Effect of magnesium sulfate on oxygenation and lung mechanics in morbidly obese patients undergoing bariatric surgery: a prospective double-blind randomized clinical trial
Article information
Abstract
Background
Respiratory mechanics are often significantly altered in morbidly obese patients and magnesium sulfate (MgSO4) is a promising agent for managing several respiratory disorders. This study aimed to examine the effects of MgSO4 infusions on arterial oxygenation and lung mechanics in patients with morbid obesity undergoing laparoscopic bariatric surgery.
Methods
Forty patients with morbid obesity aged 21–60 years scheduled for laparoscopic bariatric surgery under general anesthesia were randomly allocated to either the control (normal saline infusion) or MgSO4 group (30 mg/kg lean body weight [LBW] of 10% MgSO4 in 100 ml normal saline intravenously over 30 min as a loading dose, followed by 10 mg/kg LBW/h for 90 min). The primary outcome was intraoperative arterial oxygenation (Δ PaO2/FiO2). Secondary outcomes included intraoperative static and dynamic compliance, dead space, and hemodynamic parameters.
Results
At 90 min intraoperatively, the Δ PaO2/FiO2 ratio and the Δ dynamic lung compliance were statistically significantly higher in the MgSO4 group (mean ± SE: 16.1 ± 1.0, 95% CI [14.1, 18.1] and 8.4 ± 0.5 ml/cmH2O, 95% CI [7.4, 9.4]), respectively), and the Δ dead space (%) was statistically significantly lower in the MgSO4 group (mean ± SE: −8.0 ± 0.3%, 95% CI [−8.6, −7.4], P < 0.001). No significant differences in static compliance were observed.
Conclusions
Although MgSO4 significantly preserved arterial oxygenation and maintained dynamic lung compliance and dead space in patients with morbid obesity, the clinical relevance is minimal. This study failed to adequately reflect the clinical importance of these results.
Introduction
Bariatric surgery is considered the most effective treatment for patients with morbid obesity as it results in weight loss and has a clear impact on obesity-related comorbidities [1].
Morbid obesity is commonly associated with a higher incidence of restrictive lung diseases [2]. Obese patients often exhibit significant alterations in respiratory mechanics, which can be further aggravated by general anesthesia, such as decreased expiratory reserve volume (ERV) and functional residual capacity (FRC). In addition to atelectasis, insufficient oxygenation, reduced chest and lung compliance, increased lung resistance, and increased work of breathing have been reported [3,4].
Additionally, morbid obesity is often associated with respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD). A meta-analysis of more than 300,000 adult patients found a direct relationship between obesity and asthma, suggesting that as the body mass index (BMI) increases, the risk of asthma increases [5]. The mechanisms underlying this relationship may include the mechanical consequences of long-term lung compression, exaggerated local and systemic inflammation, and abnormal immunological responses, which are usually altered in obesity [6]. Moreover, obesity is more prevalent among patients with COPD than in the general population [7]. Hence, obese patients are more prone to postoperative acute respiratory failure [8] and have a higher incidence of pneumonia, prolonged periods of mechanical ventilation, and weaning difficulty [9–14].
Magnesium sulfate (MgSO4) is a promising agent with favorable effects in the management of various respiratory disorders such as asthma, COPD, and pulmonary hypertension. Endogenous magnesium plays a crucial role in sustaining appropriate lung function and reducing airway reactivity [15,16]. Magnesium helps smooth muscle relaxation by blocking calcium release [17]. It also acts through various mechanisms such as T cell stabilization, prevention of mast cell degranulation, inhibition of acetylcholine release, and stimulation of nitric oxide and prostacyclin synthesis, thereby reducing airflow obstruction [17]. Several studies have reported magnesium deficiency in patients with asthma [18]. Furthermore, low serum magnesium levels are associated with COPD exacerbation [19].
A recent study found promising results regarding arterial oxygenation and lung mechanics with the administration of intraoperative magnesium in patients with COPD [20]. We hypothesized that magnesium supplementation could improve perioperative oxygenation and lung mechanics parameters in morbidly obese patients undergoing bariatric surgery. Therefore, this study aimed to examine the effects of intraoperative MgSO4 administration on arterial oxygenation and lung mechanics in morbidly obese patients undergoing bariatric surgery.
Materials and Methods
This double-blind, randomized clinical trial was approved by the Research Ethical Committee of the Faculty of Medicine, Ain Shams University (Approval number: FMASU R07/2021), and registered at ClinicalTrials.gov (NCT04769440). This study was also conducted in accordance with the ethical principles of the Helsinki Declaration 2013. A total of 40 patients aged 21–60 years with a BMI > 40 kg/m2 and restrictive lung disease diagnosed by pulmonary function tests (forced vital capacity [FVC] < 70%) were enrolled. The included patients were scheduled for laparoscopic bariatric surgery < 3 h under general anesthesia and had no previous history of abdominal surgery.
The exclusion criteria were as follows: refusal to participate in the study; American Society of Anesthesiologists (ASA) physical status score > II; history of organ failure (e.g., cardiac, hepatic, or renal), arrhythmias, or combined restrictive-obstructive pulmonary disease; or use of antiarrhythmic drugs, beta-blockers, or calcium channel blockers. Patients with any of the following were also excluded from the study: forced expiratory volume in the first second (FEV1)/FVC < 70%, pregnancy or lactation, a history of allergies to the study drugs, and operation time > 3 h.
This study was conducted at hospitals affiliated with Ain Shams University between March 2021 and February 2022. After all patients who met the inclusion criteria provided informed consent, they were randomly assigned to either the MgSO4 group or the control group at a 1 : 1 ratio using a computer-generated table of random numbers sealed in opaque envelopes. The envelopes were opened immediately before drug administration. Fifteen minutes after endotracheal intubation, the patients in the MgSO4 group (n = 20) received an intravenous infusion of 10% MgSO4 in 100 ml normal saline at 30 mg/kg lean body weight (LBW) over 30 min as a loading dose, followed by 10 mg/kg LBW/h for 90 min. Patients in the control group (n = 20) received an intravenous infusion of 100 ml of normal saline for 30 min, followed by a saline infusion at the same rate as the study group for 90 min. The study drugs were prepared by hospital pharmacists. Moreover, a blinded anesthetist who did not participate in the study performed patient follow-up.
Preoperatively, each patient’s medical history and demographic data (i.e., age, BMI, and ASA physical status score) were recorded, and a thorough physical examination was performed, including complete blood count, prothrombin time, activated partial thromboplastin time, liver and kidney function tests, serum magnesium levels, pulmonary function tests, and arterial blood gases. Patients were instructed to fast for 8 h before the operation.
Upon arrival in the operating room, an intravenous cannula was inserted. The patient was premedicated with ranitidine (50 mg) and metoclopramide (10 mg). Standard monitoring via noninvasive blood pressure (NIBP), electrocardiography (ECG), and pulse oximetry was conducted for all patients, and capnography was performed after intubation. Baseline readings of the mean arterial pressure (MAP), heart rate (HR), and oxygen saturation (SpO2) were also recorded.
LBW was used to calculate the doses of all drugs except neostigmine, for which total body weight was used. LBW was calculated using the James equation as follows: (1.10 × weight) – (128 [weight/height]2) for men and (1.07 × weight) – (148 [weight/height]2) for women [21].
Preoxygenation was performed for 5 min. Anesthesia was induced by slowly administering intravenous fentanyl (2 µg/kg LBW) and propofol (1.5–2 mg/kg LBW) until loss of response to verbal commands. Intravenous atracurium (0.5 mg/kg LBW) was administered to facilitate tracheal intubation. Anesthesia was maintained with 1.0%–1.5% isoflurane in oxygen at a fraction of inspired oxygen (FiO2) of 0.4. In the event that the SpO2 dropped below 95%, the FiO2 was increased gradually by 0.1. The neuromuscular block was maintained with incremental doses of atracurium (0.01 mg/kg LBW) every 30 min, guided by peripheral nerve stimulator monitoring while maintaining a train-of-four (TOF) count at 1/4. All the measurements were performed using a TOF count of 1/4.
All the patients were mechanically ventilated. We adopted a volume-controlled mode of ventilation, maintaining a low tidal volume of 6–8 ml/kg LBW, and positive end-expiratory pressure (PEEP) ranging from 8 to 10 cmH2O. End-tidal CO2 was maintained between 30 and 35 mmHg by adjusting the respiratory rate.
The patients were placed in the reverse Trendelenburg position and the abdomen was insufflated with CO2, maintaining an intra-abdominal pressure between 14 and 15 mmHg. Ringer’s acetate was administered during the operation, and the total volume of consumed fluids was calculated. All the surgical procedures were performed by the same team. Intravenous paracetamol (2 g) and ketorolac (40 mg) were administered at the end of surgery. The surgeon then carefully evacuated the CO2 from the abdomen, and the isoflurane treatment was discontinued. Muscle relaxation was reversed prior to extubation. Once the TOF count reached 2/4, neostigmine 0.05 mg/kg and atropine 0.02 mg/kg LBW were administered to counteract the remaining muscle relaxant effect. Once the patients were able to follow verbal commands, they were transferred to the post-anesthesia care unit (PACU), where they were closely monitored.
Outcomes
To evaluate the primary and secondary outcomes, the following variables were recorded.
Primary outcome
To assess the primary outcome of intraoperative arterial oxygenation, we evaluated the Δ PaO2/FiO2. The PaO2/FiO2 ratio was recorded 5 min after endotracheal intubation (baseline) and 90 min after the drug infusion was initiated. The Δ PaO2/FiO2 ratio was calculated by subtracting the PaO2/FiO2 ratio at baseline from the PaO2/FiO2 ratio 90 min after initiating the drug infusion.
Secondary outcomes
To evaluate the secondary outcomes, static and dynamic lung compliance, dead space, and hemodynamic parameters were assessed. Static lung compliance was calculated as: tidal volume/(plateau pressure – PEEP). Dynamic lung compliance was calculated as: tidal volume / (peak airway pressure – PEEP). Physiological dead space was calculated as Vd/Vt = 1.14 (PaCO2 – EtCO2)/(PaCO2 – 0.005) using the Hardman and Aitkenhead equation [22]. Each was recorded 5 min after endotracheal intubation (baseline) and 90 min after initiating the drug infusion. The Δ static compliance was calculated by subtracting the static lung compliance at baseline from the static lung compliance 90 min after initiating the drug infusion. The Δ dynamic compliance was calculated by subtracting the dynamic lung compliance at baseline from the dynamic lung compliance 90 min after initiating the drug infusion. Finally, the Δ dead space (%) was calculated as follows: dead space 90 min after initiating the drug infusion – dead space at baseline/dead space at the end of the drug infusion%.
To assess hemodynamic parameters, the MAP and HR were recorded at baseline and every 15 min. In the event that the MAP dropped > 20% from baseline, vasoactive medications such as ephedrine were administered, and atropine was administered if the HR dropped to < 50 beats/min. The Ramsay sedation score was assessed upon arrival in the operating room, immediately postoperatively, and 1 h postoperatively [23]. Serum MgSO4 levels were recorded 1 h postoperatively.
The following operative data were recorded: surgical time, intraoperative fluids, blood loss, recovery time (defined as the time from the cessation of isoflurane to the patient complying with orders), and the need for postoperative intensive care unit (ICU) admission (criteria for admission were SpO2 < 88% on a 6-L oxygen mask, signs of altered consciousness [agitation or drowsiness], tachypnea, and the need for postoperative mechanical ventilation). Postoperative complications such as bleeding or leakage were also recorded. Patients were transferred to the hospital ward if the modified Aldrete score was ≥ 9.
Sample size calculation
Using the PASS 11 and setting the power to 0.80 and α to 0.05, a minimal sample size of two cases in each group was required to obtain statistically significant results between the assumed Δ PaO2/FiO2 (%) in the MgSO4 and control groups (Δ 3.1 ± 0.2 and −12.2 ± 0.5, respectively) [20]. A sample size of 40 patients (20 patients per group) was used to ensure that the sample was representative of the entire population.
Statistical analysis
IBM Statistical Package for Social Sciences (SPSS) statistics software (version 22.0; IBM Corp., USA) was used to code, tabulate, and statistically analyze the collected data. Quantitative data were tested for normality using the Shapiro-Wilk test. Normally distributed data were compared using the independent t-test (group comparisons) and paired t-test (time comparisons) and are described using the mean ± standard deviation (SD). Non-normally distributed data were compared using the Mann-Whitney test and are described using the median (first – third interquartile range). Qualitative data were compared using Fisher’s exact test and are presented as numbers and percentages. The level of significance was set at a P < 0.05.
Results
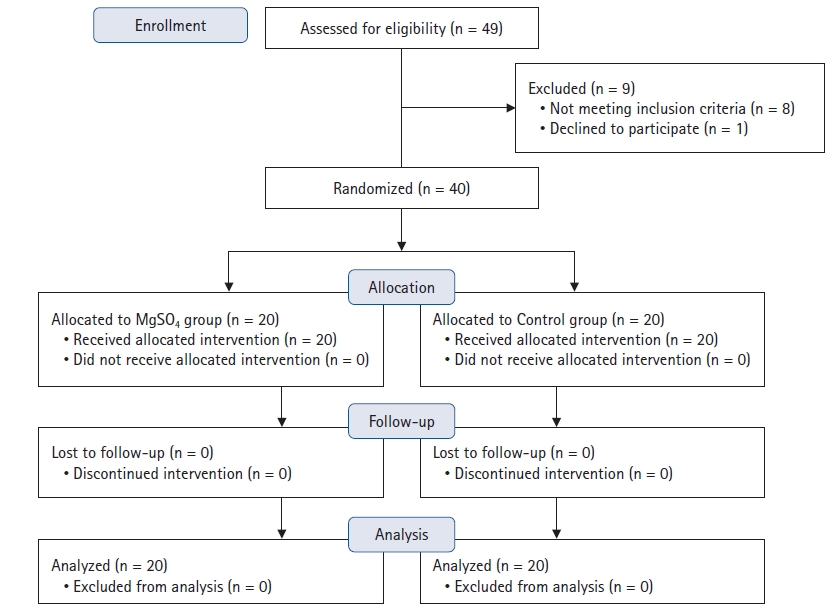
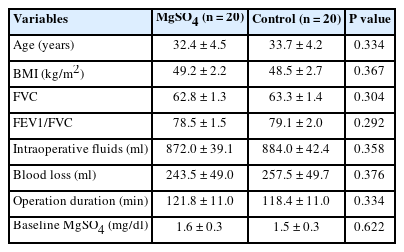
While 49 individuals were recruited for this study, eight patients did not meet the study’s inclusion criteria and one patient declined to participate. Thus, a total of 40 patients were included in this study. The patients were divided into two groups of 20 patients each (Fig. 1). Baseline characteristics (age, BMI, FVC, FEV1/FVC ratio, intraoperative fluids, blood loss, operation duration, and baseline MgSO4 levels) were not statistically significantly different between the groups (Table 1).
In terms of intraoperative oxygenation, the PaO2/FiO2 ratio decreased significantly among patients in the control group at 90 min intraoperatively compared with baseline, whereas no significant decrease was observed among patients in the MgSO4 group at 90 min intraoperatively compared with baseline. Additionally, the PaO2/FiO2 ratio at 90 min was not significantly different between the groups; however, the Δ PaO2/FiO2 ratio at 90 min increased in the MgSO4 group compared to the control group (mean ± SD: −0.8 ± 1.8 vs. −16.9 ± 3.9, respectively), with a statistically significant difference (mean ± SE: 16.1 ± 1.0, 95% CI [14.1, 18.1], P < 0.001; Table 2).
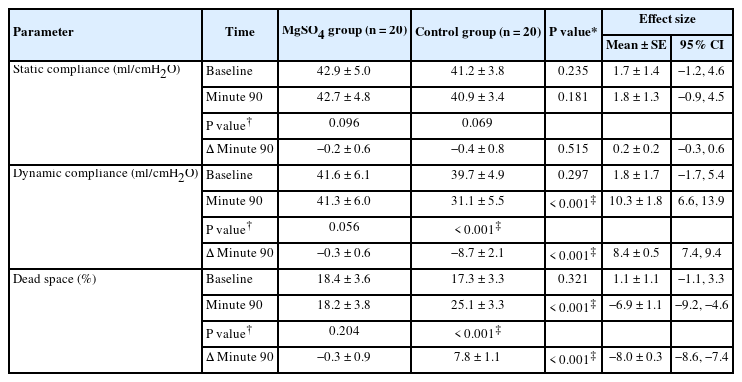
In terms of lung mechanics, static compliance was not significantly different between the two groups at baseline or at 90 min intraoperatively. In addition, static compliance at 90 min compared to baseline was not significantly different between the two groups (Table 3). In contrast, dynamic compliance was significantly higher in the MgSO4 group than in the control group at 90 min intraoperatively (P < 0.001). Although dynamic compliance decreased significantly at 90 min in the control group compared to baseline (P < 0.001), no significant difference was found at 90 min in the MgSO4 group compared to baseline (Table 3).
In terms of dead space, no significant differences were observed in the MgSO4 group at 90 min intraoperatively compared to baseline, whereas a significant increase was observed in the control group (P < 0.001). In the between-group comparison, the dead space was significantly higher in the control group than in the MgSO4 group at 90 min postoperatively (P < 0.001) (Table 3). The Δ dynamic lung compliance was higher in the MgSO4 group than in the control group at 90 min intraoperatively (mean ± SD: −0.3 ± 0.6 ml/cmH2O vs. −8.7 ± 2.1 ml/cmH2O, respectively), with a statistically significant difference (mean ± SE: 8.4 ± 0.5 ml/cmH2O, 95% CI [7.4, 9.4], P < 0.001). Additionally, the Δ dead space (%) was lower in the MgSO4 group than in the control group (mean ± SD: −0.3 ± 0.9% vs. 7.8 ± 1.1%, respectively), with a statistically significant difference (mean ± SE: −8.0 ± 0.3%, 95% CI [−8.6, −7.4], P < 0.001; Table 3).
Regarding hemodynamic parameters, no significant between-group differences were noted in the mean HR and MAP at baseline. However, the mean intraoperative HR and MAP were significantly lower in the MgSO4 group than in the control group from 30 to 90 min (P < 0.001) (Figs. 2 and 3).
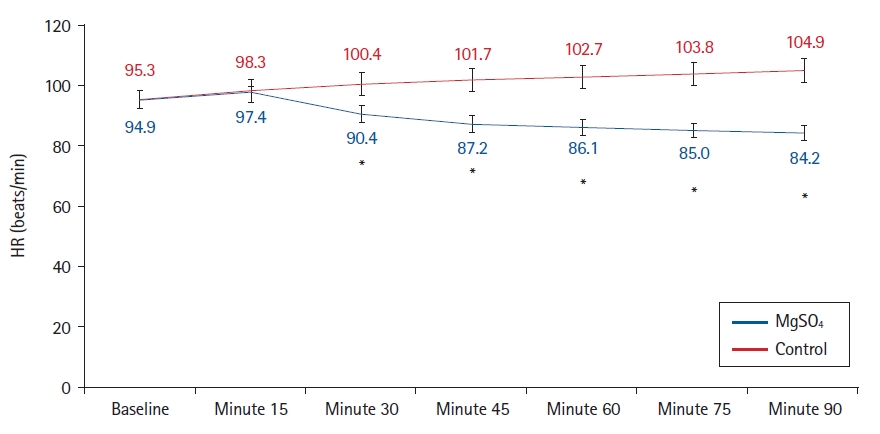
Comparison of the intraoperative heart rate (beats/min) between the study groups. Lines are the mean data and error bars are the standard deviation. *P < 0.001 compared to the control group. HR: heart rate.
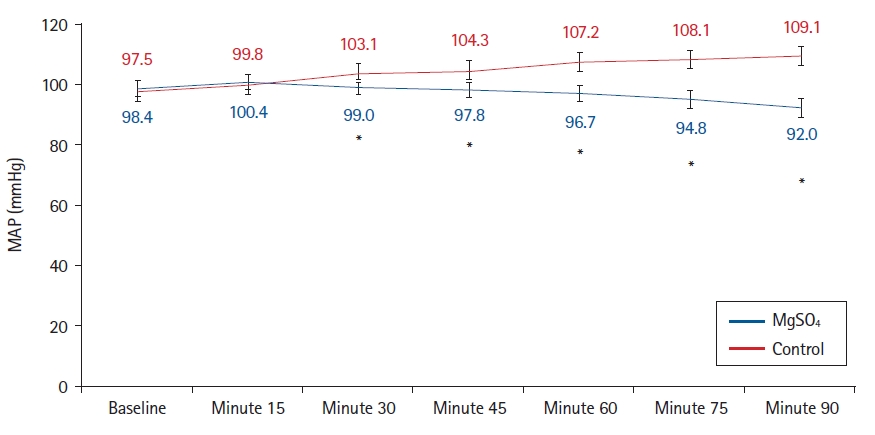
Comparison of the intraoperative mean arterial pressure (mmHg) between the study groups. Lines are the mean data and error bars are the standard deviation. *P < 0.001 compared to the control group. MAP: mean arterial pressure.
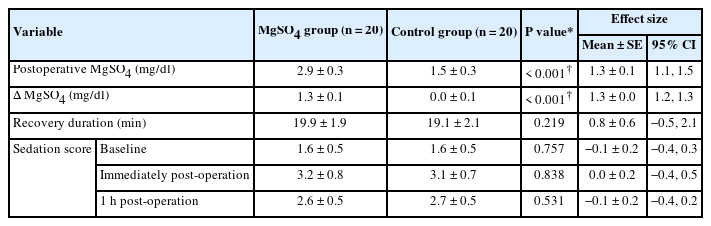
Postoperative MgSO4 and Δ MgSO4 levels were significantly higher in the MgSO4 group than in the control group (P < 0.001). No significant differences were noted between the groups in terms of duration of recovery (P = 0.219) (Table 4).
In addition, no significant differences were found between the MgSO4 and the control groups regarding the need for ICU admission or invasive ventilation postoperatively. Three patients (15%) in the MgSO4 group experienced postoperative hypoxia in the PACU that required ICU admission compared to five patients (25%) in the control group (relative risk [RR] = 0.60, 95% CI [0.17, 2.18], P = 0.695). In addition, two patients (10%) in the MgSO4 group required invasive ventilation compared to four patients (20%) in the control group (RR = 0.50, 95% CI [0.10, 2.43], P = 0.661). No significant differences in sedation scores were found between the two groups at baseline, immediately postoperatively, or 1 h postoperatively (Table 4). Additionally, none of the patients in either group developed any other postoperative complications such as bleeding or leakage.
Discussion
This study demonstrated that infusing MgSO4 intraoperatively has protective effects on arterial oxygenation and lung mechanics in morbidly obese patients with restrictive lung disease undergoing bariatric surgery under general anesthesia. MgSO4 significantly preserved arterial oxygenation by inhibiting a reduction in the intraoperative PaO2/FiO2 ratio. Furthermore, MgSO4 was able to maintain dynamic lung compliance (no significant decrease) and dead space (no significant increase) during general anesthesia and mechanical ventilation; however, the clinical relevance of these findings is minimal.
To our knowledge, this is the first clinical study to examine the effects of intraoperative MgSO4 infusion on arterial oxygenation and lung mechanics in morbidly obese patients undergoing bariatric surgery.
Obesity has been shown to cause alterations in lung physiology, including increased respiratory rate, reduced lung volume, diminished chest and lung compliance, increased airway resistance (referred to as decreased lung volume, small airway closure, and airway remodeling by proinflammatory adipokines), and increased oxygen consumption. Furthermore, obesity has been associated with an increased alveolar-arterial oxygen gradient caused by ventilation-perfusion mismatch due to microatelectasis, which worsens in the supine position [24]. Obesity-related increases in adipose tissue mass are associated with enhanced mast cell proliferation. Since mast cells are the primary mediators of allergies, obesity-induced mast cell proliferation may represent a potential pathway for airway illnesses in obese individuals [25].
Patients with morbid obesity are at risk of rapid oxygen desaturation upon general anesthesia induction because the FRC is decreased by approximately 50% compared to preoperative values [4]. The impact of general anesthesia is further intensified by mechanical ventilation and the use of muscle relaxants, which may compromise pulmonary function, lung compliance, and gas exchange owing to the development of atelectasis. Additionally, the patient’s position and use of the pneumoperitoneum may lead to further impairment [26,27].
In our study, administering MgSO4 maintained the arterial oxygenation by preventing a reduction in the intraoperative PaO2/FiO2 ratio. However, given the small effect size of our study, the clinical significance of these findings is minimal. MgSO4 may preserve intraoperative arterial oxygenation in patients with obesity by promoting both pulmonary vasodilation and bronchodilatation, leading to improved perfusion and ventilation. In general, the therapeutic effects of magnesium may be attributed to its effects as a calcium antagonist [28,29].
MgSO4 can enhance vasodilation by relaxing the tone of the vascular smooth muscles. Moreover, MgSO4 promotes the local synthesis of vasodilator substances such as nitric oxide and prostaglandins (e.g., prostacyclin) [30]. In terms of magnesium-induced bronchodilation, various experimental data suggest that several pathways may be involved, such as the suppression of cholinergic neuromuscular transmission, inhibition of calcium-induced muscle contractions, attenuation of histamine release, reversal of magnesium depletion following β-adrenergic therapy, and enhancement of the effects of β-agonists on adenylyl cyclase [31–34]. Magnesium also has sedative properties that help people relax and achieve anxiolysis, particularly during acute bronchoconstriction [30].
Additionally, magnesium relaxes rabbit bronchial smooth muscles in a dose-dependent manner when exposed to histamine, bethanechol, or electrical impulses [31]. Similarly, magnesium increases the percentage of the bronchial cross-sectional area in dogs following histamine-elicited bronchoconstriction in vivo and relaxes histamine-induced contractions of guinea pig tracheal strips in vitro [35].
Furthermore, MgSO4 has been found to have bronchodilation effects regardless of baseline serum magnesium levels, even after short periods of drug infusion [27]. These findings could help explain the positive effects of MgSO4 infusions on dynamic compliance and dead space observed in this study. Our results are similar to those of a previous study conducted by Ahmed et al. [20], which showed that an intraoperative infusion of MgSO4 resulted in mild perioperative protective effects against both arterial oxygenation and lung mechanics in patients with moderate COPD following laryngectomy under general anesthesia.
In the current study, the post-infusion serum magnesium level in the Mg group was 2.9 ± 0.3 mg/dl, which is lower than levels associated with magnesium toxicity. Loss of the patellar reflex occurs with plasma levels of 9.6–12 mg/dl, whereas respiratory depression occurs at levels of 12–18 mg/dl [36].
MgSO4 is readily accessible and affordable, with few side effects when administered at recommended doses [37]. It has a rapid onset of action when administered intravenously, which is critical in emergencies. In addition, intravenous MgSO4 is rapidly eliminated from the kidneys. However, this is both a therapeutic opportunity and a challenge. As maximal renal tubular reabsorption of magnesium occurs at normal serum levels and renal clearance increases linearly with higher concentrations, achieving a sustained spasmolytic effect is not easy [38]. The infusion rate, rather than the overall dosage or infusion time, has a greater impact on the maximum serum level throughout treatment. Since it was first described in 1936, the ideal bolus dose of intravenous MgSO4 has not yet been identified. Consequently, a wide dose range of 25–100 mg/kg has been used [38–42].
MgSO4 has been found to have several therapeutic effects in clinical anesthesia, including enhancing postoperative analgesia and reducing the consumption of other anesthetics, opioids, and hypnotics [37]. However, the adverse effects are generally moderate and include intravenous injection pain, residual neuromuscular blockade, and hypotension. Hypermagnesemia is an uncommon complication that usually affects patients with renal failure who are receiving medicines containing magnesium [43]. However, close monitoring is still needed to promptly detect and manage adverse events [44]. No magnesium-related complications were observed in this study.
This study had some limitations. As we enrolled only morbidly obese patients with restrictive lung disease, our findings cannot be generalized to other patient populations. Additionally, this study only included patients who underwent bariatric surgery; therefore, our results should be validated using other surgical procedures. Finally, because intraoperative MgSO4 infusions were not maintained until the end of the procedure, outcomes may vary with longer infusions or greater plasma concentrations.
In conclusion, the intraoperative administration of MgSO4 infusion significantly preserved arterial oxygenation and maintained dynamic lung compliance and dead space in morbidly obese patients; however, the clinical relevance of these findings is minimal. This study failed to adequately reflect the clinical importance of these results.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Marwa M. Mowafi (Conceptualization; Data curation; Investigation; Methodology; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)
Marwa A. K. Elbeialy (Data curation; Investigation; Methodology; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)
Rasha Gamal Abusinna (Data curation; Investigation; Methodology; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing)