Comparison of the analgesic efficacy of the ultrasound-guided transversalis fascia plane block and erector spinae plane block in patients undergoing open inguinal hernia repair under spinal anesthesia
Article information
Abstract
Background
Open inguinal hernia repair (OIHR) surgery is a common surgical procedure, and ultrasound guided interfascial plane blocks can also be included in current approaches to postoperative multimodal analgesia regimens. This study aimed to compare the postoperative analgesic efficacy of the erector spinae plane block (ESPB) and transversalis fascia plane block (TFPB) in patients undergoing OIHR.
Methods
This prospective, randomized, assessor-blinded comparative study was conducted in the postoperative recovery room and ward of a tertiary hospital. A total of 80 patients with American Society of Anesthesiologists physical status I–III were enrolled and allocated equally to either the ESPB or TFPB group. The patients received standard multimodal analgesia in addition to an ultrasound-guided ESPB or TFPB. During the first 24 h postoperatively, tramadol consumption was assessed and pain levels at rest and during movement were compared using numeric rating scale (NRS) scores at 1, 3, 6, 9, 12, 18, and 24 h postoperatively.
Results
The results showed no difference in NRS scores at any time point between the groups, except for NRS at rest in the third hour. However, tramadol consumption was lower in the TFPB group than in the ESPB group overall (88 ± 75.2 vs. 131 ± 93.7 mg, respectively; P = 0.027, mean difference: −43, 95% CI [−80.82, −5.18]).
Conclusions
The TFPB leads to lower tramadol requirements in the first 24 h postoperatively than the ESPB in patients undergoing OIHR.
Introduction
Regional anesthesia techniques, particularly with the development and incorporation of ultrasonography technology into anesthesia practice, have become popular and widely used by anesthesiologists over the past few decades, both as effective anesthesia techniques and as essential components of multimodal analgesia [1–3].
Approximately 20 million open or laparoscopic inguinal hernia repairs are performed annually, making it one of the most common operations conducted in general surgery [4]. Effective pain management is crucial for both types of surgeries, though patients undergoing open inguinal hernia repair (OIHR) often experience nociceptive pain initially and can potentially develop moderate to severe long-term chronic pain due to factors such as nerve damage. Some studies report an incidence of chronic pain up to 20% within 1–5 years of OIHR performed using a Liechtenstein incision [5]. While some publications suggest that incorporating regional anesthesia techniques into conventional analgesic approaches can mitigate chronic postoperative pain, evidence supporting this claim remains limited [5,6].
Opioids, non-steroidal anti-inflammatory drugs, and other analgesics are conventionally recommended to manage postoperative pain post-OIHR. However, procedure-specific pain management (PROSPECT) guidelines recommend a multimodal analgesic approach for postoperative pain management, including regional nerve techniques such as infiltrative analgesia, ilioinguinal/iliohypogastric (II-IH) nerve block, and transversus abdominis plane block [7,8].
In OIHR surgery, the subcostal nerve (T12), ilioinguinal nerve (L1), iliohypogastric nerve (T12-L1), and sometimes the genitofemoral nerve (L1-L2) provide sensory innervation to the incision area [9–11]. According to the literature, II-IH and transversus abdominis plane (TAP) blocks are used most frequently to treat postoperative pain following OIHR surgery [12]. To provide a wider sensory block to the inguinal region, some clinicians have chosen to apply blocks more proximal than the TAP and II-IH blocks. While the transversalis fascia plane block (TFPB) inhibits both the lateral cutaneous branches of the IH and subcostal nerves, it also inhibits sensory transmission to the T12-L1 dermatomes. This technique, originally only used for analgesia in iliac crest harvesting, has since been applied in a variety of surgeries including inguinal hernia repair, cesarean section, and varicocelectomy [13–15]. Numerous studies have also been conducted on the quadratus lumborum block and erector spinae plane block (ESPB), among others, which have become increasingly popular for adult and pediatric lower abdominal surgery [16–18].
The ultrasound-guided TFPB is a regional anesthesia technique defined by Hebbard that targets the T12-L1 dermatomes [19]. Similar to the techniques mentioned above, the TFPB has been used for inguinal region and lower abdominal surgeries owing to the target region of the block, and has been the subject of various clinical studies [20,21]. Although both the TFPB and ESPB have been found to reduce postoperative analgesic consumption in OIHR, no study has compared analgesic consumption between these two techniques in inguinal hernia repair surgery.
We hypothesized that these two techniques, which provide sensory block in similar anatomical regions, would show comparable reduction in analgesic requirements. This randomized controlled trial aimed to compare the effects of ESPB and TFPB on the analgesic requirement in the first 24 h after unilateral OIHR surgery. A secondary aim was to compare the pain scores between the two techniques within the same timeframe.
Materials and Methods
Study design
The design of this study was randomized, prospective, comparative, and assessor-blinded. The principles outlined in the Declaration of Helsinki, 2013 were adhered to throughout this research project, which was conducted at a tertiary hospital between May 2022 and November 2022. This study was approved by the local ethics committee (No. OMU-KAEK 2021/558) and the Medicines and Medical Devices Agency (No. 22-AKD-05) of the Turkish Ministry of Health and registered at ClinicalTrials.gov (No. NCT05344105).
This study included patients aged 18–65 years with an American Society of Anesthesiologists (ASA) physical status I–III scheduled to undergo elective unilateral open inguinal hernia surgery under spinal anesthesia. Patients with a body mass index (BMI) > 35 kg/m2, coagulopathy, local infection or hematoma in the block target area, an allergy to local anesthetic (LA) agents or one of the drugs used in the study, history of chronic opioid and corticosteroid use as well as those who refused to participate, were unable to use the controlled analgesia system, had a psychiatric disorder, or were taking drugs that could affect the perception of pain, such as gabapentin/pregabalin, were excluded from the study. To further standardize the study, patients with surgical times < 30 min or > 180 min were excluded.
Randomization and blinding
While being transferred to the postoperative care unit (PACU), the patients were randomly allocated to the TFPB and ESPB groups by the anesthesia assistant using sequentially numbered opaque envelopes (n = 40 per group).
The healthcare professional responsible for randomization, who was not involved in patient evaluation, was the sole participant in this step. Each patient was assigned a randomized identification number that was used for all data collection and evaluation processes. Microsoft Excel 2010 was used to create the randomization ID numbers. The anesthesiologist responsible for data collection was blinded to the study group. A separate specialist who was not involved in data collection or analysis performed each block.
Anesthesia admnistration procedure
All patients received anesthesia and perioperative analgesia according to the same protocol. Intraoperative monitoring included electrocardiography, non-invasive blood pressure monitoring, and peripheral oxygen saturation measurements. To provide surgical anesthesia, a 26-gauge (G) spinal needle was inserted from the midline at the L3–L4/L4–L5 level and spinal anesthesia, consisting of 2.5–3 ml of 0.5% heavy bupivacaine, was administered to all patients in the seated position. No adjunctive medication was added to the spinal anesthesia. Patients were subjected to a pinprick test after spinal anesthesia, and surgery was started after sensory block at the T10 level was achieved. The surgical team did not administer infiltrative analgesia to the surgical site. Twenty minutes before the end of surgery, 1 g paracetamol and 50 mg dexketoprofen were administered to all patients as part of the perioperative analgesia plan.
Block administration
All blocks were performed in a sterile environment at the end of the surgery in the block performance room. Each block was performed unilaterally using a low-frequency ultrasound device (3–5 MHz, Esoate MyLabTM30Gold) at the same LA volume and concentration (30 ml of 0.25% bupivacaine).
TFPB application
Sonographic imaging was performed in the supine or lateral position when the supine image was insufficient. To identify the skin, subcutaneous tissue, external oblique muscle, internal oblique muscle, transversus abdominis muscle, deep fascia of the transversus abdominis muscle, retroperitoneal adipose tissue, peritoneum, and quadratus lumborum muscle, the transducer was placed such that it rested on the iliac crest in the transverse plane and was angled slightly caudally. A 21-G 100-mm needle (SonoPlex STIM, Pajunk) was advanced just as deep as the lateral end of the transversus abdominis muscle using the out-of-plane technique, and 30 ml of LA was injected.
ESPB application
With the patient in the lateral decubitus position, the transducer was placed 2–3 cm lateral to the spinous process of the T12 vertebra, and the erector spinae muscle and transverse process were visualized. Using the out-of-plane technique, the tip of the 21-G 100-mm needle was advanced in the interfacial plane deep to the erector spinae muscle, and 30 ml of LA was injected.
Standard postoperative analgesia protocol and pain evaluation process
All patients underwent identical analgesic protocols. After surgery, 1 g of paracetamol and 50 mg of dexketoprofen were administered intravenously at 8- and 12-h intervals, respectively. Tramadol-based patient-controlled analgesia (PCA), prepared at a concentration of 4 mg/ml in a total volume of 100 ml, was also administered. The bolus dose was adjusted to 10 mg and the lockout time was set to 20 min, with no basal infusion. In the recovery room, the PCA was initiated immediately after the block was performed, and the patient was instructed to request analgesia if the numeric rating scale (NRS) score was > 4. If the NRS score remained > 4 despite the use of PCA in the first 24 h, 25 mg of intravenous meperidine was planned as a rescue analgesic. The total amount of tramadol consumed was recorded at 1, 3, 6, 9, 12, 18, and 24 h postoperatively.
The NRS was used to assess pain at 1, 3, 6, 9, 12, 18, and 24 h postoperatively at rest and while coughing. The NRS is a one-dimensional scale that can be used to assess pain intensity in adults. It is a segmented numerical version of the visual analog scale and involves choosing an integer (ranging from 0 to 10) that most accurately reflects the current level of pain, where 0 represents no pain and 10 represents the most excruciating pain imaginable.
Outcome measurements
The primary outcome was opioid (tramadol) consumption within the first 24 h. The NRS scores obtained while at rest (NRS-rest) and while coughing (NRS-dynamic) served as secondary outcome measures. Six hours after surgery, symptoms such as nausea, vomiting, time to first analgesia request, and quadriceps muscle weakness were noted. Quadriceps muscle weakness was assessed as follows: with the hip joint at 45° and the knee joint at 90° of flexion, the patient was instructed to extend the knee joint first against gravity and then against applied resistance. The patient’s ability to extend the knees was assessed using a 3-point scale (0 = normal strength [the knee can be extended to full extension both against gravity and applied force], 1 = paresis [the knee can be extended against gravity but not against applied resistance], and 2 = paralysis [the knee cannot be extended]). Scores of 1 and 2 were considered to reflect quadriceps weakness.
Sample size and statistical analyses
In our pilot study involving 10 patients, we observed that the 24-h tramadol consumption in the TFPB group was 108 ± 41.47 mg. To detect a statistically significant 30% reduction in tramadol consumption with an alpha level of 0.05 and a beta level of 0.10, we calculated that a minimum of 35 participants per group would be required. To account for potential dropouts, we included a minimum of 40 patients in each group, which represented a 15% increase in the sample size.
The Statistical Package for Social Sciences (SPSS Statistics for Windows, version 22.0; IBM Corp.) was used for statistical analyses. The Kolmogorov-Smirnov test was used to determine data normality. Descriptive data are presented as mean and standard deviation (SD), mean difference (MD) and 95% CI, or median (Q1, Q3). Continuous variables with equal variances were assessed using the t-test, whereas non-normally distributed data were analyzed using the Mann-Whitney U test. Categorical variables were evaluated using the chi-square or Fisher’s exact test. The time to first analgesia requirement was analyzed using the t-test and Kaplan-Meier analysis. The threshold for statistical significance was set at P < 0.05. The Bonferroni correction was used to analyze NRS scores, with statistical significance adjusted to P < 0.0071 owing to measurements from seven time points.
Results
Eighty-four patients agreed to participate in the study, four of which were excluded: two for inadequate/failed spinal block and two for PCA device failure. Therefore, 40 patients per group were included in the study. The CONSORT flow diagram for this study is shown in Fig. 1.
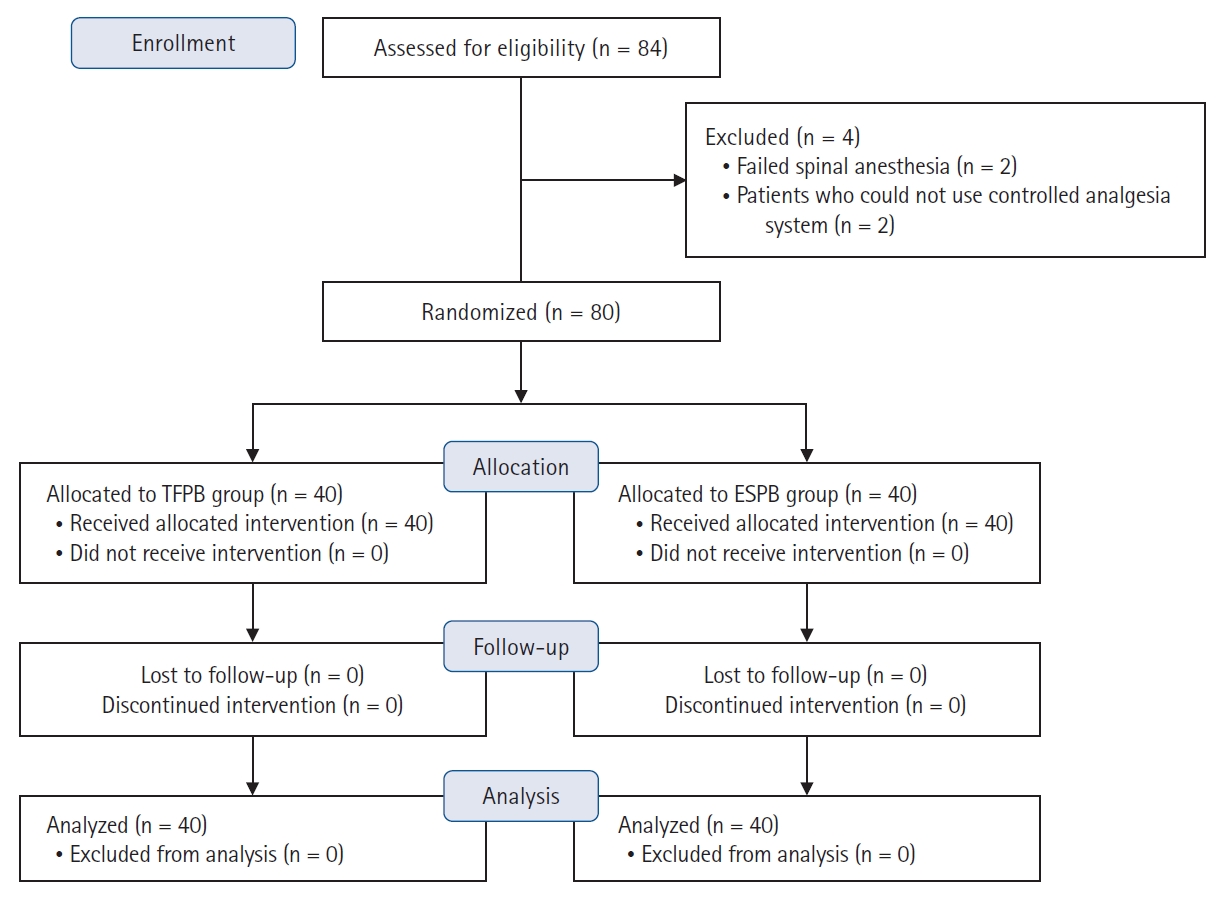
Consolidated Standards of Reporting Trials (CONSORT) diagram of the study. TFPB: transversalis fascia plane block, ESPB: erector spinae plane block.
Males comprised the majority of patients in both groups (TFPB group: 38/40 and ESPB group: 35/40). The ASA classification; average age, height, weight, and BMI of the patients; and surgical times were similar between the groups, as shown in Table 1 (P > 0.05).

Comparison of Age, Gender, ASA Classification, Height, Weight, Body Mass Index, Surgical Time, and Time to First Analgesia Requirement between the TFPB and ESPB Groups
When the mean 24-h tramadol requirements of the groups were compared, the TFPB group was found to have a lower tramadol requirement than the ESPB group, with a statistically significant difference (88 ± 75.2 vs. 131 ± 93.7 mg, MD: −43, 95% CI [−80.82, −5.18], P = 0.027).
As shown in Table 2 and Fig. 2, the cumulative amount of tramadol consumed in the TFPB group was significantly lower than that consumed in the ESPB group at all time points, with the exception of the first hour. In addition, when we used time intervals rather than time points of cumulative tramadol and repeated the comparisons, the use of tramadol for hours 1–3 was statistically significantly lower in the TFPB group than in the ESPB group (10.5 ± 20.24 vs. 24.5 ± 31.86 mg, MD: −14, 95% CI [25.88, −2.12], P = 0.018). No significant differences in the amount of tramadol required was found between hours 3–6, 6–9, 9–12, 12–18, or 18–24 (P > 0.05). Fig. 2 shows a comparison of tramadol consumption between the groups at different time intervals. Meperidine was not required for any patient in either group.

Comparison of Cumulative Tramadol Consumption at Different Time Points between the TFPB and ESPB Groups

Box plot comparison of tramadol consumption at different time frames between groups. The x axis shows tramadol consumption at different time frames for each group and the y axis shows the tramadol consumption during the time frames (*Statistically significant difference). TFPB: transversalis fascia plane block, ESPB: erector spinae plane block.
Compared to patients in the ESPB group, a significantly higher rate of patients in the TFPB group required no additional analgesia (7.5% vs. 25%, P = 0.033). The time to first analgesia requirement was longer in the TFPB group than in the ESPB group, although the difference was not significant (264.8 ± 140.1 vs. 209.2 ± 110.6 min, MD: 55.6, 95% CI [−0.59, 111.79], P = 0.053) (Table 1). Fig. 3 shows a Kaplan-Meier graph of the time to first analgesic requirement according to group. The median values along with the (Q1, Q3) were as follows: 317.5 min (Q1, Q3; 152.5, 1227.5) for the TFPB group and 180 min (Q1, Q3; 120, 330) for the ESPB group. The log-rank test revealed a noteworthy distinction between the two groups, favoring the TFPB group in terms of both time to first analgesic requirement and analgesic consumption (P = 0.006).

Kaplan Meier curve for TFPB and ESP groups with confidence intervals. The x axis shows the time in minutes and y axis shows the percentage of patients not requiring tramadol. TFPB: transversalis fascia plane block, ESPB: erector spinae plane block.
At rest, the NRS scores were similar between the groups at all time points except at hour 3, as shown in Table 3. Dynamic NRS scores were similar across all time points and between groups. Only one patient in the ESPB group experienced quadriceps weakness for up to 9 h after surgery; the other patients experienced no motor weakness at or after 6 h.
Discussion
In our study, patients in the TFPB group who underwent unilateral OIHR surgery under spinal anesthesia required significantly less tramadol for postoperative analgesia than those in the ESPB group. The NRS scores were comparable across most timeframes. Since the scheduled analgesia was adequate in the TFPB group, the proportion of patients who did not request an additional PCA rescue dose in the first 24 h was 25%, whereas it was 7% in the ESPB group. This difference was statistically significant.
As mentioned, available studies for both techniques included in this study are limited. In OIHR, the TFPB has only been used in a few studies. Lopez-Gonzalez et al. [22] conducted a retrospective observational study in which 30 ml of 0.25% levobupivacaine was administered through the TFPB and anterior TAP block at the conclusion of unilateral OIHR surgery performed under general anesthesia and found comparable postoperative analgesic outcomes for both techniques. Fouad et al. [15] compared the postoperative analgesic effects of the TFPB and anterior quadratus lumborum block and found both to be effective and comparable in inguinal hernia surgery. One controlled study examined the postoperative analgesic effect of a preemptive TFPB in patients undergoing OIHR and concluded that it reduces both postoperative analgesic requirements and pain intensity following pediatric inguinal herniorrhaphy [23].
The ESPB, introduced by Forero in 2016 [24], involves administering LA in the interfacial plane between the transverse process of the vertebrae and the erector spinae muscle group with the goal of blocking both the dorsal and ventral rami. The ESPB can be adapted to various spinal levels, potentially producing paravertebral block-like effects [24,25], and has been used for postoperative pain management as part of multimodal analgesia for nearly all types of operations (except for distal extremities and cephalic operations) with positive results [25,26].
Previous studies have shown the efficacy of ESPB after OIHR surgery in both adult and pediatric patients [27,28]. El-Emam and El Motlb [27] administered ESPB to children at a volume of 0.5 ml/kg from the L1 transverse process and found a lower rescue analgesic requirement, lower FLACC scores, and a longer time to first analgesic request compared to the II-IH block in OIHR. Sakae et al. [28] performed ESPB at T8 level with 20 ml ropivacaine (0.5%) LA, determined that it did not reduce the rescue analgesic requirement, and reported that it was ineffective for OIHR. Given the volume and concentration of ESPB used in that study [28], we did not expect it to be effective for OIHR.
In our study, we observed that TFPB outperformed ESPB in terms of the postoperative analgesic requirement in patients undergoing OIHR under spinal anesthesia, whereas the effects on pain scores and first analgesic requirement were comparable. Despite differences in the clinical study methodology, tramadol requirements in both groups were comparable or lower than those in regional anesthesia studies in the same patient group [29,30]. The TFPB group required 33% less tramadol than the ESPB group; however, this difference may not be clinically significant. To date, no minimum clinically important difference (MCID) studies have been conducted for OIHR, and no data have been provided regarding the threshold at which change in opioid requirements or NRS scores would be significant. As a result, we could not make any definitive statements regarding the clinical significance of this statistical difference between the groups. However, asserting the clinical significance of this difference, which is equivalent to an oral morphine dose of approximately 13 mg, may not be reasonable given the currently available literature (generally, a reduction ≥ 30 mg or > 40% is considered significant). For a stronger claim, the MCID for OIHR surgery should be calculated along with the concept-specific MCID, which is already recommended for similar types of surgeries [31,32].
As mentioned, ESPB is a popular, easy, and safe technique that is frequently used for both acute and chronic pain, and successful applications for perioperative analgesia have been reported for both open and laparoscopic inguinal hernia surgeries. The possible mechanism of action is explained as the transition of LA to the paravertebral area when applied to the posterior of the transverse process. However, clinical, cadaveric, and radiological studies have shown that for many interfacial plane blocks, this same distribution is not always observed [33,34]. Although the ESPB sometimes results in limited sensory block in the paraspinal region, it also sometimes works as a multilevel paravertebral block [35,36]. Conversely, the TFPB application point is very close to the nerve tissue and is a more target-specific block. The differences in tramadol requirements between the groups may have resulted from these anatomical differences. When we reanalyzed tramadol consumption using time intervals instead of cumulative tramadol consumption, we determined that the statistical difference was found in the 1–3 h interval and the main difference in the subsequent measurements was due to the difference at this interval. Although the LA is applied directly adjacent to the nerve in TFPB, it is applied far from these neuronal structures in ESPB and reaches the target via leakage from the fascial planes. This may also help explain the difference determined clinically earlier.
Performance-oriented characteristics, such as ease of sonoanatomical visualization and identification, necessity of positioning, and block onset time, are also important, as well as whether the technique used in regional anesthesia is effective as an analgesic. In our study, we placed all patients undergoing ESPB in the lateral decubitus position, which increased the time required to perform the block. However, we were able to perform this technique in the supine position in 37 of the 40 patients who received the TFPB. This not only saves practitioner time but also eliminates the need for an additional healthcare professional to maintain the patient under spinal anesthesia in the lateral position. The block performance time for the TFPB was significantly shorter and the effort required was lower. However, this was not documented in detail as it was not one of our outcomes.
Ten patients in the TFPB group and three patients in the ESPB group did not require any tramadol from their PCA devices, with a statistically significant difference.
Quadriceps weakness was a secondary outcome of our study. We found quadriceps weakness in one patient in the ESPB group when the groups were assessed at 6 h after the block, which persisted until 9 h postoperatively. At 6 h postoperatively, no quadriceps weakness was found in the TFPB group. Transient quadriceps weakness has been reported anecdotally in the literature after the administration of a TFPB or ESPB at or below the T11 level, though it usually resolves within 24 h [37,38]. As with all regional anesthesia techniques, complications such as intravascular injection, systemic anesthetic toxicity, and injury to adjacent tissues can be observed. Practitioners must be aware of this complication and potential side effects of LA spread.
This study also had some limitations. The first limitation was that neither cutaneous blockage mapping nor dermatomal sensory analysis were conducted after regional anesthesia. We chose not to perform these measurements because the patients included in the study underwent surgery under spinal anesthesia and because doing so might have been confusing in the event of prolonged spinal anesthesia. A recent Delphi consensus advised that block characteristics such as sensory testing of the block and block duration should be noted and reported [39]. Compared with peripheral nerve block studies, determining the duration of facial plane blocks is significantly more difficult. Instead, we assessed the time to first analgesic request, which was ≥ 3.5 h for both block groups. The Delphi consensus study also suggests recording and reporting patient satisfaction. Although we conducted patient satisfaction surveys, such as the QoR-15, and almost all our patients provided positive feedback, the fact that this was not documented is a significant limitation. As our work was planned prior to the release of this Delphi consensus, we were unable to follow these and similar recommendations, but we recommend that those who work on regional anesthesia in the future consider the consensus recommendations.
Although the lack of a control group can be considered a limitation, our research was defined and conducted as a comparative study, as previous controlled/observational studies have demonstrated the effectiveness of both blocks. In studies investigating the postoperative analgesic efficacy of facial plane blocks, patients may undergo surgery under general or spinal anesthesia [40]. In our clinic, spinal anesthesia is often preferred as the main method of administration in patients with OIHR. Considering our clinical practice, we believe that it would be more appropriate to add a facial block after spinal anesthesia, rather than administering spinal anesthesia alone. Another limitation is that we did not evaluate and note the duration of spinal anesthesia in some timeframes. Unfortunately, this concern is common in similar studies investigating the effectiveness of interfacial plane blocks performed at the end of surgeries performed under spinal anesthesia. Features such as the type and volume of LA in the spinal anesthesia, and the duration of surgery were kept similar, and all blocks were performed at the end of surgery, thus minimizing the effects of spinal anesthesia duration on pain and analgesic consumption. A non-inferiority/superiority or equivalence trial may have been more appropriate. However, because of the absence of an established gold standard for both the ESPB and TFPB techniques and the lack of prior comparative studies, this particular methodology was not employed.
In the absence of spinal morphine, our study revealed that patients who underwent unilateral OIHR under spinal anesthesia experienced a lower cumulative analgesic requirement during the 24-h postoperative period when ultrasound-guided TFPB was added as part of the multimodal analgesia than when ESPB was added.
Acknowledgements
We would like to thank Naci Murat from the Ondokuz Mayis University Faculty of Engineering/Industrial engineering for his contributions to the statistical evaluation of this study.
Notes
Funding
This study was funded by the Interventional Clinical Research Ethics Committee of Samsun Research and Education Hospital (No. EHK/2022-97).
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Hale Kefeli Çelik (Conceptualization; Data curation; Funding acquisition; Methodology; Writing – original draft; Writing – review & editing)
Serkan Tulgar (Conceptualization; Data curation; Methodology; Supervision; Writing – original draft; Writing – review & editing)
Ömer Faruk Bük (Data curation; Investigation; Writing – review & editing)
Kadem Koç (Data curation; Methodology; Writing – review & editing)
Murat Ünal (Data curation; Investigation; Writing – review & editing)
Caner Genç (Data curation; Investigation; Writing – review & editing)
Mustafa Süren (Conceptualization; Methodology; Supervision; Writing – review & editing)

