Use of the Disposcope endoscope for awake orotracheal intubation in an elderly patient with a large vocal cord polyp -a case report-
Article information
Abstract
Background
Vocal cord polyps are commonly encountered in the otorhinolaryngology department. The risk of anesthesia is high in patients with large vocal cord polyps. Awake intubation with appropriate airway tools provides a favorable safety profile.
Case
We present the case of a 60-year-old male patient who had been suffering from a large vocal cord polyp for 16 years. Electronic laryngoscopy revealed that the vocal cord polyp was approximately 1.5 cm in diameter. The polyp had a pedicle and demonstrated synchronous motion with respiratory excursion. It covered almost the entire glottic area during inspiration and moved away from the glottis during expiration. A Disposcope endoscope was used for awake tracheal intubation, and the surgery was completed successfully.
Conclusions
The Disposcope endoscope can be a useful option for awake orotracheal intubation in cases of anticipated difficult intubation and difficult facemask ventilation.
Vocal cord polyps occur commonly in the otorhinolaryngology department. Hoarseness is the predominant clinical manifestation. As the polyps grow larger, some patients develop symptoms such as dyspnea and even the inability to lie flat. Most vocal cord polyps are diagnosed and treated in the early stage; however, a small percentage of patients do not seek medical treatment until the polyps have caused dyspnea or begun to significantly affect their lives. Patients with large vocal cord polyps have a high risk of general anesthesia due to difficult intubation [1]. Intubation after the administration of potent sedatives or muscle relaxants may aggravate the airway obstruction caused by the polyp, which can lead to an emergency difficult airway [2]. In contrast, awake intubation has a good safety profile as both spontaneous ventilation and intrinsic airway tone are maintained before intubation [3]. In our reported case, awake tracheal intubation in an elderly patient with a large vocal cord polyp was performed using a Disposcope endoscope.
Case Report
Written informed consent was obtained from the patient and his family for the publication of this case report. Institutional review board exemption was obtained.
A 60-year-old male patient weighing 87 kg and 170 cm in height visited the otolaryngology outpatient clinic of our hospital for hoarseness and dyspnea. The patient had presented to our hospital 16 years prior with a chief complaint of hoarseness. At that time, the patient underwent electronic laryngoscopy, which led to the diagnosis of a vocal cord polyp. Consequently, a surgical procedure for vocal cord polyp resection using a self-retaining laryngoscope was scheduled. Due to inadequate airway assessment by the anesthesiologist, the tracheal intubation was difficult. Although the patient was successfully intubated using a traditional direct laryngoscope, the multiple tracheal intubations led to glottic edema, posing an increased surgical challenge and ultimately impeding successful surgical treatment of the vocal cord polyp. After discharge, the patient failed to seek further medical attention at an upper-level hospital. Sixteen years later, he visited the otolaryngology clinic of our hospital again with complaints of being unable to sleep on his back for long periods and worsened dyspnea.
The anesthesia-related physical examination revealed normal mouth opening and head and neck mobility. However, the patient’s thyromental distance was found to be < 6 cm, his airway was Mallampati class III, and he had a poor ability to prognath. Electronic laryngoscopy revealed a vocal cord polyp. The polyp had a pedicle and demonstrated synchronous motion with respiratory excursion. It covered > 90% of the glottic area during inspiration and moved away from the glottis during expiration (Figs. 1A-B).
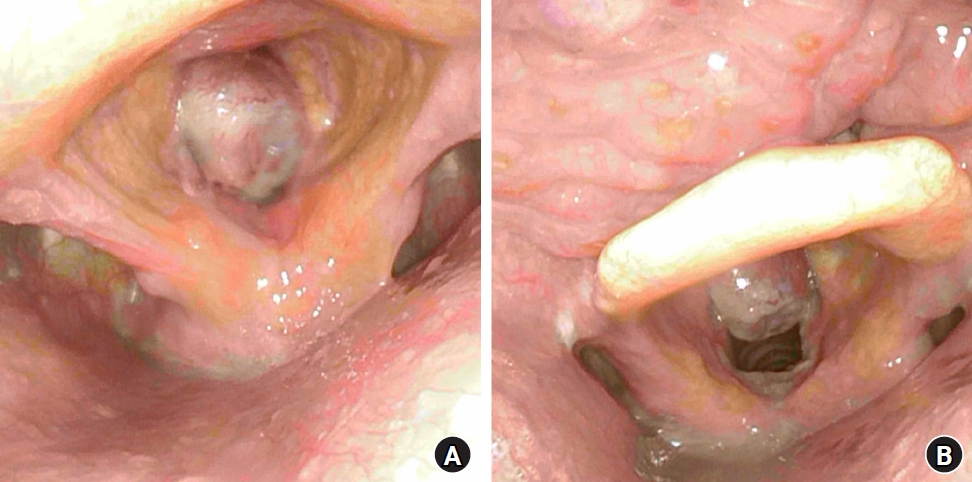
The polyp covering more than 90% of the glottic area during inspiration (A) and moving away from the glottis during expiration (B).
The patient received oxygen via a facemask at a flow rate of 5 L/min after entering the operating room, followed by intravenous dexmedetomidine at 1 μg/kg/h for 10 min, which was reduced to 0.5 μg/kg/h after the loading dose. Sufentanil (0.15 μg/kg) was also administered. First, the oral cavity, oropharynx, and larynx were anesthetized using 2% lidocaine. With the assistance of the Disposcope endoscope (5.0 mm OD, Disposcope TAIWAN, Hsinchuang, Taiwan) and epidural catheter (Fig. 2), the “spray-as-you-go” [4] method was used to fully anesthetize the base of the tongue, epiglottis, and glottis with 2% lidocaine, and 3 ml of 2% lidocaine was injected into the trachea through the cricothyroid membrane. The patient was asked to open his mouth wide, and endotracheal intubation was performed using the Disposcope endoscope. An endotracheal tube (5.5 mm ID, reinforced, Covidien LLC, Mansfield, USA) was passed through the glottis as the patient exhaled. During intubation, the clinician made sure to prevent the tube tip from touching the vocal cord polyp. The patient received intravenous propofol (100 mg), sufentanil (15 μg), and rocuronium (50 mg) immediately after tracheal intubation. The surgery was completed successfully (Figs. 3A-B), and the postoperative pathological report revealed a vocal cord polyp 1.5 cm in diameter. The patient returned to the hospital for electronic laryngoscopy one month after the operation and complete removal of the vocal cord polyp was confirmed (Fig. 3C).

The main body of the Disposcope endoscope and the epidural catheter are tied together tightly with sterile transparent tape. The red arrow indicates the tip of the epidural catheter.
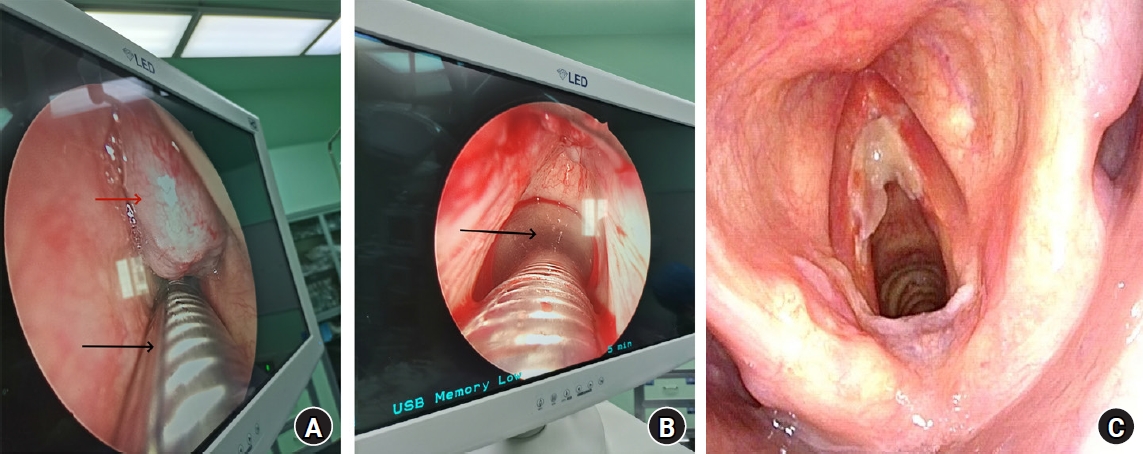
The surgical treatment of the patient. (A) Video-assisted self-retaining laryngoscope image of the surgical area at the beginning of surgery. The red arrow indicates the glottic mass, and the black arrow indicates the endotracheal tube. (B) The operation is almost complete and most of the glottic mass has been removed; the black arrow indicates the transparent cuff of the endotracheal tube. (C) Electronic laryngoscopy images of the patient one month after surgery.
Discussion
According to an extensive review of the relevant literature worldwide, patients with large vocal cord polyps of this size are relatively rare. Consequently, we conducted a comprehensive evaluation of the patient’s airway. The patient’s history of difficult tracheal intubation, body mass index, anatomical measurements, and preoperative electronic laryngoscopy results all suggested a difficult airway. The 2022 American Society of Anesthesiologists (ASA) Practice Guidelines for Management of the Difficult Airway recommend awake intubation be performed if the patient is suspected to have a difficult intubation and difficult facemask ventilation is anticipated [5]. If intubation is performed after the induction of general anesthesia, intubation failure may lead to displacement of the vocal cord mass, bleeding, and glottic edema [2]. Therefore, awake intubation was performed in this case to avoid difficult facemask ventilation owing to exacerbated respiratory obstruction. The ASA Difficult Airway Guidelines mention that the literature evaluating the optimal sequence of equipment to use during intubation for anticipated difficult airways and the most effective equipment to be attempted first after failed intubation is limited [5]. In the past, the primary choice for awake intubation in patients with anticipated difficult airways was flexible fiberoptics [6]. However, developing proficiency with fiberoptic intubation requires a rigorous learning process and the technique typically requires a substantial amount of time to perform [7]. With advancements in visualization technology, various types of video laryngoscopes and video stylets are now widely used to manage difficult airways. Compared with conventional direct laryngoscopy, video laryngoscopy has a higher intubation success rate, shorter intubation time, and fewer intubation-related complications. However, video laryngoscopy may not be appropriate for patients with limited mouth opening capacity or cervical spinal injuries. A recent study comparing the efficacy of flexible videoscopes, video laryngoscopes, and video stylets for orotracheal intubation under general anesthesia in patients with difficult airways found that video stylets and flexible videoscopes yielded higher rates of successful first-attempt intubations and better glottic exposure than video laryngoscopes [8]. Additionally, the use of video stylets for endotracheal intubation resulted in a significant reduction in intubation time compared with both the video laryngoscope and flexible videoscope. Therefore, we recommend the use of a video stylet as the first choice for difficult airway management. Another previous study found that in patients undergoing oral and maxillofacial surgeries, the required procedural time was reduced when nasotracheal intubation was performed using a Disposcope endoscope (which is a type of video stylet) compared with fiberoptic bronchoscopy [9]. Prolonged awake intubation may increase the risk of loss of airway patency in patients owing to the use of sedative and analgesic drugs. In addition, prolonged intubation may increase patient discomfort and the stress experienced by the anesthesiologist [7]. Although the monitors of most video stylets are connected to the stylet, the Disposcope endoscope transmits images wirelessly to the portable screen. Thus, the screen does not move as a result of maneuvering and advancing the tube during the procedure, facilitating the anesthesiologist’s capacity to observe and manipulate effectively. However, the Disposcope endoscope does have some limitations, such as the lack of a working channel for suctioning secretions, which may compromise visualization if considerable secretions are present. This limitation can be overcome by positioning the lens at the Murphy’s orifice of the tracheal tube without moving the lens over the tip and by improving the operational skill [8]. Although Disposcope endoscopes have recently been used for awake nasotracheal intubation [10], to date, reports on the use of Disposcope endoscope for awake orotracheal intubation are limited.
For this case, the epidural catheter was tightly attached to the Disposcope endoscope. As the special shape of the endoscope is consistent with that of the airway, the tongue base, epiglottis, and glottis can be fully anesthetized. Adequate topical anesthesia of the airway can improve the patient’s tolerance to intubation and minimize the stress response. For this case, we chose an endotracheal tube with an inner diameter of 5.5 mm given the large size of the polyp and our concern that a large tube would not pass smoothly through the glottis or would cause the polyp to fall off. In clinical practice, we have observed that passing the Disposcope endoscope, which is tightly attached to the epidural catheter, through the interior of an endotracheal tube with an inner diameter of 5.5 mm can be difficult, even when it is lubricated with liquid paraffin. In this case, the Disposcope endoscope had to be used twice during intubation: first during adequate topical anesthesia of the airway and again during tracheal intubation. If the inner diameter of the tracheal tube is larger than 5.5 mm, a Disposcope endoscope can be used to simultaneously complete topical anesthesia of the airway and tracheal intubation (Figs. 4A-B). To the best of our knowledge, this is the first study to report the use of a Disposcope endoscope to assist in topical anesthesia of the airway. In the future, we aim to develop removable, disposable consumables mounted on video stylets for topical airway anesthesia.
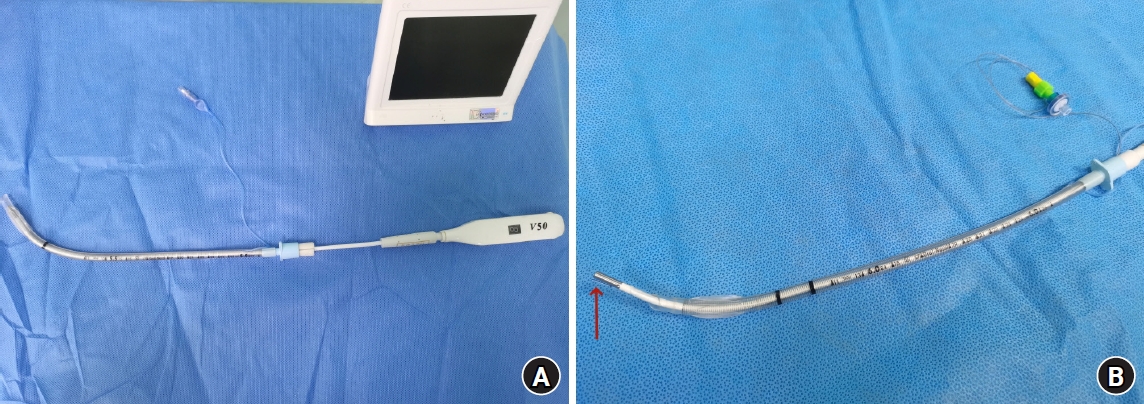
Preparation before awake intubation using the Disposcope endoscope. (A) The main body of the Disposcope endoscope is inserted into the 5.5 mm ID endotracheal tube. (B) The epidural catheter, tightly tied to the main body of the Disposcope endoscope, is inserted into the 6.0 mm ID endotracheal tube. The red arrow indicates the tip of the epidural catheter.
In conclusion, we suggest that awake orotracheal intubation with the Disposcope endoscope can be a useful option for anticipated difficult intubation and difficult facemask ventilation. Future studies should focus on exploring the value of the Disposcope endoscope in various clinical settings.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Author Contributions
Duo Yang (Writing – original draft; Writing – review & editing)
Sen Li (Data curation; Investigation)
Jinxin Lan (Writing – original draft)
Shujun Ye (Formal analysis; Investigation)
Longsheng Zhang (Methodology; Writing – original draft; Writing – review & editing)
