Comparison of the impact of applications of Targeted Transfusion Protocol and Massive Transfusion Protocol in trauma patients
Article information
Abstract
Background
The current study assessed a recently developed resuscitation protocol for bleeding trauma patients called the Targeted Transfusion Protocol (TTP) and compared its results with those of the standard Massive Transfusion Protocol (MTP).
Methods
Per capita utilization of blood products such as packed red blood cells (RBCs), fresh frozen plasma (FFP), and platelet concentrates was compared along with mortality rates during two 6-month periods, one in 2011 (when the standard MTP was followed) and another in 2014 (when the TTP was used). In the TTP, patients were categorized into three groups based on the presence of head injuries, long bone fractures, or penetrating injuries involving the trunk, extremities, or neck who were resuscitated according to separate algorithms. All cases had experienced motor vehicle accidents and had injury severity scores over 16.
Results
No statistically significant differences were observed between the study groups at hospital admission. Per capita utilization of RBC (4.76 ± 0.92 vs. 3.37 ± 0.55; P = 0.037), FFP (3.71 ± 1.00 vs. 2.40 ± 0.52; P = 0.025), and platelet concentrate (1.18 ± 0.30 vs. 0.55 ± 0.18; P = 0.006) blood products were significantly lower in the TTP epoch. Mortality rates were similar between the two study periods (P = 0.74).
Conclusions
Introduction of the TTP reduced the requirements for RBCs, FFP, and platelet concentrates in severely injured trauma patients.
Introduction
Trauma remains a major cause of mortality worldwide [1]. According to the available data, uncontrolled hemorrhage is responsible for about 40% of potentially preventable deaths following trauma, particularly in the first 24 hours post-injury [23]. Therefore, early identification of bleeding sources, efficacious hemorrhage control, and prompt resuscitation are needed to improve the outcome of trauma patients [24].
Uncontrolled post-traumatic bleeding frequently leads to a lethal triad of coagulopathy, hypothermia, and acidosis, events that further complicate resuscitation and operative control of hemorrhage [456]. The condition of each trauma case determines the individual need for specific blood products, including packed red blood cells (RBCs), fresh frozen plasma (FFP), and platelet concentrates (PCs), to treat hypovolemia due to hemorrhage. It is obvious that the use of these blood products in clinical practice should follow predetermined rules [789].
Parallel to improved understanding of the pathophysiology of trauma and hemorrhagic shock, the strategies used to manage these conditions have evolved over time [9]. Presently, standard massive transfusion protocols (MTPs) are most commonly used to resuscitate bleeding trauma patients in trauma centers [1011]. However, various studies have demonstrated conflicting results regarding the impact of these protocols on clinical outcomes [12131415161718]. In addition, the use of blood products in trauma cases can be risky. For example, despite the benefits of FFP in trauma patients with coagulopathy, some studies have shown adverse effects of it, including volume overload, acute lung injury, and nosocomial infections [18].
These issues have led to current, ongoing discussions about the ideal resuscitation strategy, and developing trauma resuscitation guidelines still remains a constant concern for trauma personnel. The trauma team at Shahid Rajaee Hospital, a high-turnover level-one trauma hospital affiliated with the Shiraz University of Medical Sciences, Shiraz, Iran, recently developed local algorithms for the resuscitation of bleeding trauma patients called the Targeted Transfusion Protocol (TTP). The goal of this single-center study was to compare the TTP algorithm with the previously used MTP guidelines.
Materials and Methods
Study protocol
This study was performed at Shahid Rajaee Trauma Center, a level-one main-referral trauma hospital in southern Iran, which is affiliated with the Shiraz University of Medical Sciences. The study protocol was approved by Iran's Ministry of Health and Medical Education (code: HMD/137; date: April 21, 2014) and the Shiraz University of Medical Sciences' Institutional Review Board. This study adhered to the Ethical Principles for Medical Research Involving Human Subjects, outlined in the Helsinki Declaration of 1975 (revised in 2000).
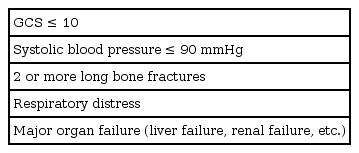
This study compared the numbers of RBC, FFP, and PC transfusions utilized during the 6-month period from the beginning of May to the end of October in 2011 (MTP) and again in 2014 (TTP). It should be noted that we did not use FVIIa in our center (due to its high cost and our limited resources). Trauma patients referred to the Shahid Rajaee Trauma Center's resuscitation room (Table 1) were prospectively included in this study.
A general practitioner under the supervision of an emergency medicine specialist was responsible for referring patients to the resuscitation room. In the hospital's resuscitation room, the general surgery team instigated either the standard MTP (in 2011) or TTP (in 2014). Notably, in both protocols, resuscitation was initiated using 2 L of crystalloids, after which blood products were transfused according to the protocol. The maximum amount of crystalloid transfusion was 3.5 L per day.
All blood samples were collected after patients entered the resuscitation room. The general surgery resident followed up and interpreted the laboratory results.
The neurosurgery team was actively involved in the management of head injury patients. A loss of consciousness or amnesia after injury, a Glasgow Coma Scale (GCS) score of less than 10, or clinical findings to suggest a skull bone fracture were considered to indicate a head injury. Such patients, just after stabilization of vital signs, underwent brain computed tomography (CT) scans. Those cases suspected of having a head injury whose vital signs did not stabilize (with a heart rate elevated over 120 bpm) after resuscitation with crystalloids and appropriate pain control were sent for brain CT scans accompanied by a general surgery resident who simultaneously performed resuscitation techniques.
Definitions
The following indices were used to compare blood products used during the two study time frames (based on the data from the entire hospital stay period):
Per capita requisition: the mean value of blood product requisition per patient during each one-month period. It should be noted that, in the standard MTP, blood products are prepared (and requested) in the form of shipments. However, in some cases, such as with an adequate response to resuscitation measures, all of these requested products may not be used and may end up being wasted.
Per capita consumption: the mean value of blood product consumption per patient during each one-month period.
Shahid Rajaee Hospital trauma resuscitation guidelines
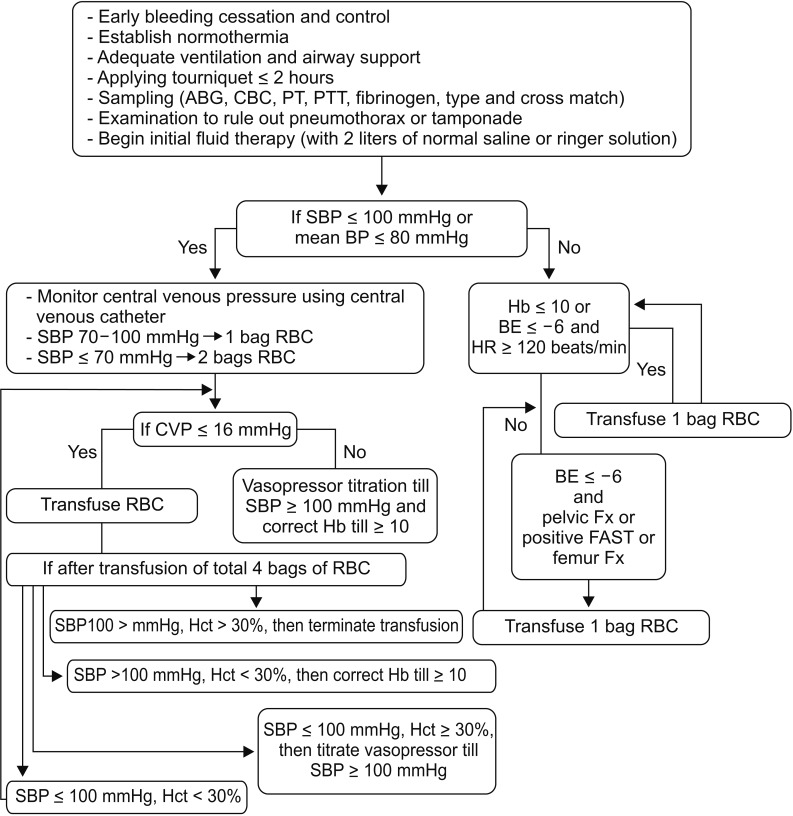
In 2011, the Shahid Rajaee Trauma Center followed a standard MTP for resuscitation of trauma patients (Fig. 1); however, in 2014, local guidelines for trauma resuscitation (Figs. 2, 3, 4) were followed.

Massive Transfusion Protocol (applied in 2011). ABG: arterial blood gas, CBC: complete blood count, PT: prothrombin time, PTT: partial thromboplastin time, INR: international normalized ratio, RBC: red blood cell, FFP: fresh frozen plasma.

Algorithm for blood product transfusions in multiple trauma patients without traumatic brain injury. ABG: arterial blood gas, CBC: complete blood count, PT: prothrombin time, PTT: partial thromboplastin time, SBP: systolic blood pressure, RBC: red blood cell, Hb: hemoglobin, BE: base excess, HR: heart rate, CVP: central venous pressure, FAST: focused assessment with sonography in trauma, Fx: fracture.
Algorithm for blood product transfusions in multiple trauma patients with traumatic brain injury. ABG: arterial blood gas, CBC: complete blood count, PT: prothrombin time, PTT: partial thromboplastin time, SBP: systolic blood pressure, Hb: hemoglobin (g/dl), BE: base excess, RBC: red blood cell, HR: heart rate, CVP: central venous pressure, Hct: hematocrit (%), Fix: fracture, FAST: focused assessment with sonography in trauma.

Algorithm for blood product transfusions in cases of penetrating trauma of the trunk, extremities, or neck without traumatic brain injury. BP: blood pressure, SBP: systolic blood pressure, CVP: central venous pressure, RBC: red blood cell, Hb: hemoglobin (g/dl), BE: base excess.
In accordance with the Shahid Rajaee Trauma Hospital local guidelines, patients were categorized into three groups:
Cases of multiple trauma without concomitant head injury.
Cases of multiple trauma with concomitant head injury.
Cases of penetrating trauma involving the trunk, extremities, or neck without concomitant head injury.
Patients meeting the above-mentioned criteria were resuscitated according to distinct guidelines (Figs. 2, 3, 4).
Additionally, fibrinogen has been used to resuscitate trauma patients with a fibrinogen level of less than 100 mg/dl since 2012.
Statistical analysis
Data were analyzed using descriptive statistics and the T-test (SPSS Statistics Software, version 16; Chicago, IL, USA). A P value of less than 0.05 was considered statistically significant.
Results
During the standard MTP study period in 2011, a total of 957 trauma patients were referred to Shahid Rajaee Trauma Center's resuscitation room. In the TTP period of 2014, a total of 1094 patients were referred to Shahid Rajaee Trauma Center's resuscitation room. All study participants had experienced a motor vehicle accident and had an injury severity score (ISS) of higher than 16.
There was no significant difference in the mean total number of admitted patients and the mean total mortality rates between the two study periods. Mortality status was compared between two groups using chi-square test (Table 2). However, the per capita utilization of RBC (4.76 ± 0.92 [mean total in 2011] vs. 3.37 ± 0.55 [mean total in 2014]; P = 0.037), FFP (3.71 ± 1.00 vs. 2.40 ± 0.52; P = 0.025), and PCs (1.18 ± 0.30 vs. 0.55 ± 0.18; P = 0.006) were significantly lower in the TTP epoch. The mortality rate was similar between the two study periods (P = 0.74). In addition, near-significant reductions in the per capita requisition of PC and per capita consumption of FFP were observed in this study.
The mean durations of hospital stay were similar in 2011 and 2014 (19 days for both periods). The mean ICU stay duration was 10.5 days in 2011 and 9 days in 2014.
Discussion
The results of the current study indicate that the introduction of TTP guidelines into clinical practice led to a statistically significant reduction in per capita utilization of RBC, FFP, and PC blood products compared with the use of a standard MTP. No impact on mortality was found.
Presently, the standard MTP is a blood product transfusion guideline widely used in trauma centers worldwide [1011]. This guideline was developed to ensure appropriate communication and coordination between medical services, including trauma and nursing teams, involved in the care of trauma patients who require a transfusion. The protocol provides an algorithmic approach to the transfusion of blood products and required laboratory studies in order to facilitate clinical care [19]. We developed new guidelines in order to reduce the quantity of blood products utilized. The current study indicated that clinical introduction of TTP algorithms successfully reduced the use of blood products; however, no change in mortality was observed.
Previous studies have shown that blood product transfusions used to resuscitate bleeding trauma patients may have some adverse effects. For example, Chaiwat et al. [20] found early RBC transfusions in trauma patients to be an independent risk factor for acute respiratory distress syndrome (ARDS) with a 6% increase in the risk of ARDS for each RBC transfusion. Accordingly, they recommended following a conservative RBC transfusion policy in trauma cases [20]. Another study by Acker et al. [21] reported an increased risk of death in children with traumatic brain injury following RBC transfusion. It has also been suggested that allogeneic blood transfusion in surgical patients is a major risk factor for the development of post-operative bacterial infection [22]. This risk factor is more significant in trauma cases than in elective surgical patients [22]. Adverse effects are also possible following the use of other blood products, such as FFP or PCs. For instance, they may cause transfusion-related acute lung injury (TRALI) [23]. Such adverse consequences were a main factor in the authors' decision to develop new algorithms for the management of bleeding trauma patients. According to this study, the TTP protocol can efficiently reduce the use of perioperative blood products, which helps to prevent transfusion-related complications, particularly TRALI [24].
One important aspect of any newly developed medical protocol is its cost-benefit ratio in the health-care system, which is more significant in centers with high admission numbers and high turn-over, such as the Shahid Rajaee Trauma Center. The U.S. Department of Health and Human Services' 2011 National Blood Collection and Utilization Survey Report indicated that, in 2011, hospitals paid an average of $225.42 per unit of leukocyte-filtered red cells, $57.91 per unit of plasma (frozen within 8 hours of phlebotomy), $535.17 per unit of apheresis platelets (leukocyte-reduced), and $62.41 per unit of cryoprecipitate [25]. The present study showed that clinical introduction of TTP algorithms can reduce costs by reducing the use of blood products. It should be noted that there was no difference between the standard MTP and TTP algorithms regarding the types of laboratory examinations, including coagulation, hematology, and blood gas tests. Another important point is that the TTP protocol resulted in the preparation of a reduced number of blood products by blood bank personnel, which lowered the blood bank workload. Nevertheless, further studies are required to explore these findings more comprehensively.
It should be noted that, during the study period from 2011 to 2014, there were no changes to the hospital's management system or medical facilities (except a change in resuscitation protocols) that could affect resuscitation measures or patient outcomes.
This study had some limitations. First, it did not compare possible changes in the amount of other types of blood products (such as cryoprecipitate and fibrinogen) that are used. Secondly, it would have been beneficial to compare the incidence of adverse effects (such as ARDS and nosocomial infection) in the two study periods. However, it should be noted that, in multiple injury patients, particularly those cases with a higher ISS, it is sometimes difficult to discriminate conclusively between transfusion-related morbidities and those morbidities that resulted from the traumatic event (for instance, TRALI versus lung contusion, fat emboli, or acute lung infections). Third, data on coagulation profiles were not compared between the two groups; this point should be considered in future studies. Another noteworthy issue of the current study is that we did not categorize the results based on the type of damage (head injury, long bone fracture, or penetrating injury). The consideration of this point in future studies will provide more detailed data regarding the benefits or pitfalls of the TTP protocol. Finally, as previously mentioned, further studies are needed to assess the effects of the TTP (compared with the standard MTP) on various costs that a health-care system and its patients may face.
In summary, the current study showed that TTP algorithms can significantly reduce the amount of blood products utilized compared to the standard MTP. However, further studies are necessary to examine various aspects of the clinical usage of the TTP protocol, including its cost-benefit ratio for health-care systems.