Endotracheal intubation in patients undergoing open abdominal surgery in the lateral position: a comparison between the intubating video stylet and fiberoptic intubating bronchoscopy
Article information
Abstract
Background
Some situations compel anesthetists to execute endotracheal intubation in the lateral position. We compared elective endotracheal intubation in the lateral decubitus position using the video stylet (VS) device with the fiberoptic (FO) bronchoscope device in patients undergoing abdominal surgery.
Methods
Overall, 50 patients were enrolled in this prospective, randomized study. They were randomly classified into the VS intubation or FO intubating bronchoscope group. After anesthesia induction, patients were placed in the lateral decubitus position, and a single investigator well-versed with the use of the VS and FO bronchoscope performed the intubation. The primary outcome was the time taken for intubation. Secondary outcomes included the intubation success rate, hemodynamic response at specific time points and perioperative complications.
Results
The average time taken for intubation was significantly lesser in the VS group than in the FO group, with values of 39.5 ± 10.0 and 75.6 ± 16.2 s, respectively (P < 0.001). Incidences of a successful first attempt of intubation in the VS and FO groups were 88% and 100%, respectively, showing no significant difference. There was a negligible difference in complications between the groups, except sore throat, which showed a higher incidence in the VS group than in the FO group (P = 0.002).
Conclusions
In laterally positioned patients, elective endotracheal intubation with VS provides less intubation time; however, its use is accompanied by a significant increase in the hemodynamic response after intubation and an increased incidence of sore throat.
Introduction
A difficult task confronting an anesthetist is airway management, which is also a main cause of morbidity related to anesthesia [1]. Accordingly, it is crucial for any anesthetist to acquire skills to handle challenges encountered in the operating theater [2]. One of them is intubation in uncommon positions, such as the lateral position, when it is problematic to put the patient in the supine position, such as in cases of accidental loss of the endotracheal tube (ETT) in the middle of operation, patients with trauma, inefficient regional anesthesia, and neoplasms of the back, occiput, or sacral region [3,4]. Recently, placing the ETT in the lateral position has been a huge concern for many anesthetists; moreover, several studies have been performed to determine the best method for lateral position intubation by using direct laryngoscopy, laryngeal mask airway, intubating the laryngeal mask airway with and without the aid of a lightwand, and intubation with the lightwand [5,6]. Unfortunately, these techniques have drawbacks of being time-consuming and putting the anesthetist in an ergonomically challenging position [7]. As a result, it was considered important to discover more ways that are both safe and successful. The fiberoptic (FO) bronchoscope was believed to achieve the sought goals [8,9]. However, it is a costly apparatus that requires thorough training. Therefore, current studies are investigating the pros of using the video rigid intubation stylet. It is a novel device with several advantages, including easy mobility with a clear display screen for vocal cord visualization, easy to clean, lightweight, chargeable, reusable, durable, and less expensive. It has a red-light source that is located at the far end of the stylet. Therefore, it is considered to be a more affordable choice than the FO bronchoscope in developing countries [10].
The aim of the present study was to compare the video stylet (VS) with the FO bronchoscope in laterally positioned patients undergoing laparotomy abdominal surgery.
Materials and Methods
This study was performed as a prospective randomized study at the Theodor Bilharz Research Institute Hospitals and Cairo University Hospital, after receiving approval from the Institutional Research Ethics Committee of the Faculty of Medicine, Cairo University (MD-53-2019) and Theodor Bilharz Research Institute Hospitals (No: 194471), with registration at ClinicalTrials.gov (NCT 04183959). The study was conducted in accordance with the Declaration of Helskinki and Good Clinical Practice. Written consent was obtained from each patient before enrollment in this study, which was designed to recruit 50 patients, including both men and women, between 18 and 60 years of age with the American Society of Anesthesiologists (ASA) physical status I or II, Mallampati class I or II, scheduled endotracheal intubation in the lateral decubitus position under general anesthesia for open abdominal surgery.
Exclusion criteria were pre-existing clinically significant cardiovascular or hypertensive disorders, age under 18 or over 60 years, ASA physical status class > II, difficult intubation, Mallampati class > II, limited neck mobility due to cervical spine pathology, dental abnormalities, obesity (body mass index [BMI] ≥ 40 kg/m2), and a high risk of pulmonary aspiration. Before the start of the study, enrolled patients were randomly allocated into 2 equal groups, using a computer-generated table of random numbers with an opaque and sealed envelope prepared by a research assistant not otherwise participating in the study, according to the device used in intubation, into VS intubation and FO bronchoscope intubating groups.
One day before surgery, patients visited the anesthesia outpatient clinic for history-taking and assessment, including electrocardiogram, complete blood count, and coagulation profile. The study protocol was explained to them, and they were informed that they could drop out any time they desired. All patients fasted for 6 h before the procedure. After demographic data had been recorded, intravenous access was established with a 20 gauge (G) intravenous (IV) cannula over the forearm on arrival at the operating theater. Simultaneously, standard monitoring devices were attached, including the electrocardiograph, noninvasive blood pressure monitor, and pulse oximeter.
All patients were premedicated IV with ondansetron 4 mg and pantoprazole 40 mg. The anesthetic protocol was standardized in all the study groups. After pre-oxygenation for 5 min, anesthesia induction was commenced using propofol (1–2 mg/kg) with IV fentanyl (1–2 µg/kg) until loss of verbal communication occurred. Subsequently, muscle relaxation was maintained by an initial loading IV dose of cisatracurium (0.15 mg/kg). After adequate oxygenation and muscle relaxation, patients were placed in the lateral position and an inflatable beanbag was used to achieve the anterior and posterior support needed. The dependent lower limb of the patient was flexed, and a pillow was placed between both lower limbs to cushion the knees' bony protrusions. Moreover, the upper limbs were protected using pillows to support the non-dependent upper limb, while the dependent one was rested on an arm board. Furthermore, an axillary roll was used to prevent axillary vessels and brachial plexus injuries by positioning between the operating table and the patient's chest wall. The head and neck were kept in the neutral position through support using a firm 6-cm high pillow comprising 2 separate parts: one made of foam and another made of a synthetic gel substance in the horseshoe shape placed on top to help fixate the head in a proper and correct way, with attention paid to the dependent eye and ear to avoid pressure and ischemia [5]. Subsequently, patients were randomly allocated to the 2 groups, with 25 patients in each.
VS group: The trachea was intubated using a laryngoscopic-assisted VS (Red-Light Directive Video Rigid Intubation stylet [BD-SL-A]; Shenzhen Besdata Technology Co., Ltd., China) by the consultant anesthesiologist expert with the use of the VS. Subsequently, an ETT was placed over the device and introduced into the mouth, and on visualizing the first 1 or 2 tracheal rings, the tube was slid into the airway.
FO group: Intubation was performed using an FO bronchoscope (RBS, Series Portable Fiber Intubation Scope, Pentax F1-16BS 5.2 mm, Pentax, USA) by the anesthesiologist expert with the use of the FO bronchoscope. For the FO bronchoscope, the scope was inserted carrying the ETT until the carina was visualized, and the tracheal tube was slid into the airway. In both groups, a trained assistant was present to help perform the maneuvers, such as lingual traction and anterior mandibular advancement to clear the airway. Each maneuver alone proved beneficial; nevertheless, they were more effective when performed together. The intubation process was thought to be a failure when not completed within either of the 2 trials or the patient's oxygen saturation (SpO2) reached < 90%. In cases of intubation failure, the patient was turned to the supine position and intubated with the conventional technique. After confirmation of successful intubation by capnography and chest auscultation, the patient was placed on mechanical ventilation with isoflurane 2% to maintain anesthesia. End-tidal CO2 was maintained between 35 and 40 mmHg. Muscle relaxation was maintained with 0.03 mg/kg IV of cisatracurium every 20 min, and surgery was continued in the required position (supine or lateral). Upon completion of the procedure, the inspired anesthetic was then stopped and neostigmine 0.05 mg/kg combined with atropine 0.02 mg/kg were used to reverse the effect of the muscle relaxant. Subsequently, extubation was performed after fulfilling the criteria of extubation. Finally, the patient was taken to the post-anesthesia care unit, and duration of surgery was recorded.
The primary outcome of the current study was the time required to intubate (defined as the time from the instrument's introduction into the subject's mouth until its removal following confirmation of the ETT correct placement by witnessing the optimal waveform on capnography). The secondary outcome was the success of intubation. The anesthesiologist who performed the intubation was asked to score the ease of use on a 4-point scale (1 = difficult; 2 = moderately difficult; 3 = fairly easy; and 4 = very easy), vital signs based on systolic arterial blood pressure (SBP), mean arterial blood pressure (MBP), diastolic arterial blood pressure (DBP), heart rate (HR), and SpO2. The latter was measured at baseline before anesthesia induction (BA), immediately after induction (AA), after induction of anesthesia but before intubation (T1), and after successful ETT placement (T2). The occurrence of side effects, including mucosal injuries, i.e., blood detected on the device, lip or dental trauma, postoperative nausea or vomiting, and desaturation (SpO2 < 92%) were recorded.
Statistical analysis
Sample size was calculated by comparing the intubation time between using the VS and FO maneuver in the lateral position of open abdominal surgery cases, as previously reported [10]. The mean time of intubation was approximately 19.7 ± 2.8 s in the VS group and approximately 38.2 ± 6.9 s in the FO maneuver group (Standard deviation was calculated from the given 95% CI). Thus, the minimum proper sample size was calculated to be 22 participants in each group to enable detecting a real difference of 6 s (15% of the control group) with 80% power at the α = 0.05 level when using Student's t-test for independent samples. Sample-size calculation was performed using Stats Direct statistical software version 2.7.2 for MS Windows (Stats Direct Ltd., UK). The number was increased to 50 patients (25 per group) to compensate for possible dropouts. Normally distributed continuous data are expressed as mean ± standard deviation. Non-normally distributed continuous and ordinal data are expressed as median (Q1, Q3). Categorical data are expressed as number of patients and incidence. The unpaired t-test was used to compare continuous data in the 2 groups. Repeated-measures analyses of variance with post-hoc Dunnett's test was used to compare changes in continuous variables in relation to the baseline preoperative values, e.g., HR, SBP, MAP, and DBP within each study group. The chi-square or Fisher's exact test was used to compare categorical data. For all statistical comparisons, a P value < 0.05 was considered significant. All data analyses and graphical demonstrations were dose-dependent and performed with the Statistical Package for Social Sciences SPSS ver. 25.0 software for Windows (IBM Corp., USA).
Results
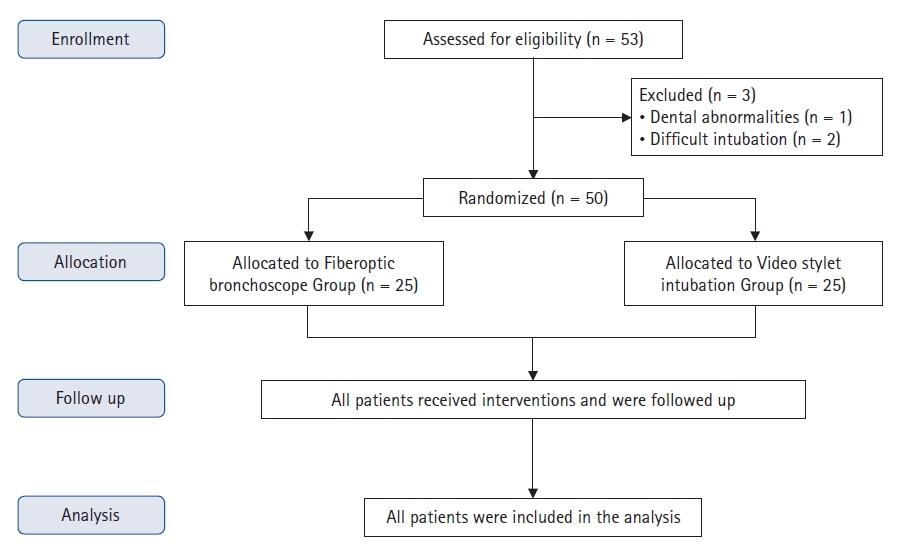
Fifty-three patients were assessed for eligibility, of whom 3 were excluded based on the exclusion criteria. Thus, 50 patients were included in the study (Fig. 1).
There were no statistically significant differences in patient characteristics or airway parameters among groups (patient age, BMI, or Mallampati score). Intubation was successful at the first attempt in 22 (88%) patients of the VS group and in 25 (100%) patients of the FO group, showing no significant differences. However, the average time required for intubation was remarkably lower (P < 0.001) in the VS group than in the FO group at 39.5 ± 10.0 and 75.6 ± 16.2 s, respectively. At the end of intubation, we asked the anesthesiologists about their satisfaction with the ease of using this technique of intubation. The result showed that anesthesiologists were satisfied when using the VS for intubation compared to the FO bronchoscope (Table 1).
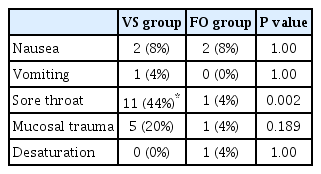
Hemodynamically, both groups were comparable regarding changes in SBP, MBP, DBP, HR, and SpO2, showing no statistically significant differences in BA, AA, or T1. However, immediately after successful intubation, T2 showed significant increases in SBP, MAP, DBP, and HR in the VS group compared to the FO group. Moreover, the mean SpO2 showed significant reduction in the FO group compared to the VS group (Figs. 2 and 3).
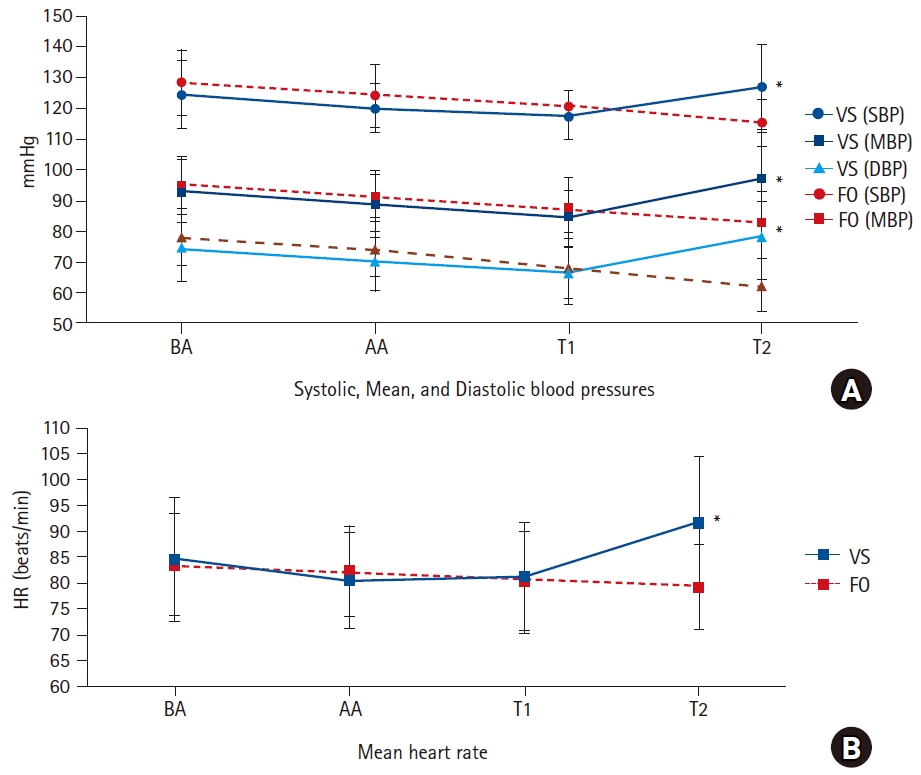
Comparison of the systolic, mean, and diastolic blood pressures and mean heart rate. Values are presented as mean ± SD. VS: video stylet intubation group, FO: fiberoptic bronchoscope group, BA: before induction of anesthesia at baseline, AA: immediately after induction of anesthesia, T1: after induction of anesthesia but before tracheal intubation, T2: immediately after successful intubation, SBP: systolic blood pressure, MBP: mean blood pressure, DBP: diastolic blood pressure, HR: heart rate. *P < 0.05.

Comparison of the mean oxygen saturation (SpO2) of the 2 studied groups. Values are presented as mean ± SD. VS: video stylet intubation group, FO: fiberoptic bronchoscope group, BA: before induction of anesthesia at baseline, AA: immediately after induction of anesthesia, T1: after induction of anesthesia but before tracheal intubation, T2: immediately after successful intubation. *P < 0.05.
Complications detected in the VS group included 11 cases (44%) of sore throat, 5 cases (20%) of mucosal trauma, 2 cases (8%) of nausea, 1 case (4%) of vomiting, and no case of desaturation and those detected in the FO group included 1 case (4%) of sore throat, 1 case (4%) of mucosal trauma, 2 case (8%) of nausea, 1 case (4%) of desaturation, and no case of vomiting. There was insignificant difference between groups in complications, except for the incidence of sore throat, which was significantly higher in the VS group than in the FO group (P = 0.002; Table 2).
Discussion
Intubation is considered a fundamental step in the management of airway, particularly when it is done in an unconventional position, such as the lateral position, or in patients with a restricted mouth opening or a restricted range of neck movement, as any deficiency in the airway management in these patients can lead to fatal outcomes. Recently, many researchers have developed methods, including the FO bronchoscope and rigid VS, for airway management in unusual positions. The rigid VS had many advantages in these extreme cases of preventing blind traumatic intubation and providing easy maneuver. Moreover, it is easy to master and adaptable to shape for better adjustment in patients with a distorted anatomy. Unfortunately, it has limitations of the inability to be used for nasal intubation in addition to not having a suction channel or oxygen delivery port. Finally, it affords only a limited view, as it can be seen only as far as the proximal trachea [11,12].
The current study concluded that the outcome of using the VS to intubate patients in the lateral position undergoing laparotomy abdominal surgery appeared to be faster, showing more than a 36 s difference between the 2 devices, which can be explained by the more time required to slide the ETT along the longer FO bronchoscope stylet. Furthermore, the need for advancement of the FO bronchoscope up to the carina and that of an assistant to uplift the patient's chin when using the FO bronchoscope can be considered as reasons for such delay. Using the VS was also shown to yield a more favorable intubation condition compared to using the FO laryngoscope. However, despite almost similar success rates, as successful intubation at the first attempt using the VS was shown to be 88% compared to the 100% found in the FO laryngoscope, the VS experienced higher failure rates, which could be attributed to several factors, including difficulty in shaping its stylet after mouth insertion, poor image quality, and lack of a suctioning port [13,14].
Concerning the incidence of complications, despite the higher rates of hypoxia shown in the FO bronchoscope group mainly due to the longer time needed for intubation, higher increases in hemodynamic parameters, including BP and HR, were measured in the latter group. This could be explained by sympathetic stimulation resulting from jaw thrust performed during intubation using the VS; moreover, more manipulations required to centralize the vocal cords could lead to a catecholamine surge [15]. However, there was an insignificant difference in the occurrence of complications between the groups, except for sore throat. This appeared to be higher when using the VS compared to the FO bronchoscope, which can be explained by the rigidity of its stylet.
Lee et al. [11] conducted a study involving 80 patients undergoing nasotracheal intubation to compare the use of the flexible FO bronchoscope with the VS with regards to the time required for intubation and complication incidence. The study showed a 36.4-s delay when using FO bronchoscopy compared to the VS. However, there was a statistically insignificant difference when comparing both groups in terms of complications.
Another study was performed involving 60 patients undergoing elective procedures in the supine position with the normal airway to compare the time required for intubation between the VS and the FO bronchoscope, showing an 18.5 s difference between the groups with a greater delay when using the FO bronchoscope. Moreover, no statistically significant differences were found in hemodynamic response or complications [10]. A study conducted by Ong et al. [16] was performed to compare the VS and the Macintosh laryngoscope under 4 different conditions, which were normal airway, immobilization of the cervical spine, tongue swelling with cervical spine fixation, and tongue edema. It was concluded that the use of the VS device appeared to have superior outcomes concerning time of intubation and learning time compared to FO bronchoscopy. Another study was performed comparing the intubation time with the incidence of complications when using the VS and FO bronchoscopy for patients undergoing thoracic surgery using a left-sided double-lumen tube. The result was shorter time required for intubation using the VS and lower rates of hoarseness and sore throat [17]. A similar study was conducted involving 200 patients using the VS OptiScope™, which showed higher rates of success for a single intubation trial and fewer postoperative complications [18].
In contrast, some authors claimed that intubation time using the VS was not short compared to that using the Macintosh manual blade [19]. Others claimed that using the OptiscopeTM, which is a VS device, did not show hemodynamic response modifications but provided better vocal cord visualization compared to the conventional laryngoscope for intubation [20].
Some limitations were present in our study. First, all participants had average BMI scores and normal airways; therefore, our results may not be generalizable for difficult intubation cases. Second, the VS does not have suction or oxygen supplementation outlets; these might be considered as drawbacks when secretions or blood accumulates in the nasopharynx or oropharynx. Finally, in the current study, the instruments were used by an expert anesthesiologist, so the outcome of use by inexperienced personnel remains unknown.
In conclusion, in laterally positioned patients, elective endotracheal intubation with VS provides less intubation time; however, its use is accompanied by a significant increase in the hemodynamic response after intubation and an increased incidence of sore throat. Nevertheless, more studies using a larger sample size are required to decide its use in patients with a difficult airway and the incidence of complications.
Acknowledgements
Our sincere thanks and gratitude to all those who participated in this study and helped accomplish this work.
Notes
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Study equipment was provided by Cairo University Hospital and Theodor Bilharz Research Institute Hospital.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Amr Samir Wahdan (Methodology; Data collection; Formal analysis; Writing – original draft; Writing – review & editing)
Nesrine Abdel Rahman El-Refai (Conceptualization; Supervision; Writing – original draft; Writing – review & editing)
Sohaila Hussien Omar (Conceptualization; Supervision; Writing – original draft; Writing – review & editing)
Shady Amr Abdel Moneem (Investigator; ; Data collection; Writing – original draft; Writing – review & editing)
Mennatallah Magdi Mohamed (Writing – review & editing)
Mohamed Mahmoud Hussien (Methodology; Data collection; Writing – original draft; Writing – review & editing)