|
 |
|
|
Abstract
A 34-year-old woman at 25 weeks 3 days was diagnosed with preterm labor and underwent an emergency cesarean section. The neonate did not cry or show any activity. The heart rate was 80 beats/min and the oxygen saturation on pulse oximetry (SpO2) was 77%. Immediately, positive pressure ventilation was delivered by T piece resuscitator, and then anesthesiologist performed endotracheal intubation. The neonate demonstrated severe cyanosis and the SpO2 dropped to 30%. Ventilation was not successful even after intubation, and we found neck crepitus, chest wall distension, and severe cyanosis on physical examination. We suspected tension pneumothorax and performed needle thoracentesis. The neonate was stabilized and transferred to the neonatal intensive care unit for further treatment, but expired on the 10th day of life. We report a case of pulmonary air leak developing tension pneumothorax, pneumomediastinum, subcutaneous emphysema in an extremely-low-birth-weight preterm infant immediately after birth.
Pulmonary air leak is caused by alveolar rupture and encompasses pulmonary interstitial emphysema, pneumothorax, pneumomediastinum, pneumopericardium, and subcutaneous emphysema [1]. Pulmonary air leak developing tension pneumothorax, pneumomediastinum, subcutaneous emphysema immediately at birth is very rare. However, it is medical emergency requiring prompt intervention. It is a life-threatening condition with high mortality and morbidity.
The prevalence of it has been reported to be about 1–2%, rising to 40% in neonate on mechanical ventilation [2]. The most common cause of pulmonary air leak in neonate is inadequate mechanical ventilation, but this report is about spontaneous pulmonary air leak in neonate without mechanical ventilation. Neonatal pulmonary air leak has been reported to be associated with extremely-low-birth-weight (ELBW), prematurity, low Apgar scores, requirement of resuscitation, and amniotic fluid or meconium aspiration [2,3,4].
We report a case of unexpected pulmonary air leak in a ELBW preterm neonate immediately after birth.
A 34-year-old woman, 169 cm, 72 kg, with no medical history presented to our hospital at 25 weeks and 3 days of gestation with preterm labor. The blood pressure was 126/74 mmHg and the heart rate (HR) was 91 beats/min. Ultrasound sonography showed the fetus had a breech presentation with a weight of 900 g and a HR of 150 beats/min. For the induction of general anesthesia for a cesarean section, we performed total intravenous anesthesia with 2% propofol and remifentanil. After delivery, the target blood concentration for 2% propofol and remifentanil were adjusted based on the patient's vital signs and bispectral index.
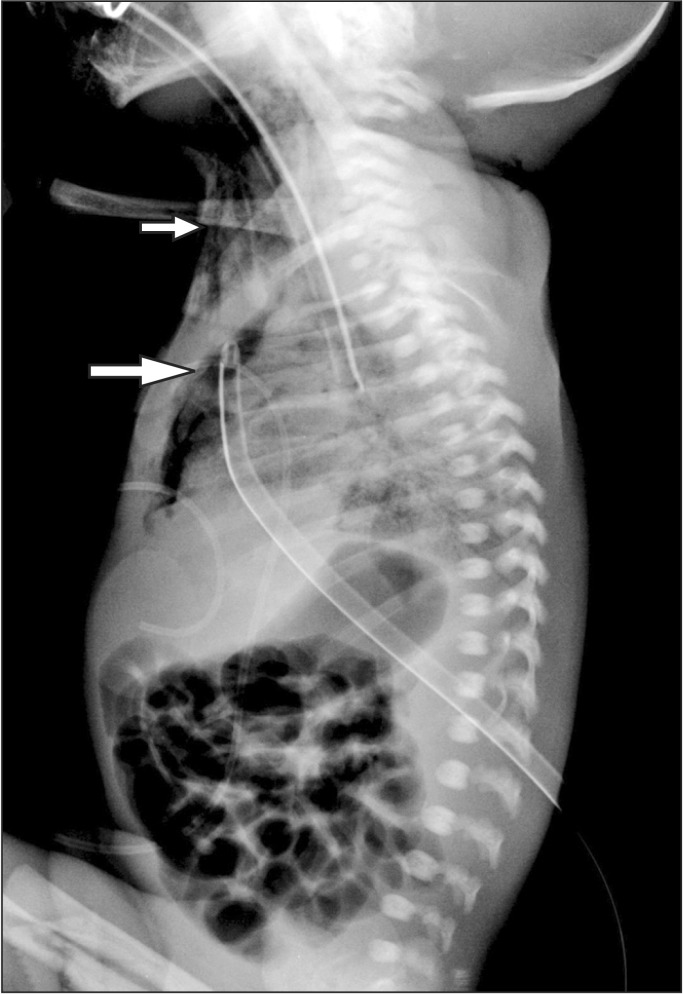
Induction-delivery time was 12 minutes, and uterus incision-delivery time was 5 minutes. The obstetrician started operation through small uterine incision since he expected small fetus. But it was difficult to delivery due to small incision and breech presentation. Fundal pressure was applied on patient's abdomen. The neonate was a 830 g, female with no abnormalities, but did not cry or show any activity with a HR of 80 beats/min and SpO2 of 77%. A breathing sound was not auscultated. The 1-minute Apgar score was 1. The pediatric resident conducted tracheal and oral suction. Positive pressure ventilation was delivered using T piece resuscitator (Neopuff®, Fisher and Paykel, Auckland, New Zealand). Peak inspiratory pressure (PIP) was 20 cmH2O, positive end expiratory pressure (PEEP) was 3 cmH2O. But the SpO2 dropped to 30%, HR was 95 beats/min, soft tissue swelling in the right supraclavicular area was observed. The anesthesiologist performed endotracheal intubation using a Miller #0 blade and a 2.5 uncuffed and successfully fixed the tube at a depth of 6.0 cm. There was no evidence of aspiration. However, the neonate's SpO2 was maintained at 40% even following intubation. On physical examination, aggravation of soft tissue swelling in the right neck, axillary, and supraclavicular areas were found and crepitus was palpable. Also, abdominal distension and severe cyanosis were observed concurrently. Upon diagnosis of right-sided tension pneumothorax, anesthesiologist was performed needle thoracentesis. Forty-six cc of air was aspirated in the 4th intercostal space of the midclavicular line using a 22-gauge angiocatheter. Following air aspiration, ventilation was achieved for both lungs, and the loss of edema in the neck area and reduction of subcutaneous emphysema were observed. The neonate's SpO2 gradually rose to 80% but the HR dropped to 59 beats/min. The pediatric resident began cardiac massage and administered 0.1 cc of 1 : 10,000 epinephrine into the endotracheal tube. The HR maintained at 180 beats/min and the SpO2 was 100%. The neonate was transferred to the neonatal intensive care unit. The thoracic surgeon inserted a 7 French chest tube, and began ventilator care. The neonate was diagnosed with right-sided pneumothorax, subcutaneous emphysema, and pneumomediastinum through the infantogram taken subsequently (Fig. 1). The neonate's respiratory distress syndrome became aggravated on postoperative day 10. The neonate expired on the 10th after birth.
Pulmonary air leak is caused by alveolar rupture due to excessive inflation as a result of generalized air trapping or uneven distribution of gas. The most common form of air leak syndrome is pneumothorax. Less commonly, localization of air in the pericardial space, subcutaneous tissue, or peritoneal space results in pneumopericardium, subcutaneous emphysema, and pneumoperitoneum [5,6].
The prevalence of it has been reported to be about 1–2%, rising to 40% in neonate on mechanical ventilation [2]. Neonatal pulmonary air leak is most prevalent on day 3rd of life [7]. Risk factors for pulmonary air leak has been reported to be associated with meconium aspiration syndrome, prematurity, amniotic fluid aspiration, surfactant deficiency syndrome, low Apgar score, infection, or the need for positive pressure ventilation during resuscitation at birth and use of high peak airway pressures on mechanical ventilation. Pulmonary interstitial emphysema that is a kind of pulmonary air leak is more commonly associated with continuous positive airway pressure therapy [8,9]. Pulmonary air leak is increased in preterm infants because the perivascular connective tissue in preterm is less dissectible and more abundant than older infants [10].
In this case, neonatal spontaneous tension pneumothorax is presumed to have occurred by excessive fundal pressure during delivery. Obstetrician needed to assist fundal pressure for fetal extraction due to small uterus incision and breech presentation. The assistant for delivery have to need many experiences to perform and coordinate fundal pressure maneuver properly. Sudden chest compression abruptly increases the alveolar pressure, which may cause alveolar rupture of neonate [11]. The neonate was stable before delivery but, neonate deteriorated immediately after birth. Pulmonary air leak was neonatal trauma that caused by excessive fundal pressure which encompasses the serial incidence of pneumothorax, pneumomediastinum, and subcutaneous emphysema.
Pneumothorax, the most common form of pulmonary air leak, can occur in neonate spontaneouly. This is most probably due to high transpulmonary pressure generated with the onset of breathing. During the first breaths of life, the transpulmonary pressure is about 40 cmH2O. Occasionally it can reach as high as 100 cmH2O. After the first few breaths, this pressure is normalized and lungs takeover the function. If this transpulmonary pressure remains higher for a long period of time, it leads to alveolar rupture and consecutive pneumothorax [12]. In this case, the neonate did not breath and oropharyngeal foreign material was removed by sufficient negative pressure suction. Also the neonate revealed no aspiration sign during intubation. Therefore, the possibility of air leak caused by high pulmonary pressure is low.
In addition, positive pressure ventilation was delivered using Neopuff during resuscitation. The target pressure for Neopuff was 20 cmH2O for PIP, 3 cmH2O for PEEP. Neopuff can provide target PIP and PEEP continously, therefore the possibility of alveolar rupture by excessive positive pressure ventilation is low.
Other possibility for the cause of air leak was tracheal injury and one lung ventilation. In this case, the neonate already showed symptoms of soft tissue swelling in the neck area and subcutaneous emphysema prior to endotracheal intubation. Intubation was performed by anesthesiologist who was experienced in many case of neonatal anesthesia. Also, bilateral breath sounds were auscultated following needle thoracentesis; we confirmed endobronchial tube depth by infantogram. Hence, the possibility of tracheal injury and one lung ventilation by endotracheal intubation is low. Pulmonary air leak developing tension pneumothorax, pneumomediastinum, subcutaneous emphysema immediately after delivery is very rare. Power and Clemens [13] reported that the diagnosis of pneumothorax within first day of birth in infants with a weight of less than 1,500 g is associated with 13 times higher mortality or bronchopulmonary dysplasia.
In conclusion, all procedure during delivery can cause unexpected adverse fetal outcome. Especially, infant that had low lung maturity and low birth weight premature can be demaged by surgical procedure for delivery. Anesthesiologists are required to provide care for babies like in this emergency situation. Therefore, closed monitoring about surgical procedure, early diagnosis and immediate treatment are important to the survival of the neonate in situations that call for resuscitation.
References
1. Jeng MJ, Lee YS, Tsao PC, Soong WJ. Neonatal air leak syndrome and the role of high-frequency ventilation in its prevention. J Chin Med Assoc 2012; 75: 551-559. PMID: 23158032.


2. Wariki WM, Mori R, Boo NY, Cheah IG, Fujimura M, Lee J, et al. Risk factors associated with outcomes of very low birthweight infants in four Asian countries. J Paediatr Child Health 2013; 49: E23-E27. PMID: 23282105.


3. Ngerncham S, Kittiratsatcha P, Pacharn P. Risk factors of pneumothorax during the first 24 hours of life. J Med Assoc Thai 2005; 88(Suppl 8): S135-S141. PMID: 16856433.

4. Sly PD, Drew JH. Air leak in neonatal respiratory distress syndrome. Anaesth Intensive Care 1984; 12: 41-45. PMID: 6703314.


5. Joseph LJ, Bromiker R, Toker O, Schimmel MS, Goldberg S, Picard E. Unilateral lung intubation for pulmonary air leak syndrome in neonates: a case series and a review of the literature. Am J Perinatol 2011; 28: 151-156. PMID: 20703979.



6. P S, J K. Preterm neonate with spontaneous pneumopericardium without any other associated air leaks. J Clin Diagn Res 2014; 8: 181-182.
7. Lim HS, Kim H, Jin JY, Shin YL, Park JO, Kim CH, et al. Characteristics of pneumothorax in a neonatal intensive care unit. J Korean Soc Neonatol 2011; 18: 257-264.

8. Al-Abdi SY, Singhal N. Pulmonary interstitial emphysema and continuous positive airway pressure in a premature infant. Saudi Med J 2005; 26: 1627-1629. PMID: 16228069.

9. Berk DR, Varich LJ. Localized persistent pulmonary interstitial emphysema in a preterm infant in the absence of mechanical ventilation. Pediatr Radiol 2005; 35: 1243-1245. PMID: 16086158.


10. Bas AY, Okumus N, Demirel N, Zenciroglu A. Persistent pulmonary interstitial emphysema in a preterm infant. Indian Pediatr 2008; 45: 775-777. PMID: 18820387.

11. Sharma A, Jindal P. Principles of diagnosis and management of traumatic pneumothorax. J Emerg Trauma Shock 2008; 1: 34-41. PMID: 19561940.



12. Chernick V, Avery ME. Spontaneous alveolar rupture at birth. Pediatrics 1963; 32: 816-824. PMID: 14075624.



13. Powers WF, Clemens JD. Prognostic implications of age at detection of air leak in very low birth weight infants requiring ventilatory support. J Pediatr 1993; 123: 611-617. PMID: 8410519.