A rare case of Wilson disease associated with intracerebral hemorrhage
Article information
Wilson disease is an inherited autosomal recessive disease of copper metabolism that results in copper toxicity; it has an incidence of 1 in 40,000 [1]. Wilson disease is associated with liver failure; however, evidence on its bleeding tendencies is equivocal [2]. We present a case of Wilson disease with secondary parkinsonism and liver cirrhosis complicated by intracerebral hemorrhage (ICH), which has not yet been reported in the literature. Patient consent was obtained for this report.
A 35-year-old man, who had been diagnosed with Wilson disease two years earlier, presented with inability to sleep and increased tremors that had lasted for a month. He had secondary Parkinsonism along with child Pugh A liver cirrhosis that had lasted for 1 year. He also had bipolar disease and alcohol and cannabis abuse disorders, and was on regular follow-up at a psychiatric clinic. Clinically, he had extrapyramidal symptoms. Hematological investigations were essentially normal; however, biochemistry revealed a serum ceruloplasmin level < 9.5 mg/dl and 24-hour urinary copper level of 398.18 µg/day, which are consistent with Wilson disease. Ultrasonography of the abdomen revealed hepatomegaly with coarse echotexture and splenomegaly. Portal hypertension was diagnosed on the basis of color doppler flow imaging findings, and upper gastrointestinal endoscopy revealed small varices with severe portal hypertensive gastropathy and gastric antral vascular ectasia. At the time of reporting, the patient was undergoing zinc treatment for Wilson disease. He was admitted, and penicillamine treatment was initiated. His anti-parkinsonism treatment was also optimized. He was discharged after 1 week and scheduled for regular follow-up. One month after the initiation of penicillamine and while on follow-up, he developed pancytopenia with a hemoglobin (Hb) level of 12.8 g/dl total leukocyte count of 4.1 × 109/L and platelet count of 70 × 109/L. Given the pancytopenia, penicillamine was discontinued and the zinc tablet dosing was increased. At 1 week post-cessation of the penicillamine therapy, he had a left-sided focal seizure associated with extensor posturing of the right limbs and altered sensorium. On clinical evaluation, the patient had a pulse of 66 beats/min and blood pressure of 126/84 mmHg with a right gaze preference, extensor posturing, fixed dilated right pupil, and left pupil at 6 mm with sluggish reaction. Urgent non-contrast computed tomography of the head revealed a large left basal ganglia hemorrhage with an intraventricular extension (13-mm midline shift) and uncal herniation (Fig. 1). Anti-compression measures were initiated with mannitol. He was intubated and mechanically ventilated. Hematology revealed a Hb level of 9.4 g/dl and platelet count of 43 × 109/L with an international normalized ratio of 1.65. The external ventricular drain was placed following neurosurgical consultation, and blood component transfusion was administered with 6 units of random donor platelets and 4 units of fresh frozen plasma, which improved the platelet count to 53 × 109/L. However, even after 24 hours post-onset of neurological symptoms, there was no improvement in sensorium and brainstem reflexes. Intensive monitoring and care were continued, and additional blood products, including 10 units of random donor platelets and 6 units of fresh frozen plasma, were administered over the next 3 days. On the 5th day of admission, the patient developed sudden onset bradycardia followed by cardiac arrest, and he could not be revived.
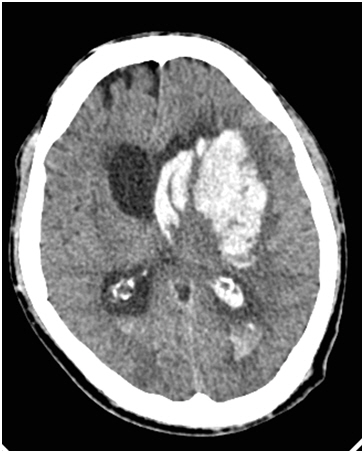
Non-contrast computed tomography image of the head showing a large left basal ganglia hemorrhage with intraventricular extension.
The literature has reports of abnormal liver functions with significantly decreased levels of factors II, V, VII, and X in Wilson disease patients [3]. Clinically, relevant coagulopathy due to primary pathology has not been reported. However, pancytopenia, including thrombocytopenia, is a known adverse effect of penicillamine therapy [4]. Deranged coagulation parameters with superimposed penicillamine-induced pancytopenia may be a cause of ICH as seen with our patient. Marijuana users are also more likely to be admitted for ICH; however, marijuana is not an independent risk factor for ICH [5]. Given the above findings, it is prudent to conclude that Wilson disease patients started on penicillamine should be strictly followed up to detect any bone marrow suppression at the earliest. As an anesthesiologist, coagulopathy should be looked for in each case of Wilson disease undergoing treatment with penicillamine during preoperative evaluation if anesthesia is being planned, and requisite blood should be secured before the procedure.
Notes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Shalendra Singh (Writing – original draft; Writing – review & editing)
Venigalla Sri Krishna (Conceptualization; Formal analysis)
Nipun Gupta (Supervision; Visualization)
Priya Taank (Conceptualization; Formal analysis)
Vikas Marwah (Resources; Supervision; Writing – review & editing)
