|
 |
|
|
Abstract
Background
Methadone is a synthetic opioid that is widely used for the treatment of chronic pain. The association between methadone treatment and QT interval prolongation or which can lead to torsades de pointes has been confirmed with larger studies on high dose methadone. The aim of this study was to determine the effect of methadone on the QTc interval in patients, whether the daily dose of methadone should be lower than what has been previously investigated.
Methods
A total of 130 patients were included, with 90 patients in the methadone group and 40 patients in the control group. For each ECG, heart rate, QT interval and corrected QT (QTc) interval were recorded. The patient demographics, methadone dose and serum level, duration of methadone use and past medical history were collected.
Results
The QTc interval was significantly longer in the treatment group than in the control group (443 ± 30.0 ms versus 408 ± 28.0 ms, respectively, P < 0.0001) and more patients in the treatment group had a QTc interval greater than 450 ms (36.7% versus 7.5%, respectively, P = 0.0005). The QTc interval was not associated with methadone dose P = 0.9278), serum level (P = 0.2256) or duration of treatment (P = 0.1822).
Conclusions
This study has shown that methadone use is associated with longer QTc intervals, even among patients with daily doses of less than 80 mg. In this study, no correlation was found between QTc duration and methadone dose, serum levels or duration of use. However, the magnitude of the QTc interval was associated with female gender and the use of antidepressants.
Methadone is a synthetic opioid that is widely used for the treatment of chronic pain and as a substitute for heroin addiction. Although it is generally considered safe [1], a recent series of case reports have suggested an association between methadone treatment and QT interval prolongation or Torsades de pointes [2-8]. This association has been confirmed with large studies [9-15] and a retrospective analysis of the FDA MedWatch program [16]. The patients in these studies have generally been on high dose methadone (>120 mg/day). However, QT interval prolongation has been noted with daily doses below 65mg [5,8,11] and no cutoff value for a safe dose has been identified. Although some studies have found a positive correlation between methadone dose and the magnitude of QTc prolongation, the association is usually stronger when additional factors such as gender, length of treatment and concomitant drug use are accounted for [9,11-13,15].
The mechanism by which methadone increases the QT interval is blockade of the HERG potassium channel (also called "KCNH2"), which mediates cardiac repolarization [15,17]. Methadone undergoes hepatic metabolism by CYP3A4, whose serum concentration is increased in disease states with decreased hepatic function [18] or if drugs that interact with CYP3A4 are used simultaneously [19]. QT prolongation can also be caused by drugs that directly affect the HERG potassium channel, such as cocaine [20] and a variety of prescription drugs [19,21,22], or by hypokalemia [22]. In patients with these additional risk factors, QT prolongation can be seen even with low doses of methadone.
The aim of this study was to determine the effect of low dose methadone on the QTc interval in patients recruited from a chronic pain clinic, where the daily dose of methadone is lower than what has been previously investigated.
Approval for this study was obtained from Institutional Review Board. Patients were identified by a retrospective review of the electronic medical records of adult patients at pain clinic. Patients were included if they received methadone for treatment of chronic pain and had both a 12-lead electrocardiography (ECG) and a serum methadone measurement recorded during the study period. A control group of patients had a recorded 12-lead ECG, but had no past history of methadone use. Patients with a history of cardiac pathology (e.g. arrhythmia, heart block, etc) were excluded from the study. A total of 130 patients were included, with 90 patients in the methadone group and 40 patients in the control group. For each ECG, the heart rate, QT interval and QTc interval were recorded. All measurements were generated by an automated ECG machine. A prolonged QTc interval was defined as greater than 450 ms. The following data were collected from each patient's medical record: patient demographics (age, gender, height, and weight), methadone dose and serum level, duration of methadone use and past medical history. The use of the following medications was documented for each patient : analgesics, including narcotics, non-steroidal anti-inflammatory drug (NSAID) and antiepileptic drugs; antidepressants, including selective serotonin release inhibitor (SSRI), tricyclic antidepressants and selective norepinephrine release inhibitor, and benzodiazepines. Methadone serum levels were assumed to be steadystate, as all patients were prescribed a stable dose of methadone every six hours. All data were collected without regard to the patients' methadone treatment status.
The associations between QTc interval and methadone use (dose, serum level and duration) and continuous demographic data (height, weight, body mass index) were assessed using Pearson and Spearman correlation coefficients. The difference in QTc interval between methadone users and non-users was tested by ANCOVA and the difference in the incidence of prolonged QT interval was tested by logistic regression. Both were adjusted for effects of gender and concomitant analgesic use. The interaction between gender and methadone use was also tested with Tukey adjustment for gender subgroup comparisons. Prior to data collection, we estimated that a sample size of 90 patients in the treatment group would have 82% power to detect a Pearson correlation coefficient r = 30 between methadone dose and QTc interval. In addition, a control group of 40 patients would have 90% power to detect a difference of 20 ms in mean QTc between the methadone and control groups, assuming that the common standard deviation of the QTc is 35 [10]. The level of significance for all statistical analyses was set at P < 0.05 (2-tailed tests). All statistical analyses were performed using SAS version 9.
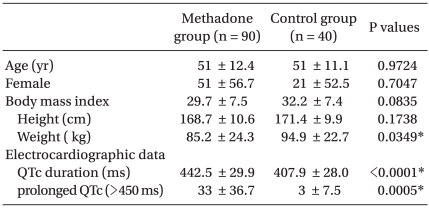
The treatment and control groups were similar in terms of gender distribution, age, height and BMI (Table 1), though actual weight was higher in the control group (94.9 kg versus 85.2 kg, respectively, P = 0.0349). The methadone dose in the treatment group ranged from 5-80 mg/day (median 30 mg/day) and the methadone serum level ranged from 10-348 ng/ml (median 81.5 ng/ml). The duration of methadone treatment ranged from 1-150 months (median 43 months).
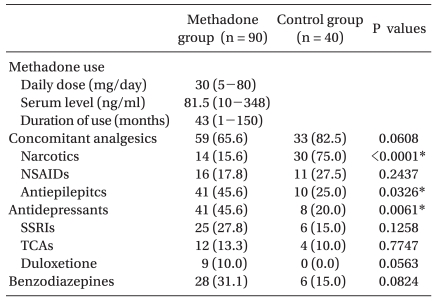
By unadjusted comparison, the QTc interval was significantly longer in the treatment group than in the control group (443 ± 30.0 ms versus 408 ± 28.0 ms, respectively, P < 0.0001) and more patients in the treatment group had a QTc interval greater than 450 ms (36.7% versus 7.5%, respectively). Four patients, all of whom were in the methadone group, had a QTc interval greater than 500 ms. In the methadone group, the QTc interval was not associated with methadone dose (P = 0.9278), serum level (P = 0.2256) or duration of treatment (P = 0.1822). The QTc interval was higher in females and shorter patients (P = 0.0061 and 0.0072, respectively), as well as patients who were taking antidepressants (P = 0.0397). However, the effects of gender and height were linked because there was a significant association between female gender and shorter height (P < 0.0001). To avoid autocorrelation, only gender was used in subsequent regression analyses. No significant association was found between QTc and age (P = 0.5470) or BMI (P = 0.7398).
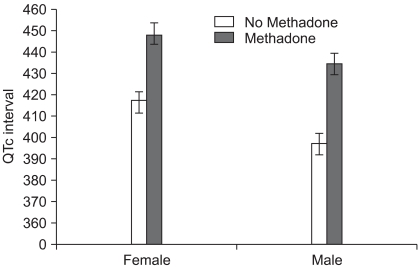
The difference in QTc interval between the two groups remained significant after adjusting for gender, the number of pain medications each patient was taking and the use of antidepressants (Table 2). The adjusted values for the treatment and control groups were 441.0 ms and 408.5 ms, respectively, with a mean difference of 32.5 ms (95% Confidence Intervals = 21, 44 ms). The methadone effect remained significant among gender subgroups, with average QTc values as follows: females on and off methadone 448 ± 27.4 ms and 417 ± 27.6 ms, respectively, and males on and off methadone 436 ± 32.0 ms and 397.4 ± 25.0 ms, respectively (P < 0.0001 for both). The interaction between methadone and gender was not significant (P = 0.97)(Fig. 1). The adjusted odds ratio for prolonged QTc interval (>450 ms) among methadone users was 7.2 (95% Confidence Intervals = 2.3, 31.8).
This study provides further evidence that methadone use is associated with prolonged QTc intervals, even at low doses (less than 80 mg/day). However, there was no association between the magnitude of the QTc interval and any of the quantitative methadone indices, including dose, serum level, and duration of use. The QTc interval was greater among females, shorter patients and those taking antidepressants. After adjusting for gender, the use of antidepressants and the number of pain medications each patient was taking, the estimated mean QTc interval was still 32.5 ms greater in the methadone group than in the control group (441.0 ms versus 408.5 ms, respectively). This effect was also seen in gender subgroup analysis, where QTc interval among methadone users was 30.5 ms and 38.1 ms greater than the control group for females and males, respectively. No instances of torsades de pointes were reported and all patients with a prolonged QT interval were clinically asymptomatic.
The upper limit of normal for QTc intervals has been inconsistently defined in the literature, with values ranging from 430 to 470 ms. However, absolute QTc values greater than 500 ms or changes from baseline greater than 30 ms have consistently been predictive of the development of drug-induced torsades de pointes [23]. It is strength of this study that the absolute QTc values are statistically different between the two groups, and that the results are not dependent on an arbitrary value that defines a prolonged QTc interval. All four patients who had absolute QTc values greater than 500 ms were in the methadone treatment group. However, no patient developed torsades de pointes, despite the increased risk for this complication. The adjusted QTc difference between the methadone and control groups was 32.5 ms, although this data alone is not sufficient to say that methadone caused an increase in the QTc interval because no baseline data was collected. However, given the similarity between the two groups in terms of demographics and concomitant medications, it is unlikely that the use of methadone did not contribute to these results.
The interaction between methadone dose and QTc duration has been investigated in a number of previous studies, most of which have included patients receiving a higher dose of methadone than those included in this study. Maremmani et al. [24] studied 83 patients receiving a mean daily methadone dose of 87 mg (10-600 mg/day). They found that 83% of patients had QTc values greater than standardized values for age and sex. However, no correlation was found between QTc duration and methadone dose. In a study of 138 patients receiving median dose of 170.9 mg/day (40-290 mg/day) of methadone, Peles et al. [10] found only a weak trend toward prologation of QTc duration with methadone dose, which did not reach statistical significance (r = 0.13, P = 0.1). Correlation between QTc duration and methadone serum levels was not demonstrated (r < 0.01, P = 1). These results are similar to our study, which also showed no correlation between these measures.
Some studies, however, have found a relationship between methadone dose and QTc duration. Ehret et al. [11] studied EKGs among 247 hospitalized patients, 167 of whom were receiving methadone (4-600 mg/day, median 100 mg/day). A weak, though statistically significant, correlation was found between methadone dose and QTc interval (r = 0.2, P < 0.01). Furthermore, QTc intervals of greater than 500 ms occurred with doses as low as 30 mg/day and among the six patients who developed torsades de pointes the average dose ranged from 40 to 200 mg/day. Similarly, our study contained four patients with QTc intervals greater than 500 ms who were receiving 20-40 mg/day of methadone. These findings highlight the difficulty in defining a safe range of methadone, as significant QTc prolongation can occur even at very low doses. Cruciani et al. [9] studied 140 patients receiving a median dose of 110 mg/day (20-1,200 mg/day) of methadone. They found that QTc was associated with an interaction between dose and duration. They found a dose x duration interaction (d = 0.86, P = 0.0009), which was significant only for males who had been receiving treatment for less than 12 months.
Martell et al. [12,13] have documented a change in QTc interval using baseline and follow-up EKGs after beginning methadone. In the first study, Martell et al. [13] analyzed EKGs from 132 patients at baseline and 2 months after beginning methadone therapy with doses from 30-150 mg/day. Over this period, the QTc increased by 10.8 ms (P < 0.0001) with greater changes among males and those receiving greater than 110 mg/day of methadone. In a follow-up study, Martell et al. [12] studied 160 patients at baseline and 6 and 12 months after starting therapy. The median methadone doses were 80 mg/day (20-180 mg/day) and 90 mg/day (20-200 mg/day) at 6 and 12 months, respectively. They found a significant correlation between methadone dose and the magnitude of QTc interval increase at 6 months (r = 0.18, P = 0.03), though the significance of this effect was marginal at 12 months (P = 0.08). However, the magnitude of QTc increase at 12 months was significantly associated with methadone serum trough (r = 0.37, P = 0.008) and peak levels (r = 0.32, P = 0.03). The average QTc change from baseline to 6 and 12 months was 12.4 ms (P < 0.001) and 10.7 ms (P = 0.001), respectively, both of which fall below the cut-off of 30 ms that defines the risk for torsades de pointes. Two patients had a QTc greater than 500 ms at each time point, but no patients developed torsades de pointes.
These studies have provided conflicting conclusions about the relationship between methadone dose and the QTc interval. Some have used a case-control design, while others collect data prospectively and analyze the impact of methadone use over time. Although either design provides valuable information, it is difficult to compare these studies. In addition, the range of methadone doses has varied considerably among these studies. It is possible that a correlation exists between methadone dose and QTc duration, but that studies such as ours, which include a very small range of doses, do not contain a large enough range of data for this correlation to become statistically significant. These studies have also differed with regards to the duration of methadone treatment. The results found by several authors [9,10,12,13] were dependent on the duration of methadone treatment and did not reach significance after 12 months. Peles et al. [10] hypothesized that the initial increase in QTc interval on starting methadone therapy may be an adaptation that does not continue linearly over time. Indeed, among the initial case reports of patients who presented with torsades de pointes, many patients had either recently initiated or increased their methadone dose [4-6]. The median duration of methadone therapy in our study was 43 months. Therefore, it is possible that no correlation was found between the duration of methadone treatment and the length of the QTc interval because of the length of time over which the patients in the study had been taking methadone.
In each study, methadone use has been associated with longer QTc intervals. However, in most cases, additional factors have been important in determining the length of the QTc interval. Ehret et al. [11] found that in addition to methadone dose, QTc prolongation was associated with hypokalemia, hepatic dysfunction and comedication with CYP3A4 inhibitors. In fact, when the other factors were considered synergistically, they were stronger predictors of QTc interval duration than the methadone dose. A model using all four of these predictors accounted for 31.8% of the QTc variability, indicating that other important factors had not been included. Although Peles et al. [10] did not find a significant correlation between methadone dose and QTc duration in their overall sample, a significant correlation was found among patients who tested positive for cocaine (r = 0.4, P = 0.003), which is known to block the HERG potassium channel that contributes to cardiac repolarization [19-22]. Krantz et al. [5] reported 17 patients who had developed torsades de pointes while receiving very high dose methadone (mean 397 mg/day). Among these patients, 14 had other potential risk factors for arrhythmia, including hypokalemia, the use of other drugs that interfered with methadone metabolism or directly prolonged the QT interval and structural heart disease. Similarly, in our study, the methadone indices were not correlated with the QTc interval. The only factors which were correlated with QTc interval were demographic variables and comedications.
The main limitation of this study is the lack of baseline patient data. Although the QTc measurements were significantly different between the two groups, we cannot say that methadone was associated with a change in QTc interval in the treatment group. Therefore, a follow-up study of QTc duration among low-dose methadone users at baseline and 6 and 12 months after beginning treatment will be conducted to determine the change in QTc duration in this patient population. In addition, some authors have noted that the QTc interval decreases after patients decrease their methadone intake [2,4,7,11]. This would be incredibly important among patients who have QTc intervals greater than 500 ms and are at greater risk for developing torsades de pointes. We will therefore collect follow-up data for patients in our clinic who decrease or stop their methadone to determine how the QTc interval responds to these changes.
This study has shown that methadone use is associated with longer QTc intervals, even among patients with daily doses of less than 80 mg. We have confirmed the findings of other studies, which have shown that the QTc interval is prolonged over a wide range of methadone doses and that no safe dose, below which QTc prolongation does not occur, has been found at this time. Although four patients in this study had QTc intervals greater than 500 ms, it is important to note that none had torsades de pointes or other adverse events due to their prolonged QTc duration. In this study, no correlation was found between QTc duration and methadone dose, serum levels or duration of use. However, the magnitude of the QTc interval was associated with female gender and the use of antidepressants.
References
1. Effective medical treatment of opiate addiction. NIH Consens Statement Online 1997; 15: 1-38.
2. Decerf JA, Gressens B, Brohet C, Liolios A, Hantson P. Can methadone prolong the QT interval? Intensive Care Med 2004; 30: 1690-1691. PMID: 15185068.


3. Lamont P, Hunt SC. A twist on torsade: a prolonged QT interval on methadone. J Gen Intern Med 2006; 21: C9-C12. PMID: 17026725.



4. Walker PW, Klein D, Kasza L. High dose methadone and ventricular arrhythmias: a report of three cases. Pain 2003; 103: 321-324. PMID: 12791438.


5. Krantz MJ, Lewkowiez L, Hays H, Woodroffe MA, Robertson AD, Mehler PS. Torsades de pointes associated with very-high-dose methadone. Ann Intern Med 2002; 137: 501-504. PMID: 12230351.


6. De Bels D, Staroukine M, Devriendt J. Torsades de pointes due to methadone. Ann Intern Med 2003; 139: E156PMID: 12859181.

7. Gil M, Sala M, Anguera I, Chapinal O, Cervantes M, Guma JR, et al. QT prolongation and Torsades de Pointes in patients infected with human immunodeficiency virus and treated with methadone. Am J Cardiol 2003; 92: 995-997. PMID: 14556883.


8. Piguet V, Desmeules J, Ehret G, Stoller R, Dayer P. QT interval prolongation in patients on methadone with concomitant drugs. J Clin Psychopharmacol 2004; 24: 446-448. PMID: 15232338.


9. Cruciani RA, Sekine R, Homel P, Lussier D, Yap Y, Suzuki Y, et al. Measurement of QTc in patients receiving chronic methadone therapy. J Pain Symptom Manage 2005; 29: 385-391. PMID: 15857742.


10. Peles E, Bodner G, Kreek MJ, Rados V, Adelson M. Corrected-QT intervals as related to methadone dose and serum level in methadone maintenance treatment (MMT) patients: a cross-sectional study. Addiction 2007; 102: 289-300. PMID: 17222284.


11. Ehret GB, Voide C, Gex-Fabry M, Chabert J, Shah D, Broers B, et al. Drug-induced long QT syndrome in injection drug users receiving methadone: high frequency in hospitalized patients and risk factors. Arch Intern Med 2006; 166: 1280-1287. PMID: 16801510.


12. Martell BA, Arnsten JH, Krantz MJ, Gourevitch MN. Impact of methadone treatment on cardiac repolarization and conduction in opioid users. Am J Cardiol 2005; 95: 915-918. PMID: 15781034.


13. Martell BA, Arnsten JH, Ray B, Gourevitch MN. The impact of methadone induction on cardiac conduction in opiate users. Ann Intern Med 2003; 139: 154-155. PMID: 12859171.


14. Krantz MJ, Lowery CM, Martell BA, Gourevitch MN, Arnsten JH. Effects of methadone on QT-interval dispersion. Pharmacotherapy 2005; 25: 1523-1529. PMID: 16232014.


15. Kornick CA, Kilborn MJ, Santiago-Palma J, Schulman G, Thaler HT, Keefe DL, et al. QTc interval prolongation associated with intravenous methadone. Pain 2003; 105: 499-506. PMID: 14527710.


16. Pearson EC, Woosley RL. QT prolongation and torsades de pointes among methadone users: reports to the FDA spontaneous reporting system. Pharmacoepidemiol Drug Saf 2005; 14: 747-753. PMID: 15918160.


17. Katchman AN, McGroary KA, Kilborn MJ, Kornick CA, Manfredi PL, Woosley RL, et al. Influence of opioid agonists on cardiac human ether-a-go-go-related gene K(+) currents. J Pharmacol Exp Ther 2002; 303: 688-694. PMID: 12388652.


18. Tegeder I, Lotsch J, Geisslinger G. Pharmacokinetics of opioids in liver disease. Clin Pharmacokinet 1999; 37: 17-40. PMID: 10451781.


19. Al-Khatib SM, LaPointe NM, Kramer JM, Califf RM. What clinicians should know about the QT interval. JAMA 2003; 289: 2120-2127. PMID: 12709470.


20. Ferreira S, Crumb WJ Jr, Carlton CG, Clarkson CW. Effects of cocaine and its major metabolites on the HERG-encoded potassium channel. J Pharmacol Exp Ther 2001; 299: 220-226. PMID: 11561083.

21. Redfern WS, Carlsson L, Davis AS, Lynch WG, MacKenzie I, Palethorpe S, et al. Relationships between preclinical cardiac electrophysiology, clinical QT interval prolongation and torsade de pointes for a broad range of drugs: evidence for a provisional safety margin in drug development. Cardiovasc Res 2003; 58: 32-45. PMID: 12667944.



22. Roden DM. Drug-induced prolongation of the QT interval. N Engl J Med 2004; 350: 1013-1022. PMID: 14999113.


23. Bednar MM, Harrigan EP, Ruskin JN. Torsades de pointes associated with nonantiarrhythmic drugs and observations on gender and QTc. Am J Cardiol 2002; 89: 1316-1319. PMID: 12031739.


24. Maremmani I, Pacini M, Cesaroni C, Lovrecic M, Perugi G, Tagliamonte A. QTc interval prolongation in patients on long-term methadone maintenance therapy. Eur Addict Res 2005; 11: 44-49. PMID: 15608471.


- TOOLS