Introduction
An accurate analysis of the anatomical structure of the airway is needed in anesthesiology as well in all areas of medical procedures having to do with respirators. The accurate location of the endotracheal tube (ETT) is an important factor for adequate airway patency and safe anesthetic management, especially in cases that require endotracheal intubation (ETI) for total inhalational anesthesia [
1,
2]. When ETI is attempted in patients who have experienced cardiac arrest for advanced cardiac life support (ACLS), inappropriate bronchial intubation occurs in 28% of the cases [
3]; therefore, a more accurate standard for airway management is necessary.
In ETI, the location of the intubated tube may differ depending on the patient's physical condition, the position and movement of the head and neck, airway-related disorders, and congenital abnormalities [
4]. Additionally, since the airway of children is different than that of adults, accurate airway evaluations are necessary for safer medical management [
5].
In the current medical field, research regarding the standard measurements for ETI is based on western adults [
6], and it is suggested to be 23 cm for men and 21 cm for women. However, owing to the physical difference between Westerners and Koreans, this standard can increase the risk of bronchial intubation in Koreans [
7].
Previous studies conducted to evaluate the lengths of the upper airway and the trachea in Korean adults used CTs and bronchoscopy, but did not clearly show the difference in length between Westerners and Koreans [
8-
11]. Additionally, there are physical differences between western and Korean children, whose physical measurements rapidly change depending on their age. Previous studies conducted to evaluate the length of the upper airway and trachea of Korean children were indirect and based simply on x-ray images and endotracheal tubes [
12,
13]. Indeed, no direct measurements have been conducted using fibroptic bronchoscopy.
Therefore, instead of measuring the lengths from chest x-ray images and CT scans, we conducted a more accurate and direct study of Korean children and adults electing ophthalmic and ENT surgery using fibroptic bronchoscopy to determine the lengths of the structural parts of the airway and to offer a more Korean-specific proper ETI depth.
Materials and Methods
This study was conducted on 87 American Society of Anesthesiologists class I patients ranging in age from 5-81 electing for noninvasive ENT or ophthalmic surgery. Written consent for the bronchoscopy-based airway study was gained in addition to consent for the anesthesia. For children, pyridostigmine (0.004 mg/kg) was IM administered as premedication, while 0.2 mg of pyridostigmine and 2 mg of midazolam were administered IM and 20 mg famotidine was administered IV for adults. For anesthesia, children were administered 1.5 mg/kg ketamine IV, while adults were administered 1.5 mg/kg propofol IV. Afterwards, general anesthesia was maintained using sevoflurane and vecuronium.
Fibroptic bronchoscopy was used to measure the length of the upper airway and the trachea. After maintaining total muscle relaxation and appropriate oxygen saturation, the patient's head was placed in a neutral position, and the fibroptic bronchoscope was inserted into the trachea. First, the bronchoscope was inserted in the middle of the upper incisors, and after confirming the location of the carina, the scope was further inserted into each right and left main bronchus. Measurements were taken when the end of the bronchoscope reached the first point at which the main bronchus subdivides into the lobar bronchus. Afterwards, as the bronchoscope was being removed from the trachea, the distance to the carina was measured. The cricothyroid membrane, which is the point at which the distance between the cartilages widens, was checked, and the measurement was taken at the inferior margin of the cricoid cartilage. The measurements of each structural portion of the upper airway were taken and defined as below.
ILt: the length between the upper incisor and the distal end of the left main bronchus
IRt: the length between the upper incisor and the distal end of the right main bronchus
IC: the length between the upper incisor and the carina
Icr: the length between the upper incisor and the inferior margin of the cricoid cartilage
T: the length of the trachea (T = IC - Icr)
IT: the length from the upper incisors to the midtrachea (IT = Icr + 0.5 × T)
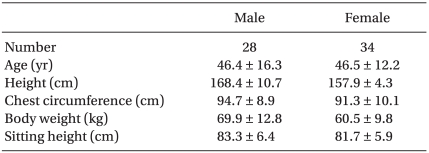
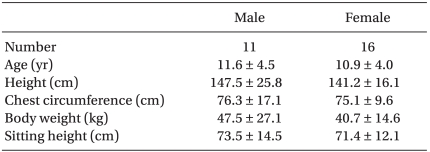
Afterwards, the age, sex, height, sitting height, chest width, and weight of all of the patients were recorded. Characteristic comparisons between the sexes of adults and children were conducted using a two tailed unpaired t-test. The relationship between the height, sitting height, and chest width to the lengths of the parts of the airway was tested using a simple linear regression analysis. The relationship between the lengths of the parts of the airway and the age of the child were also tested based on simple linear regression analysis. The correlation among each measurement was tested using a simple correlation analysis. The statistical analysis of each measurement was conducted using SPSS (ver. 17.0, SPSS Inc. USA). A P value below 0.05 was assumed to be statistically significant.
Discussion
Generally, the depth of ETI for Western adults is measured from the upper incisor or the mouth. For men, it is secured at a depth of 23 cm, while for women it is obtained at 21 cm [
6]. Latto et al. [
15] stated that the ideal position of the intubated tube is having the cuff's proximal end 1 cm below the vocal cord. Unfortunately, this is clinically difficult; thus, Eagle [
16] used body height to calculate this and suggested the appropriate method of defining the appropriate length of the intubated tube was when the end of the tube reached the midtrachea. These conclusions were obtained from elaborating on the method based on children that Morgan offered, which is Length of tube (cm) = 0.1 × height (cm) + 5 [
14,
16]. Research regarding the lengths of the upper airway and trachea in Korean adults using fibroptic bronchoscopy exists, but such studies are limited in the fact that the approach using the mean value, which is generally used, does not provide a correlation with a high coefficient of determination [
9]. There have also been studies conducted using fibroptic bronchoscopy to determine the length to the right and left main bronchus [
8,
10], as well as studies employing CT scans to identify the length to the main bronchus, but these studies did not go beyond finding the position for double-lumen tubes (DLT) [
11].
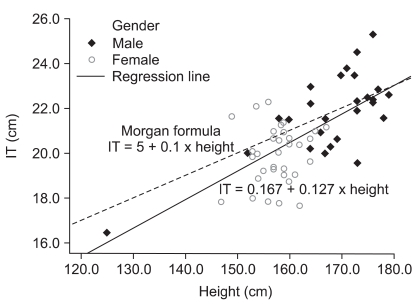
For ETI, the equation IT (cm) = 0.167 + 0.127 × height (cm) was compared to Morgan's equation, which is based on Western adults, to identify the length from the upper incisor to the midtrachea, and the results showed that the group of those below the average height of the Korean male adults (167.8-174.1 cm, National Physical Fitness Survey, 2009) had a lower value than westerners (
Fig. 3). Evaluation of the mean value revealed that the length between the upper incisor and the midtrachea in men was 21.8 ± 1.8 cm, while in women it was 19.9 ± 1.3 cm (
Table 3). This is lower than the previous intuitive measurements, where the length for men was 23 cm, and for women it was 21 cm [
6]. These results can be used to demonstrate and explain previous reports showing how ETI using Western standards can induce the side-effects of bronchial intubation [
7].
Different from the generally known values, the results of the presented research showed that the mean value of the most ideal ETI depth for Korean adults is 21.8 cm for men and 19.9 cm for women, and using this can minimize the possibility of bronchial intubation. Although the trachea is of a relatively standard length, the length between the upper incisor and the midtrachea differs by about 1.27 cm (IT [cm] = 0.167 + 0.127 × height [cm]) for every 10 cm difference in height; therefore, this must be considered when conducting ETI. Accordingly, when adjusting for the height difference, using the equation Length of tube (cm) = 0.167 + 0.127 × height (cm) will minimize the possibility of bronchial intubation.
Lee et al. [
17] evaluated the relationship between the height of men and women and ETI depth and found consistent meaningful results for the male group, but not for the female group. It is assumed that this is because the height distribution of Lee et al.'s female group was pooled towards 150 cm to 165 cm. The present study showed similar results, and the height distribution of the female group in the present study (157.9 ± 4.3 cm) also had a lower variance than that of the male group.
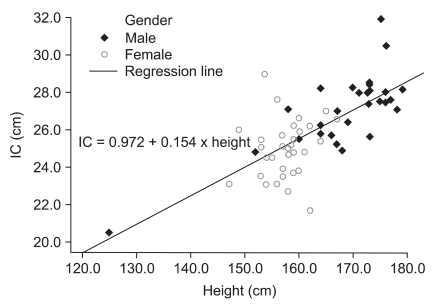
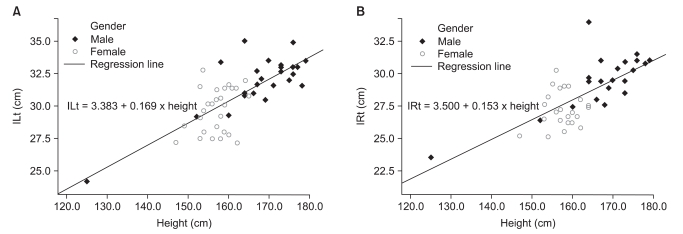
When using a double-lumen endotracheal tube (DLT), intubation is considered appropriate when the proximal bronchial cuff is at the left main bronchus [
18]. Brodsky et al. [
19] stated that when using a DLT, for a height of 170 cm, the mean intubation depth was 29 cm, and for each 10 cm height difference, the tube depth shifts 1 cm. The equations in the presented study, IC = 0.972 + 0.154 × height and ILt = 3.383 + 0.169 × height, were calculated by simple linear regression analysis. For 170 cm in height, the length from the upper incisor to the carina was 27.2 cm, while that to the left main bronchus was 32.1 cm. Additionally, for every 10 cm height difference, a shift of 1.5 cm in the tube depth was observed. When compared to the results of a study conducted by Brodsky, for a height of 170 cm, the length of the DLT used in Westerners and Koreans was similar. However, when shorter or taller than 170 cm, for every 10 cm there is a 0.5 cm difference. This is in line with the aforementioned discovery that there is a difference between Westerners and Koreans in the length between the upper incisor and the midtrachea of patients under the height 170 cm.
A study of the length of the trachea based on chest x-ray images was conducted in Korean children [
12], but this study was limited in that it was based on children admitted to the ICU who were intubated at the time. Thus the study was not based on the anatomical information of normal children. A study of the length between the upper incisor and the carina using a cuffless endotracheal tube was also conducted; however, the results were limited in that conclusive results were only shown with respect to the mean value, but not the correlativity [
13].
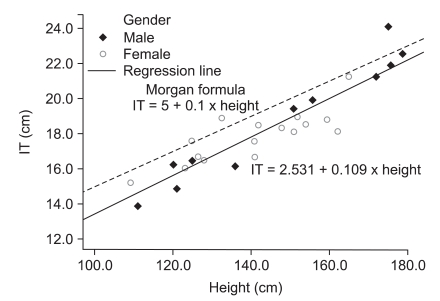
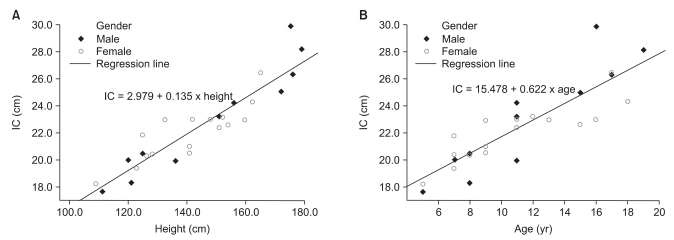
In Western children, the length between the upper incisor to the midtrachea is based on Morgan's equation, which is Length of tube (cm) = 0.1 × height (cm) + 5 [
14]. However, the present study evaluated Korean children using a simple linear regression analysis to identify an equation for the length between the upper incisor and the midtrachea (IT), which is IT (cm) = 2.531 + 0.109 × height (cm). When compared to Morgan's equation, this equation showed an approximately 1 cm difference (0.99-1.35 cm) for the average height range of the studied children (143.8 ± 20.4 cm) (
Fig. 6). This difference in children is greater than the difference that was observed between Western adults and Korean adults. This finding is significant for the standard measurements of ETI because children have shorter tracheas than adults. Moreover, Kim et al. [
20] found that the intubated tube moved in Korean children when the head was tilted up and down. Specifically, when the head was tilted up it moved 1.0 ± 0.5 cm, while it moved 1.8 ± 0.8 cm when the head was tilted down. When such findings were combined with the results of the present research, it is assumed the end of the tube may move 2.0-2.8 cm from the adequate midtrachea when the head is tilted up or down. Considering the length of the trachea in children, this much tube movement can entail the risk of bronchial intubation or the dislocation of the tube from the trachea. Therefore, when conducting ETI in Korean children, it is believed that Korean standard measurements, not the Western standard measurements, should be used for safe anesthetic management. Moreover, contrary to other measurements, the length of the trachea showed a higher coefficient of determination to age than to height, and in the aforementioned findings in adults, the relationship of the length of the trachea to age has no statistical significance. These findings indicate that, contrary to other parts of the airway, the length of trachea develops according to age. However, when a child develops into an adult and stops growing, the trachea is of the average length; thus, the aforementioned findings agree with this fact. Accordingly, the length of the airway is highly correlated with height in both children and adults, while it is highly correlated with age in children, but not in adults.
In conclusion, evaluation of a patient group electing for ophthalmic and ENT surgery revealed that the appropriate ETI depth based on measurements of Westerners needs to be reconsidered for the airway structure of Koreans. These results were confirmed by the finding that the previous intubation depth was too deep for the average Korean adults and children.
Overall, there is a need for a Korean-specific ETI standard. Because there may be a greater number of cases of unintended results such as bronchial intubation due to adhering to the previous standard than have been reported, a research study with a greater study population should be conducted.