Comparison of effects of telmisartan versus valsartan on post-induction hypotension during noncardiac surgery: a prospective observational study
Article information
Abstract
Background
Telmisartan is considered more potent than valsartan. Hemodynamic response during anesthesia induction may be influenced by anti-hypertension (HTN) medication. The present study compared the effect of anti-HTN medications on post-induction hypotension during noncardiac surgeries.
Methods
This observational study standardized the anesthetic regimen across patients, with hypotension defined as mean blood pressure (BP) of less than 65 mmHg. The hemodynamic changes within 5 min before and after endotracheal intubation, and within 10 min before and after surgical incision were measured. Transthoracic echocardiographic evaluation of the left ventricle (LV) during anesthesia induction was performed. The primary endpoint was the decline in mean BP after anesthetic administration in telmisartan and valsartan groups. Multivariate logistic regression analysis was used to identify predictors of post-induction hypotension.
Results
Data from 157 patients undergoing noncardiac surgery were analyzed. No significant differences were found in mean BP decline between the two groups during anesthesia induction. Hemodynamic changes and LV ejection fraction (EF) during anesthesia induction were similar between the groups. Age and preoperative initial mean BP in operation room (OR) were associated with post-induction hypotension in both groups.
Conclusions
The angiotensin receptor blocker (ARB) type did not influence post-induction hypotension during anesthesia induction. Age and preoperative initial mean BP in OR were associated with post-induction hypotension in patients taking ARBs.
Introduction
Angiotensin receptor blockers (ARBs) are commonly used as effective first-line anti-hypertension (HTN) medications [1,2]. Recent guideline recommend ARBs as the primary anti-HTN treatment [3]. The hemodynamic effects of ARBs can vary based on their potency. Several studies have assessed the efficacy of ARBs in managing daily blood pressure (BP) [4,5]. Telmisartan stands out among ARBs because of its potency and prolonged duration of action compared to valsartan [6–8].
Fluctuations in hemodynamic response are common during anesthesia induction, often influenced by various factors. Typically, there is an initial decline in BP after anesthetic administration, followed by an increase after endotracheal intubation. Preoperative medications can significantly influence these hemodynamic responses. However, few studies have evaluated the hemodynamic responses related to specific ARBs during anesthesia induction.
We hypothesized that the hemodynamic response might differ based on the ARB type administered preoperatively. This study compared post-induction hypotension in patients taking telmisartan or valsartan as anti-HTN medication during non-cardiac surgery.
Materials and Methods
Study population
This was a prospective observational study of patients undergoing surgery under general anesthesia. The study protocol was approved by the Institutional Review Board (Konkuk University Medical Center, Seoul, Korea; Approval No, KUH1160077) which confirmed that the study was performed in accordance with the ethical standards of the Helsinki Declaration-2013, and was registered at http://cris.nih.go.kr (KCT0001595) prior to patient enrolment. All patients provided written informed consent before participation in the study. Patients who had been taking telmisartan or valsartan for a minimum of four weeks prior to the surgery were included. To further refine the study cohort, only those aged > 40 years, requiring general anesthesia for elective surgery, in the supine position, and classified as American Society of Anesthesiologists Physical Status (ASA-PS) class 2 were enrolled. The exclusion criteria were the use of either beta-blockers (BB) or calcium channel blockers (CCB), history of congestive heart failure (CHF), coronary artery disease (CAD), peripheral artery occlusive disease, cerebral infarction or hemorrhage, cardiac arrhythmia, orthostatic hypotension, and intraoperative change in position (Trendelenburg or reverse Trendelenburg position, beach chair position, prone position, or lateral position). Patients with abnormal intraoperative transthoracic echocardiographic measurements, such as poor echocardiographic view, left ventricular (LV) ejection fraction (EF) < 45%, and regional wall motion abnormality of LV wall, prior to anesthetic administration were excluded from further analysis.
Patients were allocated into two categories; those taking telmisartan (Telmisartan group) and those taking valsartan (Valsartan group). To optimize the effect of ARBs during anesthesia induction, all patients took their usual dose on the morning of the surgery. Anesthetists, surgeons, and nursing staff who participated in patient care were blinded to the study. Data were collected by trained observers who were blinded to the study and did not participate in patient care.
Anesthetic technique
No premedication was administered to any of the patients. Following standard monitoring, each patient was given an intravenous bolus infusion of 5 ml/kg balanced electrolyte solution before anesthesia induction. The anesthetic regimen remained consistent across all patients. Standard monitoring included electrocardiography, noninvasive BP monitoring, and pulse oximetry. Bispectral index monitoring was used to assess the depth of anesthesia. For anesthesia induction, 0.5 mg/kg lidocaine, 3 μg/ml propofol [9], and 5 ng/ml remifentanil using target control infusion (TCI) [10] set to last 5 min, were administered. Rocuronium (0.6 mg/kg) was administered for neuromuscular blockade, guided by peripheral neuromuscular transmission monitoring. Once the target plasma concentrations of propofol and remifentanil were achieved, endotracheal intubation was performed. Patients were subsequently ventilated using volume-controlled ventilation, maintaining tidal volume of 6 ml/kg and a positive end-expiratory pressure of 5 cmH2O.
Hemodynamic management
Hypotension was defined as a mean arterial BP < 65 mmHg. From the time of propofol administration to 10 min after surgical incision, hemodynamic management was performed as follows: if the mean BP was less than 60 mmHg, 50 μg phenylephrine was administered intravenously; if the systolic BP was higher than 180 mmHg, 200 μg nicardipine was administered intravenously; if the heart rate (HR) was less than 40 beats/min, 4 mg ephedrine was administered intravenously. From the surgical incision to skin closure, if the mean BP was below 65 mmHg, a continuous intravenous infusion of phenylephrine was started with the dose adjusted to maintain a mean BP ≥ 65 mmHg.
Clinical measurements
The total amounts of anesthetic agents used during anesthesia induction were recorded. The total duration of anti-HTN medication, the interval between anti-HTN medication administration on the morning of the surgery and anesthesia induction, the entire anesthesia induction period, and the total anesthesia and surgical duration were measured. Preoperative laboratory values were also recorded.
Noninvasive BP and HR measurements were performed on the morning of the operation. After entering the operation room (OR), noninvasive BP measurements continued every minute from the start of patient monitoring to 5 min after surgical incision, and then every 2.5 min during the surgery. Hemodynamic values were recorded at several time points: the morning of the operation (Ward), the first hemodynamic monitoring values in OR (Initial OR), within 5 min before and after endotracheal intubation (Pre- and Post-intubation, respectively), and within 10 min before and after surgical incision (Pre- and Post-incision, respectively). Other monitored variables included the decline in mean BP after anesthetic administration, the incidence of mean BP < 65 mmHg, and the incidence of out-of-range mean BP, defined as 20% higher or lower than the baseline mean BP on the morning of the operation. The incidences of hemodynamic agent usage during anesthesia induction and phenylephrine infusion during the operation were also recorded.
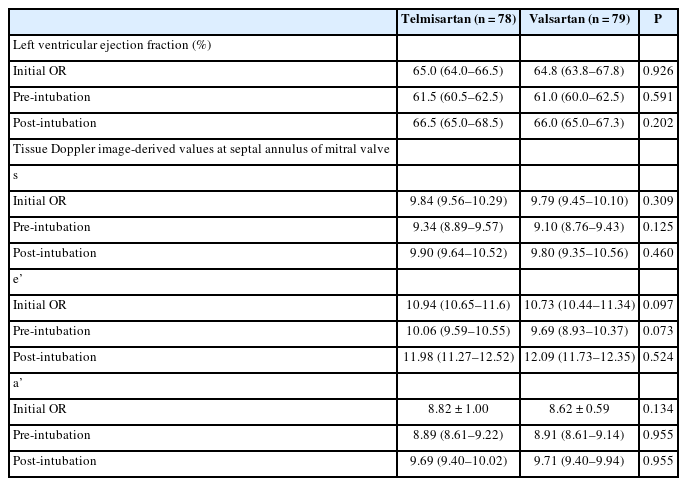
Transthoracic echocardiography (TTE) examination
During anesthesia induction in the supine position, serial transthoracic echocardiography (TTE) evaluations were conducted using a 5 MHz transducer on a GE VividTM 7 (GE Healthcare). These measurements coincided with the hemodynamic value recording times, i.e., Initial OR, Pre-intubation, and Post-intubation. All TTE values were recorded at the end of the expiratory phase to exclude respiratory influences. These included left ventricular ejection fraction (LVEF) and tissue Doppler image (TDI) with pulsed wave Doppler in a two-dimensional image of the apical four-chamber view. LVEF was determined using the modified Simpson’s method. TDI derived velocities of upward deflection during the systolic phase (s), along with the downward deflection during the early diastolic phase (e’), and the late diastolic phase (a’) were measured at the septal annulus of the mitral valve (MV) from an average of 2 beats. A single cardiac anesthesiologist performed all TDI assessments that were subsequently reviewed by two independent anesthesiologists.
Statistics
The primary outcome was the difference in mean BP decrease from Initial OR to Post-incision between the Telmisartan and Valsartan groups. Based on the pilot study involving 18 patients, the mean BP decrease was 20.8 ± 5.2 mmHg and 24.6 ± 9.8 mmHg in the Telmisartan and Valsartan groups, respectively. A priori power analysis revealed an effect size of 0.47, resulting in a calculated sample size of 70 in each group for the primary outcome based on an α value of 0.05 and power of 0.8. Considering a 20% potential drop-out rate, we enrolled 85 patients in each group for a total of 170 participants.
For continuous variables, data distribution was first assessed for normality using the Shapiro-Wilk test. Independent two-tailed t-tests were utilized to compare the means of normally distributed continuous variables. For data not conforming to a normal distribution, the Mann-Whitney U test was used. The chi-square test was used for comparing categorical variables between the two groups. Intraclass correlation coefficients (ICCs) were calculated to assess the consistency of echocardiographic measurements, where ICC values ≥ 0.75 denoted satisfactory and excellent agreement.
A univariate logistic regression analysis was performed for each potential risk factor of post-induction hypotension including age, diabetes mellitus, total duration of anti-HTN medication, type of anti-HTN medication (telmisartan or valsartan), the interval between anti-HTN medication administration on the morning of the surgery and anesthesia induction, propofol dosage, mean BP on the morning of the surgery, initial mean BP in OR, and total duration of anesthesia induction. A multivariate logistic regression analysis, including these potential risk factors, was performed using enter method to identify the independent predictors for post-induction hypotension. The post-induction hypotension period was defined as a mean BP < 65 mmHg between the introduction of anesthetic agent and 10 min after surgical incision.
Normally distributed continuous data were presented as mean ± standard deviation. Non-normally distributed continuous data were presented as medians (Q1, Q3). For categorical variables, the numbers (n) and proportions (%) were calculated.
All statistical analyses were performed using the Statistical Package for Social Sciences 22® (IBM Corp.). P values < 0.05 were considered statistically significant.
Results
In total, 282 patients were eligible for the study between April 2017 and April 2018. Among them, 112 were excluded for the following reasons: 48 were on ARBs combined with either BB or CCB, six had a history of CHF, 15 had a history of CAD, two had a history of PADO, six had a history of cerebral infarction or hemorrhage, one had a history of cardiac arrhythmia, one had a history of orthostatic hypotension, and 26 were scheduled for surgeries requiring intraoperative position change. Additionally, 13 patients were excluded from the final analysis due to poor echocardiographic views. Consequently, 157 patients were included in the final analysis (78 in the Telmisartan group and 79 in the Valsartan group) (Fig. 1).

Flow diagram for the study. ARBs: angiotensin receptor blocker, BB: beta blocker, CCB: calcium channel blockers, CHF: congestive heart failure, CAD: coronary artery disease, PAOD: peripheral artery occlusive disease, BP: blood pressure.
Both groups had similar demographic characteristics with age, gender, types of surgery, New York Heart Association class, ASA-PS, and medical history being comparable between the two groups (Table 1). There were no significant differences between the groups in terms of the total anesthetic amount used during anesthesia induction, duration of anti-HTN medication use, and the interval from taking anti-HTN medication on the morning of the surgery to anesthesia induction. Preoperative laboratory values were also similar between the two groups (Table 1).
The decline in mean BP during anesthesia induction for all patients was 27.7 ± 13.9 mmHg, with similar values for the Telmisartan and Valsartan groups (27.1 ± 15.3 mmHg vs. 28.3 ± 12.4 mmHg, respectively; P = 0.585) (Table 2). Overall, 36.3% of the patients experienced a mean BP < 65 mmHg from Initial OR to Post-incision, while 71.3% had a decline in mean BP > 20% of the morning BP from Initial OR to Post-incision. The incidence of the decline in mean BP decreasing below 65 mmHg and changes (either increase or decrease) exceeding 20% of the baseline morning BP from Initial OR to Post-incision was similar between the two groups (Table 2). There were no significant intergroup changes in mean BP during anesthesia induction between the two groups (Fig. 2A). The changes in HR during anesthesia induction were also similar between the groups (Fig. 2B), along with the use of hemodynamic agents including phenylephrine, ephedrine, or nicardipine (Table 2). During operation, the incidences of mean BP < 65 mmHg, with an increase or decrease greater than 20% of the morning BP, were also similar between the two groups. The highest intraoperative mean BP was significantly higher in the Telmisartan group than in the Valsartan groups (90.1 ± 10.6 mmHg vs. 87.1 ± 11.5 mmHg, respectively; P = 0.009). However, parameters such as lowest intraoperative mean BP, highest and lowest HR, and the incidence of phenylephrine infusion during operation, were similar between the groups (Table 2).

Comparison of Hemodynamic Profiles and Left Ventricular Ejection Fraction (LVEF) between the Telmisartan and Valsartan Groups during Anesthesia
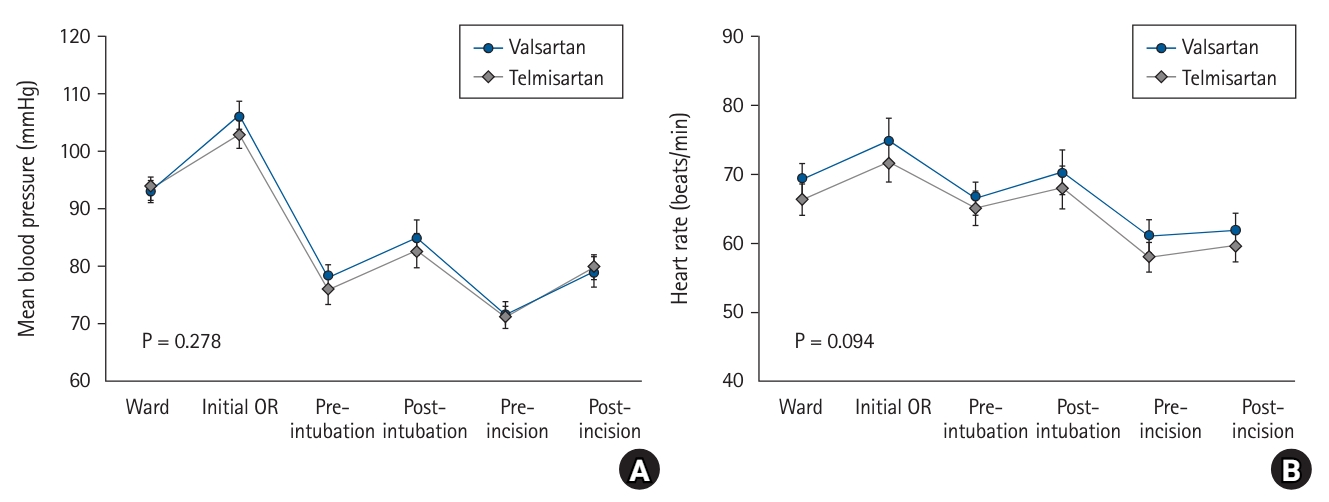
Changes in hemodynamic parameters during anesthesia induction. Changes in mean BP (A) and HR (B) in both groups are shown. BP: blood pressure, HR: heart rate, OR: operation room, Ward: on morning of operation, Initial OR: at the first time of patient hemodynamic monitors in the operation room, Pre-intubation: lowest values within 5 min before endotracheal intubation, Post-intubation: lowest values within 5 min after endotracheal intubation, Pre-incision: within 10 min before surgical incision, Post-incision: within 10 min after surgical incision.
The ICC for LVEF measurements at Initial OR, Pre-intubation, and Post-intubation were 0.773 (95% CI [0.702, 0.829]), 0.808 (95% CI [0.746, 0.856]), and 0.789 (95% CI [0.722, 0.841]), respectively. Regarding TDI values including s, e’, and a’, the lowest coefficient was 0.864, signifying excellent agreement. LVEF during anesthesia induction decreased after anesthetic administration, but increased after intubation, with no significant intergroup differences between the Telmisartan and Valsartan groups (Table 3). The TDI values (s, e’, and a’) during anesthesia induction were also comparable between the groups (Table 3).
Multivariate logistic regression analysis identified age and the mean BP at initial OR as independent predictors for a mean BP < 65 mmHg from Initial OR to Post-incision (OR [95% CI]; 1.06 [1.01, 1.11] and 0.94 [0.90, 0.97]; P = 0.020 and P = 0.001, respectively) (Fig. 3) (Supplementary Table 1).
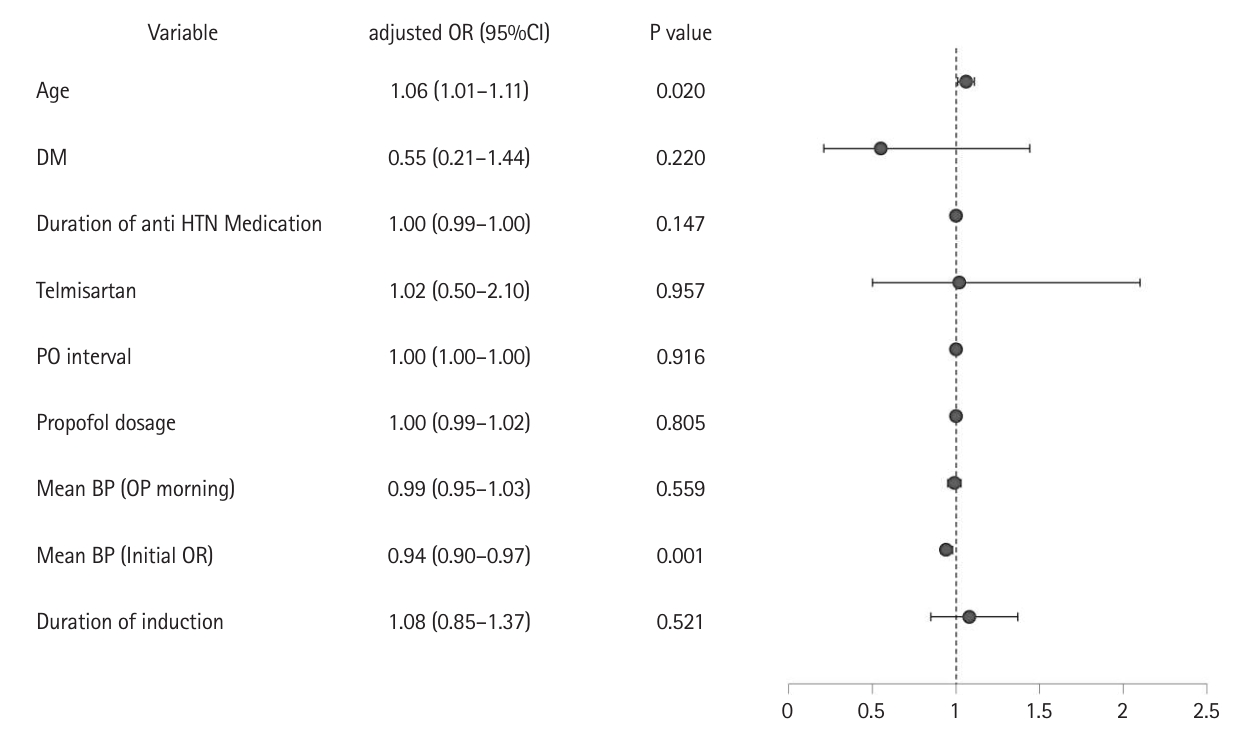
Multivariate logistic regression analysis for post-induction hypotension. DM: diabetes mellitus, HTN: hypertension, PO: per oral, BP: blood pressure, OP: operation, OR: operation room, Telmisartan: use of telmisartan as anti-HTN medication (reference value: use of valsartan), PO interval: the interval between taking anti-HTN medication on the morning of the operation and anesthesia induction, OP morning: on the morning of the operation, Initial OR: at the first time of patient hemodynamic monitors in the operation room, Duration of induction: total duration of anesthesia induction, OR: odds ratio.
Discussion
The present study demonstrated that telmisartan and valsartan had comparable effects on the decline in mean BP during anesthesia induction. There were no significant differences in the LVEF and longitudinal contraction of LV between the two groups during anesthesia induction. The highest and lowest intraoperative hemodynamic values were also comparable between the two groups. These results suggest the type of ARB administered on the morning of the surgery does not influence the hemodynamic changes during anesthesia induction.
Previous clinical studies comparing the effects of telmisartan and valsartan on HTN management [4,11–13] have demonstrated the superiority of telmisartan in controlling BP. This is because of the high protein-binding affinity [8] and pronounced norepinephrine suppression [6] of telmisartan compared to valsartan. However, telmisartan may lead to a decline in BP, potentially causing post-induction hypotension after anesthetic administration. Therefore, we anticipated a greater decline in mean BP in the Telmisartan group compared to the Valsartan group. However, there was no discernible difference in BP reduction during anesthesia induction between the two groups.
The similar changes in BP during anesthesia induction for the Telmisartan and Valsartan groups could be attributed to several factors. A BP fluctuation, under the influence of reduced systemic vascular resistance or cardiac contractility after anesthetic administration, sympathetic stimulation due to endotracheal intubation, and various factors, are common during anesthesia induction. However, various vasopressors or sympathetic antagonists may be administered to attenuate these fluctuations. Moreover, fluid administration during anesthesia induction may also significantly influence the hemodynamics. Under these conditions, the effects of ARBs may be overshadowed, resulting in indistinguishable post-induction hypotension. Consequently, the present study demonstrated consistent intraoperative BP fluctuations, regardless of the specific ARB used. While previous research has demonstrated that telmisartan offers a more potent BP control than valsartan, its influence could be attenuated by several clinical variables during practical application.
Chronic ARB therapy has been shown to interfere with the sympathetic nervous system functioning, while enhancing the parasympathetic activity [14]. Consequently, recent guidelines recommend discontinuation of ARBs prior to cardiac surgery for mitigating the risk of perioperative hypotension [15]. However, these recommendations remain a topic of debate, because the potential deleterious effects of ARBs on perioperative hypotension may vary with the type of surgery, i.e., cardiac or noncardiac surgery. Several recent studies have demonstrated that ARBs do not exacerbate perioperative hypotension during noncardiac surgeries, nor do they correlate with increased morbidity and mortality [16,17]. The present study showed that the incidence of mean BP < 65 mmHg was 36.3%, while that of a decline exceeding 20% of the morning BP was 71.3% in both groups. Moreover, the average reduction in mean BP during anesthesia induction was approximately 28 mmHg in both groups. These changes may be tolerable in noncardiac surgeries because the EF and longitudinal performance of LV were within the acceptable range on echocardiography, and the cardiac contractility remained relatively tolerable during anesthesia induction. Additionally, the relatively low incidence of vasopressor administration compared to previous studies suggests that clinically significant hypotension was a rare occurrence in the present study. Yoon et al. [17] recently demonstrated that the incidence of vasopressor use during anesthesia induction was 37% in patients taking ARBs that was higher than that in the present study. We hypothesized that the measured and gradual infusion of anesthetics through programmed TCI for total intravenous anesthesia may have played a role in limiting the incidences of post-induction hypotension and vasopressor use during anesthesia induction [18,19].
The present study showed that age and initial mean BP in OR were associated with post-induction hypotension. In particular, initial mean BP in OR was inversely related to post-induction hypotension that was in accordance with previous studies demonstrating that a lower pre-induction BP increased the incidence of post-induction hypotension [20,21]. Theoretically, increased sympathetic activity related to preoperative anxiety, such as white coat HTN, can be rapidly blunted by anesthetic administration. Crowther et al. [22] demonstrated in a prospective study that high preoperative BP was not associated with intraoperative hypotension or related complications. These inconsistent results highlight the need for a more comprehensive randomized control trial to validate these observations.
This study had several limitations. First, not all patients underwent invasive BP monitoring, although noninvasive BP was measured every minute for all patients. Second, the potential for heterogeneity in variables influencing intraoperative hypotension exists in the present study. Finally, patients classified as ASA-PS class III were not included. Therefore, in the future, meticulously planned, large-scale randomized trials are imperative to investigate the effects of ARBs on perioperative hypotension.
In conclusion, the ARB type did not significantly influence post-induction hypotension during general anesthesia induction. Age and initial mean BP in OR were significantly associated with post-induction hypotension in patients on ARBs.
Notes
Funding
This research was supported by Konkuk University.
Conflicts of Interest
Seong-Hyop Kim has been an editor for the Korean Journal of Anesthesiology since 2019. However, he was not involved in any process of review for this article, including peer reviewer selection, evaluation, or decision-making. There were no other potential conflicts of interest relevant to this article.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Chung-Sik Oh (Conceptualization; Data curation; Formal analysis; Writing – original draft)
Jun Young Park (Data curation; Investigation)
Seong-Hyop Kim (Supervision)
Supplementary Material
Univariate analysis and multivariate logistic regression analysis of variables associated with post-induction hypotension.