 |
 |
|
|
Abstract
Background
Magnesium sulfate (MgSO4) has been used in the treatment of pre-eclampsia, hypertension and arrhythmia. Magnesium enhances the neuromuscular block of rocuronium. This study has been conducted to evaluate the reversal efficacy of sugammadex from deep rocuronium-induced neuromuscular block (NMB) during consistent pretreatment of MgSO4 in rabbits.
Methods
Twenty-eight rabbits were randomly assigned to four groups, a control group or study groups (50% MgSO4 150ŌĆō200 mg/kg and 25 mg/kg/h IV), and received rocuronium 0.6 mg/kg. When post-tetanic count 1ŌĆō2 appeared, sugammadex 2, 4, and 8 mg/kg was administered in the 2-mg group, control and 4-mg group, and 8-mg group, respectively. The recovery course after reversal of sugammadex administration was evaluated in each group.
Results
The mean serum concentration of magnesium was maintained at more than 2 mmol/L in the study groups, and the total dose of MgSO4 was more than 590 mg. The reversal effect of sugammadex on rocuronium-induced NMB in pretreated MgSO4 was not different from that in the group without MgSO4. The recovery time to train-of-four ratio 0.9 after sugammadex administration in the 2-mg group was longer than in the other groups (P < 0.001); there were no other significant differences among the groups.
Eclampsia is most common complication of pregnancy with hypertension and proteinuria, with an incidence of 6ŌĆō8% [1]. Magnesium sulfate (MgSO4) is used widely for the treatment and prevention of seizures in patients with eclampsia [2]. In the clinical field, to treat eclampsia, MgSO4 is initially bolus injected as a loading dose with 4 g and 2 g/h is infused as maintenance dose, such that the serum concentration of magnesium reaches 2.0ŌĆō3.5 mmol/L. MgSO4 enhances the effects of muscle relaxation on non-depolarizing neuromuscular blocking agents (NMBA) by depressing the acetylcholine release at the motor end plate within neuromuscular junction, decreasing the excitability of muscular fibers, and decreasing the electric potential amplitude at the end plate [3].
Sugammadex, a modified ╬│-cyclodextrin, is a selective relaxant-binding agent. Sugammadex achieves rapid reversal of muscle relaxation by forming a tight complex with unbound steroidal NMBA molecules, such as rocuronium or vecuronium. A deep neuromuscular block (NMB) by rocuronium (1ŌĆō2 post-tetanic counts [PTC]) is reversed with 4.0 mg/kg of sugammadex [4]. A deep NMB has various advantages. It can provide a better surgical field with lower intra-abdominal pressure than a moderate NMB (1ŌĆō2 train of four [TOF] counts), decrease postoperative pain and induce rapid recovery of bowel function [5]. It also improves the surgical view in microsurgery [6]. Czarnetzki et al. [7] reported that there was no effect of MgSO4 pretreatment on the sugammadex reversal for a deep NMB with rocuronium. However, this study was performed with one bolus injection of 60 mg/kg MgSO4 and the serum magnesium concentration was 1.5 mmol/L; this concentration was lower than the clinical concentration of 2.0ŌĆō3.5 mmol/L for eclampsia treatment. In addition, there were various limitations for the maintenance of constant serum concentrations of magnesium.
The aim of this study was to evaluate the effect of high serum magnesium concentration on the sugammadex reversal of a rocuronium-induced deep NMB in experimental animals.
After approval by our institutional animal care and use committee (CLAS MRCC HYU 2014-0069), we used 28 adult male New Zealand white rabbits, weighing 3.3ŌĆō3.8 kg (3.5 ┬▒ 0.2 kg). The animals were anesthetized with 100% oxygen (oxygen flow 200 ml/kg/min) and sevoflurane (Sevoflo┬« Abbott Laboratories Ltd, Kent, UK) using a face mask attached to a Bain circuit for the induction. Tracheal intubation with a 3.0 uncuffed tube was performed using a blind technique with the guidance of capnography [8] and the lungs were ventilated with an animal respirator (SN-480-5, Shinano Co., Ueda City, Japan). Ventilation was controlled to maintain end-tidal carbon dioxide ranging from 30ŌĆō35 mmHg, as measured by an ETCO2/SpO2 monitor (CO2SMO┬«, Novametrix Co., Wakefield, OH, USA), with a tidal volume of 25 ml/kg, a respiratory rate of 30ŌĆō35 breaths/min and inspiration time : expiration time (I : E) ratio of 1 : 2. To continuously monitor the end-tidal sevoflurane concentration between the intubation tube and the animal respirator, a gas analyzer (Datex-Ohmeda S/5 Anesthesia Monitor; GE Healthcare Finland, Helsinki, Finland) was used. The minimum alveolar concentration of sevoflurane was 3.7 ┬▒ 0.16% in rabbits; therefore, the end-tidal concentration of sevoflurane for maintenance of adequate anesthesia was controlled at 4% [9]. A common carotid artery was cannulated for monitoring arterial blood pressure and intermittent analysis of arterial blood gases. A four-limb electrocardiogram was used for heart rate monitoring.
The rabbits were randomly assigned to four groups (control group [n = 7], 2-mg group [n = 7], 4-mg group [n = 7], and 8-mg group [n = 7]). The position of all animals was supine. The right ear vein was cannulated for intravenous (IV) fluid and drug administration. In the control group, normal saline 5 ml/kg was infused for 20 minutes using a syringe pump 1 hour before the study. In the study groups (2-mg, 4-mg and 8-mg groups), 50% MgSO4 (50 mg/ml) 150ŌĆō200 mg/kg, which was diluted 10 times with normal saline, was infused using the same method as in the control group, and the maintenance dose of MgSO4 25 mg/kg/h was continuously infused to maintain a constant serum magnesium concentration (2.0ŌĆō3.5 mmol/L). Drug dosages were determined by the weight of the rabbit. The serum magnesium concentrations were measured before administration of MgSO4 and just before and after the study by sampling from the carotid artery. Arterial blood gas analysis was performed using a GEM-STAT┬« gas analyzer (Mallinckrodt Co., St. Louis, MO, USA). The rectal temperature of the rabbits was maintained at 38Ōäā using a thermostat (Blanketrol II, 222, Cincinnati Sub-Zero Co., Cincinnati, OH, USA) and a heat lamp.
The right hind leg was shaved, and a longitudinal incision was made along the anterior leg. Dissection was performed to expose the right tibialis anterior muscle and common peroneal nerve. The common peroneal nerve was stimulated supramaximally at the posterolateral aspect of the knee with a 0.2-ms square-wave stimulus from a peripheral nerve stimulator (Dual-Stim®, Life-Tech Inc, Stafford, USA). TOF stimulation was applied once every 10 s. The tendon of the tibialis anterior was attached to a force displacement transducer (45196A®, San-ei Co., Tokyo, Japan) with the use of 2.0 silk. The twitch response was quantified mechanomyographically with a preload tension (20 g). The mechanomyogram was recorded on a multichannel recorder (Biophysiograph 7748®, San-ei Co., Tokyo, Japan). NMB was quantified by the first twitch (T1) of the TOF and TOF ratio (T4/T1).
After a stable recording of neuromuscular transmission had been established for 20 min, rabbits in all groups received rocuronium 0.6 mg/kg. After the complete depression of twitch on TOF, PTC was measured every 6 min. When PTC 1ŌĆō2 appeared, sugammadex 4 mg/kg was administered as reversal agent in the control group and the 4-mg group, 2 mg/kg in the 2-mg group and 8 mg/kg in the 8-mg group. The twitch recordings were evaluated for the following variables: time from the end of the injection of rocuronium to maximal twitch suppression (onset); time from the end of the injection of rocuronium to the appearance of PTC 1ŌĆō2; time from the end of injection of rocuronium to recovery of T1 in the TOF to a value of 25%, 75%, and 95% of control twitch tension (T1 [25, 75, 95]); time from the end of the injection of rocuronium to a TOF ratio of 90% (TOF [90]). At the end of the study, animals were given a lethal dose of pentobarbital and potassium chloride by IV injection.
Statistical analyses were conducted using SPSS 17.0 for window (SPSS Inc., Chicago, IL, USA). To determine the sample size, the technique used in a report was employed [10]. The mean onset of rocuronioum was 0.5 ┬▒ 0.1 min in rabbits. A minimum detected difference of 20% was considered significant. A sample size of 7 in each group was calculated to be appropriate to achieve a power of 0.8 and an ╬▒ value of 0.05. One-way analysis of variance with post hoc Bonferroni correction was performed for multiple comparisons among groups. Differences were considered statistically significant at P < 0.05. All variables were expressed as mean ┬▒ SD.
Serum magnesium concentrations just before the study were 0.60 ┬▒ 0.12 mmol/L in the control group, 0.52 ┬▒ 0.05 mmol/L in the 2-mg group, 0.57 ┬▒ 0.07 mmol/L in the 4-mg group, and 0.54 ┬▒ 0.07 mmol/L in the 8-mg group (P = 0.302). After the loading dose injection (MgSO4 150ŌĆō200 mg/kg), serum magnesium concentrations were 2.73 ┬▒ 0.53 mmol/L in the 2-mg group, 2.98 ┬▒ 0.58 mmol/L in the 4-mg group, and 3.03 ┬▒ 0.26 mmol/L in the 8-mg group (P = 0.468). Just after the study, serum magnesium concentrations were 0.53 ┬▒ 0.10 mmol/L in the control group, 2.12 ┬▒ 0.23 mmol/L in the 2-mg group, 2.11 ┬▒ 0.18 mmol/L in the 4-mg group, and 2.13 ┬▒ 0.24 mmol/L in the 8-mg group (P < 0.001). Total doses of MgSO4 were 590 ┬▒ 97 mg in the 2-mg group, 655 ┬▒ 60 mg in the 4-mg group, and 653 ┬▒ 69 mg in the 8-mg group (P = 0.226). There were no differences in serum magnesium concentration and total dose between the study groups (Table 1).
The onset time of rocuronium in the study groups (2-mg group [0.43 ┬▒ 0.06 min], 4-mg group [0.42 ┬▒ 0.04 min] and 8-mg group [0.43 ┬▒ 0.04 min]) was significantly shortened than that in the control group [0.63 ┬▒ 0.1 min] (P < 0.001). The time for appearance of PTC 1ŌĆō2 in the study groups (2-mg group [30.0 ┬▒ 6.9 min], 4-mg group [26.4 ┬▒ 5.8 min] and 8-mg group [28.2 ┬▒ 7.5 min]) was significantly prolonged than in the control group [14.4 ┬▒ 4.2 min] (P < 0.001; Fig. 1, Table 2).
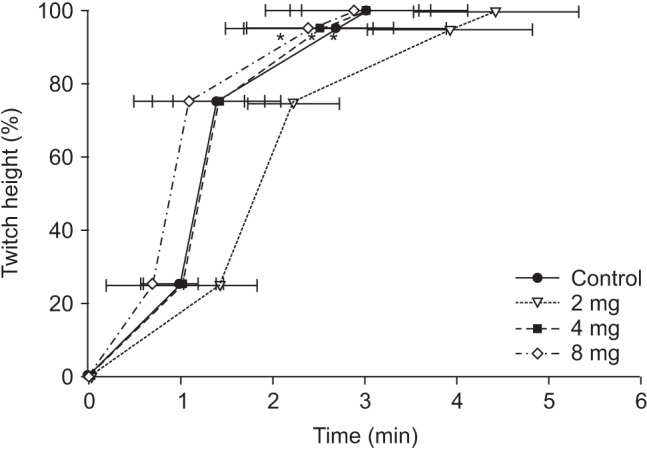
TOF [90] in the 2-mg group (2.03 ┬▒ 0.47 min) was significantly longer than in the other groups (1.31 ┬▒ 0.57 min in the control group, 1.24 ┬▒ 0.30 min in the 4-mg group, and 1.14 ┬▒ 0.40 min in the 8-mg group, P < 0.001; Table 2). T1 [75] in the 2-mg group (2.24 ┬▒ 0.45 min) was longer than in the other groups (1.44 ┬▒ 0.69 min in the control group, 1.43 ┬▒ 0.49 min in the 4-mg group, and 1.14 ┬▒ 0.58 min in the 8-mg group, P < 0.001). T1 [95] in the 2-mg group (3.93 ┬▒ 0.93 min) was longer than in the other groups (2.73 ┬▒ 1.23 min in the control group, 2.53 ┬▒ 0.78 min in the 4-mg group, and 2.44 ┬▒ 0.73 min in the 8-mg group, P < 0.001; Fig. 2, Table 2).
The hemodynamic data and ETCO2 were not different between all groups, and did not affect the results. These results were not displayed.
In this study, more than 590 mg of MgSO4 was required to maintain a serum magnesium concentration above 2.0 mmol/L. The onset time of rocuronium in the study groups was significantly shorter than in the control group and the time for appearance of PTC 1ŌĆō2 in the study groups was significantly longer than in the control group. In addition, TOF [90], T1 [75] and T1 [95] from the end of sugammadex injection in the 2-mg group were significantly extended relative to those in the other groups.
The normal range of serum magnesium concentration is 0.7ŌĆō0.9 mmol/L in humans [11] and 0.5ŌĆō0.8 mmol/L in rabbits [12]. The serum magnesium concentration in this study was 0.52ŌĆō0.60 mmol/L. Previous studies [7,13,14,15] found interactions between muscle relaxants and MgSO4 40ŌĆō60 mg/kg, which was single IV bolus administered. Therefore, these conditions were very different from eclampsia treatment, which requires a sustained serum magnesium concentration (2.0ŌĆō3.5 mmol/L) with a continuous infusion of MgSO4. Even in the study with humans, serum magnesium concentrations were not maintained at the level necessary to treat eclampsia [16]. In the current study, the loading dose of MgSO4 150ŌĆō200 mg/kg was administered for 20 min using a syringe pump before study, and a maintenance dose of MgSO4 25 mg/kg/h was continuously administered to resemble the clinical situation of eclampsia treatment, maintaining a constant serum magnesium concentration of 2.0ŌĆō3.5 mmol/L. Therefore, the effect of serum magnesium at the therapeutic concentration for eclampsia on the reversal of sugammadex could be evaluated.
An increase in serum magnesium concentration can induce hypotension. It is the results which magnesium directly antagonizes the calcium effect and acts to vascular smooth muscle and induces vasodilation. Indirectly, magnesium induces a sympathetic block and decreases vasomotor reflex and blood retention of peripheral veins, due to skeletal muscle relaxation. Finally, magnesium decreases venous return to the left ventricle and cardiac output [17]. However, in this study, there were no differences in blood pressure or heart rate between groups, regardless of sugammadex administration. The reason for this finding was not clear, but might be associated with the greater hemodynamic effect of an inhalational anesthetic agent other than magnesium.
In rabbits, the effective dose resulting in a 50% reduction of <twitch tension (ED50) and the effective dose resulting in a 95% reduction of twitch tension (ED95) are 61.5 ┬▒ 5.3 ┬Ąg/kg and 95.1 ┬▒ 6.7 ┬Ąg/kg, respectively [18]. Kim et al. [19] reported that the ED50 value of rocuronium for rabbits was 56.5 mg/kg, a level that was 40% of the level reported for humans [20]. Therefore, the dose of rocuronium was 0.6 mg/kg was used for a deep NMB, which is the same dose used for intubation in humans. MgSO4 administered 15 min before propofol anesthesia reduces the onset time of rocuronium by approximately 35% and prolongs the total recovery time by approximately 25% [7]. In the current study, the onset time of rocuronium 0.6 mg/kg in the study groups was significantly shorter than in the control group. This decrease in onset time might be associated with serum magnesium concentrations above 2.0 mmol/L. The onset time of rocuronium 0.6 mg/kg in humans is approximately 1.5 min [21]. The decreased onset time in rabbits might be due to the increased dose (7 ├Ś ED95) used in rabbits compared with the human dose (2 ├Ś ED95). The longer time (26ŌĆō30 min) for the appearance of PTC 1ŌĆō2 in the study groups compared to the control group (14 min) also might be associated with serum magnesium concentration levels. Clinically, the presence or absence of MgSO4 may have an effect on the emergent reversal with sugammadex after muscle relaxant.
The recommended dose of sugammadex is 2 mg/kg for a moderate NMB, which is determined by a TOF count above 2 twitches, 4 mg/kg for a deep NMB, which is determined by a PTC below 10, and 16 mg/kg for emergent reversal immediately after NMBA administration [22]. In this study, the dose of sugammadex for reversal was 4 mg/kg, because PTC was 1ŌĆō2 when sugammadex was administered. In addition, 2 mg/kg and 8 mg/kg of sugammadex were used to evaluate the efficiency of reversal with MgSO4 pretreatment.
Sugammadex could reverse a rocuronium-induced NMB in a dose-response manner, even among patients treated with MgSO4 [23]. Clinically, there was no effect of MgSO4 pretreatment on the sugammadex reversal for deep NMB with rocuronium [7]. In this study, T1 [95] in the control and the 4-mg group, which received identical doses of sugammadex, did not vary. These results meant that the pretreatment MgSO4 did not affect the reversal of sugammadex under the constant serum magnesium concentration of 2.0ŌĆō3.5 mmol/L in rabbits. In contrast, there was no difference in T1 [95] between the 4-mg group and the 8-mg group. This might be the result of a ceiling effect of sugammadex, although further study is needed. The prolongation of T1 [95] (3.93 ┬▒ 0.93 min) in the 2-mg group might be due to a dose of not a deep NMB but a moderate NMB.
TOF ratio represents a presynaptic receptor block, whereas a post-synaptic receptor block is expressed by a depression in the single twitch response [24]. In the presence of appropriate concentrations of sugammadex, only a low concentration of free NMBA remains in the neuromuscular junction and will preferentially block post-synaptic acetylcholine receptors. This could explain why, after an optimal dose of sugammadex, the recovery of the TOF ratio to 0.9 precedes the recovery of T1, and why the TOF ratio may be fully recovered when this is not yet the case for T1 [25]. When antagonizing with classical reversal agents (anticholinesterase drugs) or natural recovery, the time course of recovery from NMBA varies from the case with sugammadex; first, there is the full return of T1 and then recovery of the TOF ratio to 90% [10,26]. In this study, TOF [90] appeared at a time similar to T1 [75], and T1 [95] appeared later than TOF [90]. This might be due to the reversal nature of sugammadex.
One limitation of this study was that anesthetic maintenance was performed with sevoflurane. Inhalational anesthesia is more commonly used in clinical practice than intravenous anesthesia, so we used an inhalational anesthetic agent for anesthesia maintenance. However, although it remains equivocal [27,28], the effect of sevoflurane on the recovery of a neuromuscular blockade by rocuronium cannot be completely ignored. In addition, one report suggested that sugammadex could not be affected by inhalational agents [29]. Therefore, the effect of sevoflurane might be limited. Another limitation was that we tested only a small number (n = 7 in each condition) of rabbits in order to minimize sacrifice of the animals, based on Min et al. [10]. If the number of rabbits was increased after a measurement of sample size, significant results may be obtained. Although eclampsia occurs only in women, male animals have undergone in this animal study due to disturbances such as the menstrual cycle.
In conclusion, the reversal of sugammadex from a deep rocuronium-induced NMB during the constant serum magnesium concentration of 2.0ŌĆō3.5 mmol/L was not affected in rabbits. However, the reversal effect of sugammadex varied depending on the dose.
References
1. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol 2009; 33: 130-137. PMID: 19464502.


2. Sibai BM. Magnesium sulfate prophylaxis in preeclampsia: evidence from randomized trials. Clin Obstet Gynecol 2005; 48: 478-488. PMID: 15805803.


3. Lee C, Zhang X, Kwan WF. Electromyographic and mechanomyographic characteristics of neuromuscular block by magnesium sulphate in the pig. Br J Anaesth 1996; 76: 278-283. PMID: 8777111.



4. Jones RK, Caldwell JE, Brull SJ, Soto RG. Reversal of profound rocuronium-induced blockade with sugammadex: a randomized comparison with neostigmine. Anesthesiology 2008; 109: 816-824. PMID: 18946293.


5. Kim MH, Lee KY, Lee KY, Min BS, Yoo YC. Maintaining optimal surgical conditions with low insufflation pressures is possible with deep neuromuscular blockade during laparoscopic colorectal surgery: a prospective, randomized, double-blind, parallel-group clinical trial. Medicine (Baltimore) 2016; 95: e2920PMID: 26945393.



6. Kim HJ, Lee K, Park WK, Lee BR, Joo HM, Koh YW, et al. Deep neuromuscular block improves the surgical conditions for laryngeal microsurgery. Br J Anaesth 2015; 115: 867-872. PMID: 26582847.



7. Czarnetzki C, Tassonyi E, Lysakowski C, Elia N, Tram├©r MR. Efficacy of sugammadex for the reversal of moderate and deep rocuronium-induced neuromuscular block in patients pretreated with intravenous magnesium: a randomized controlled trial. Anesthesiology 2014; 121: 59-67. PMID: 24608361.


8. Flecknell P. Laboratory animal anaesthesia. 4th ed. New York, Elsevier. 2016, pp 33-37.
9. Scheller MS, Saidman LJ, Partridge BL. MAC of sevoflurane in humans and the New Zealand white rabbit. Can J Anaesth 1988; 35: 153-156. PMID: 3356052.


10. Min HK, Kim KS, Lee GS. Rocuronium-induced neuromuscular block after long pretreatment of magnesium sulfate in rabbits. Korean J Anesthesiol 2007; 52: 443-448.

11. Musso CG. Magnesium metabolism in health and disease. Int Urol Nephrol 2009; 41: 357-362. PMID: 19274487.


12. Barlet JP. Plasma calcium, inorganic phosphorus and magnesium levels in pregnant and lactating rabbits. Reprod Nutr Dev 1980; 20: 647-651. PMID: 7349435.


13. Fuchs-Buder T, Wilder-Smith OH, Borgeat A, Tassonyi E. Interaction of magnesium sulphate with vecuronium-induced neuromuscular block. Br J Anaesth 1995; 74: 405-409. PMID: 7734259.



14. Lampl E, Dandoy M. Priming of atacurium with magnesium. Br J Anaesth 1993; 70: 72.
15. James MF, Schenk PA, van der. Priming of pancuronium with magnesium. Br J Anaesth 1991; 66: 247-249. PMID: 1817630.



16. Groudine SB, Soto R, Lien C, Drover D, Roberts K. A randomized, dose-finding, phase II study of the selective relaxant binding drug, Sugammadex, capable of safely reversing profound rocuronium-induced neuromuscular block. Anesth Analg 2007; 104: 555-562. PMID: 17312208.


18. Park YJ, Kim KS, Lee GS. Neuromuscular interactions between mivacurium and rocuronium in rabbits. Korean J Anesthesiol 1998; 34: 686-693.

19. Kim KS, Shim JC, Jun JH, Lee KH, Chung CW. Rabbits treated with chronic isepamicin are resistant to mivacurium and rocuronium. Anesth Analg 1999; 88: 654-658. PMID: 10072022.


20. Diefenbach C, Nigrovic V, Mellinghoff H, Buzello W. Muscle relaxants. New substances and neuromuscular monitoring. Anaesthesist 1997; 46: 3-13. PMID: 9082865.


21. Foldes FF, Nagashima H, Nguyen HD, Schiller WS, Mason MM, Ohta Y. The neuromuscular effects of ORG9426 in patients receiving balanced anesthesia. Anesthesiology 1991; 75: 191-196. PMID: 1859007.


22. Kopman AF. Sugammadex: a revolutionary approach to neuromuscular antagonism. Anesthesiology 2006; 104: 631-633. PMID: 16571954.


23. Sakurai Y, Uchida M, Aiba J, Mimura F, Yamaguchi M, Kakumoto M. Reversal of rocuronium-induced neuromuscular blockade with sugammadex in patients for cesarean delivery treated with magnesium sulfate. Masui 2014; 63: 315-319. PMID: 24724442.

24. Bowman WC. Prejunctional and postjunctional cholinoceptors at the neuromuscular junction. Anesth Analg 1980; 59: 935-943. PMID: 6255826.

25. Staals LM, Driessen JJ, Van Egmond J, De Boer HD, Klimek M, Flockton EA, et al. Train-of-four ratio recovery often precedes twitch recovery when neuromuscular block is reversed by sugammadex. Acta Anaesthesiol Scand 2011; 55: 700-707. PMID: 21574968.


26. Kim KS, Jeon JW, Koh MS, Shim JH, Cho SY, Suh JK. The duration of immobilization causes the changing pharmacodynamics of mivacurium and rocuronium in rabbits. Anesth Analg 2003; 96: 438-442. PMID: 12538193.


27. Lowry DW, Mirakhur RK, McCarthy GJ, Carroll MT, McCourt KC. Neuromuscular effects of rocuronium during sevoflurane, isoflurane, and intravenous anesthesia. Anesth Analg 1998; 87: 936-940. PMID: 9768798.


28. Maidatsi PG, Zaralidou AT, Gorgias NK, Amaniti EN, Karakoulas KA, Giala MM. Rocuronium duration of action under sevoflurane, desflurane or propofol anaesthesia. Eur J Anaesthesiol 2004; 21: 781-786. PMID: 15678732.


29. Vanacker BF, Vermeyen KM, Struys MM, Rietbergen H, Vandermeersch E, Saldien V, et al. Reversal of rocuronium-induced neuromuscular block with the novel drug sugammadex is equally effective under maintenance anesthesia with propofol or sevoflurane. Anesth Analg 2007; 104: 563-568. PMID: 17312209.


Fig.┬Ā1
The time (min) for appearance of post-tetanic count 1ŌĆō2 given rocuronium 0.6 mg/kg during MgSO4 infusion (150ŌĆō200 mg/kg bolus and 25 mg/kg/h continuously) in rabbits. Individual points represent mean twitch height (% control). Data are mean ┬▒ SD. *P < 0.001 compared with the control group.
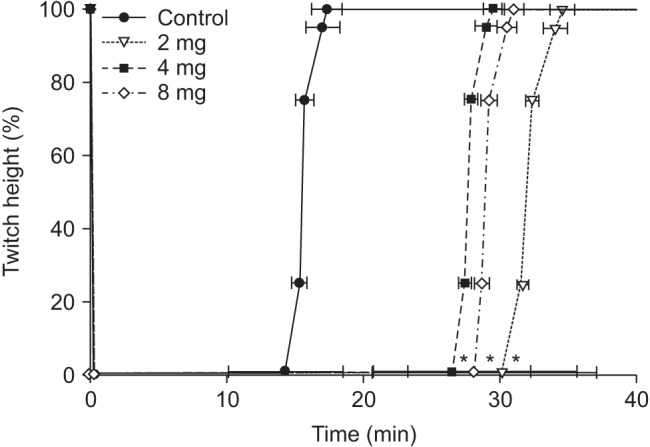
Fig.┬Ā2
The recovery time (min) after each dose of sugammadex at post-tetanic count 1ŌĆō2 from the relaxation given rocuronium 0.6 mg/kg during MgSO4 infusion (150ŌĆō200 mg/kg bolus and 25 mg/kg/h continuously) in rabbits. Individual points represent mean twitch height (% control). Data are mean ┬▒ SD. *P < 0.001 compared with the 2-mg group.
Table┬Ā1
Serum Magnesium Concentration (mmol/L) and Total Dose (mg) during MgSO4 Infusion (150ŌĆō200 mg/kg Bolus and 25 mg/kg/h Continuously) in Rabbits
Table┬Ā2
Onset and Recovery Times (min) of Rabbits Given Rocuronium 0.6 mg/kg after Reversal of Sugammadex during MgSO4 Infusion (150ŌĆō200 mg/kg bolus and 25 mg/kg/h Continuously)
Data are expressed as mean ┬▒ SD. Control: sugammadex 4 mg/kg, Group 2-mg: sugammadex 2 mg/kg, Group 4-mg: sugammadex 4 mg/kg, Group 8-mg: sugammadex 8 mg/kg. Onset: the time from injection of rocuronium to 100% twitch depression, PTC 1ŌĆō2: the time from injection of rocuronium to 1ŌĆō2 twitches of post-tetanic count (PTC), T1 [75], T1 [95]: the time from injection of sugammadex to 75% and 95% recovery of first twitch of train-of-four (TOF), respectively, TOF[90]: the time from injection of sugammadex to TOF ratio (T4/T1) of 90%. *P < 0.001 compared with Control group. ŌĆĀP < 0.001 compared with Group 2-mg.









