 2). Therefore, the inserted needle might penetrate the IEA directly overlying the femoral vein and then puncture the femoral vein through the IEA. An indwelling catheter in situ would prevent bleeding from IEA during the operation; however, immediately following removal of the catheter, conventional compression at the puncture site could no longer prevent the IEA from bleeding, leading to extravasation and formation of an IEA pseudoaneurysm. As the inferior epigastric artery passes obliquely upward from its origin it lies along the lower and medial margins of the abdominal inguinal ring, and behind the commencement of the spermatic cord. Scrotal hematoma may occur if bleeding occurs between anatomic fascial planes [8].
Clinical features of vascular injuries in association with femoral venous catheterization might differ according to the anatomic location of the injured vasculature. Catheterization above the inguinal ligament could injure the external iliac artery or IEA, which may present as a painless compressible abdominal mass, right tender painful periumbilical mass, retroperitoneal hemorrhage [8], or scrotal hematoma [5]. Our patient complained of scrotal swelling and pain immediately after the removal of the femoral venous catheter. In some cases of delayed presentation, IEA pseudoaneurysm may accompany an arteriovenous fistula [9]. Unlike direct injury-associated IEA pseudoaneurysm, which is related to higher puncture above the inguinal ligament, pseudoaneurysm of the femoral artery is relatively common in lower puncture sites at lower levels of the inguinal ligament because the femoral head cannot work as a posterior bony support for adequate arterial compression after catheter removal [10]. Symptoms and signs of femoral artery pseudoaneurysm has a tendency to localize at the arterial puncture site [11], and may include pain, swelling, severe bruising, palpable thrill or pulsatile mass in the inguinal area. Regardless of the pseudoaneurysm's location, a rapidly growing hematoma may lead to ischemia, venous thrombosis, neuropathy, or necrosis of overlying skin. Therefore, upon suspecting vascular injuries, prompt diagnostic procedures are required; for example, an ultrasound scan and abdominal CT improves diagnostic accuracy and an angiography confirms the diagnosis [6].
Treatment depends on the severity of complication. A small-sized pseudoaneurysm would resolve spontaneously in a few weeks. However, for a large or rapidly growing pseudoaneurysm, an ultrasound-guided local injection of thrombin or collagen into the pseudoaneurysm cavity or embolization could be applied. In severe cases, surgical exploration should be considered.
In conclusion, we report a rare IEA pseudoaneurysm and scrotal hematoma - most likely due to variability in vascular course - occurring after the removal of a well-functioning femoral venous catheter, which was subsequently managed with microcoil embolization without scrotal exploration.
References
1. Merrer J, De Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically ill patients: a randomized controlled trial. JAMA 2001; 286: 700-707. PMID: 11495620.


2. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med 2003; 348: 1123-1133. PMID: 12646670.


3. Ricci MA, Trevisani GT, Pilcher DB. Vascular complications of cardiac catheterization. Am J Surg 1994; 167: 375-378. PMID: 8179080.


4. Sreeram S, Lumsden AB, Miller JS, Salam AA, Dodson TF, Smith RB. Retroperitoneal hematoma following femoral arterial catheterization: a serious and often fatal complication. Am Surg 1993; 59: 94-98. PMID: 8476149.

5. Georgiadis GS, Souftas VD, Papas TT, Lazarides MK, Prassopoulos P. Inferior epigastric artery false aneurysms: review of the literature and case report. Eur J Vasc Endovasc Surg 2007; 33: 182-186. PMID: 17055755.


6. Ahmad F, Turner SA, Torrie P, Gibson M. Iatrogenic femoral artery pseudoaneurysms--a review of current methods of diagnosis and treatment. Clin Radiol 2008; 63: 1310-1316. PMID: 18996260.


7. Jakubowicz M, Czarniawska-Grzesiñska M. Variability in origin and topography of the inferior epigastric and obturator arteries. Folia Morphol (Warsz) 1996; 55: 121-126. PMID: 8908792.

8. Thomas AA, Hedgepeth R, Sarac TP, Vasavada SP. Massive scrotal hematoma following transfemoral cardiac catheterization. Can J Urol 2008; 15: 4020-4023. PMID: 18405454.

9. Piñero A, Reus M, Agea B, Capel A, Riquelme J, Parrilla P. Case report: conservative management of an arteriovenous fistula of the inferior epigastric artery. Br J Radiol 2003; 76: 135-136. PMID: 12642284.


10. Rapoport S, Sniderman KW, Morse SS, Proto MH, Ross GR. Pseudoaneurysm: a complication of faulty technique in femoral arterial puncture. Radiology 1985; 154: 529-530. PMID: 3966139.


Fig. 1
Ultrasound scan (A) shows a 2 × 3 cm-sized hematoma in scrotum (dotted arrow) replacing right testis (solid arrow) laterally. CT scans in the inguinal area (B, C) show a large hematoma, in which contrast media (dot arrow) is visible (B), and hematoma shifting the penis (C). Therefore, emergent angiography was performed.

Fig. 2
Right common iliac artery angiography shows a 0.3 cm-sized pseudoaneurysm (dark arrow) of the inferior epigastric artery arising at 2 cm distal to the right external iliac artery (A). Using a microcatheter and microguide-wire, the distal neck of the pseudoaneurysm was selected and a microcoil embolization was performed at both the distal and proximal necks of the pseudoaneurysm. Nine pieces of Tornado microcoil were used (B). The puncture site was sealed with angioseal.
- TOOLS








