Infection control of operating room and anesthesia for cesarean section during the COVID-19 outbreak in Daegu, the Republic of Korea -a case series-
Article information
Abstract
Background
The coronavirus disease-19 (COVID-19) was first reported in Wuhan, China, with Korea being subsequently exposed. In Korea, COVID-19 screening guidelines have been established in every hospital as an attempt to prevent its spread. There has been a previous report of a successful cesarean section of a confirmed mother; however, there remain no guidelines for suspected mothers. Cesarean section is often urgently operated without sufficient infection evaluations. We would like to suggest anesthetic management guidelines for cesarean section patients suspected of COVID-19.
Case
Our hospital, which is located in Daegu, Korea, was designated as a quarantine and delivery facility for suspected mothers. We performed the cesarean section on seven suspected mothers and one confirmed mother.
Conclusions
This case report presents guidelines for infection control during surgery and anesthesia for cesarean section of mothers with suspected COVID-19 involving operating room preparation and protection strategy.
In 2019, the novel coronavirus disease-19 (COVID-19) was reported in Wuhan, which has since spread in China and worldwide, including Korea [1,2]. Our hospital’s medical staff have established and followed guidelines to prevent the virus spread in the operating room, as well as exposure of medical staff to the virus. Specifically, uninfected fetuses at risk of viral infection have been delivered from COVID-19 confirmed mothers through cesarean section (C-sec), which indicates the possibility of safe delivery from COVID-19 confirmed mothers [3]. However, since C-sec is often performed urgently since the life of the mother or fetus could be at risk, surgeons proceed with the surgery before receiving the results of COVID-19 reverse transcription-polymerase chain reaction (RT-PCR). Here, we aim to present reports regarding the management of confirmed and suspected patients with COVID-19, as well as the guidelines of perioperative management for surgery and anesthesia preparation.
Case Reports
Our hospital is located in Daegu, which has the largest number of infected patients among the cities in Korea. A total of twelve mothers with suspected COVID-19 were admitted for delivery between February 26 and April 3, 2020. Four mothers with fever symptoms gave birth through normal vaginal delivery. After consulting an obstetrician, eight COVID-19 related mothers (including one confirmed and seven suspected) undergoing C-sec were treated (Table 1). Case #4 had been previously diagnosed with COVID-19 infection and had self-isolated at home. Among these patients, three had preeclampsia, two had premature rupture of membranes (PROM) with dystocia, one had PROM with fetal distress, one had dystocia caused by cephalopelvic disproportion, and one had preterm labor with fetal distress. Five of the seven suspected patients had fever, one had dyspnea, and one had both fever and dyspnea. Given the patients’ symptoms, COVID-19 could not be excluded; therefore, they were transferred through an exclusive passage and elevator from the hospital entrance triage without passing the gynecology outpatient clinic in our hospital. They were admitted to the negative pressure-quarantine room in the delivery center for a minimum of 15 minutes and a maximum of 60 minutes until just before surgery. The preoperative evaluation involved laboratory tests, chest X-ray, electrocardiogram, and COVID-19 RT-PCR. However, if C-sec was to perform urgently, the surgery was performed without waiting for the results of routine laboratory tests. Case #4 (COVID-19 confirmed patient) was admitted for emergency C-sec due to obstructed labor caused by cephalopelvic disproportion. After admission, she had a COVID-19 RT-PCR test again. An urgent C-sec was required immediately before the reception of the RT-PCR results for the seven suspected mothers. All seven suspected patients were prepared for surgery and anesthesia as per the hospital’s guidelines for patients with COVID-19 (Fig. 1).
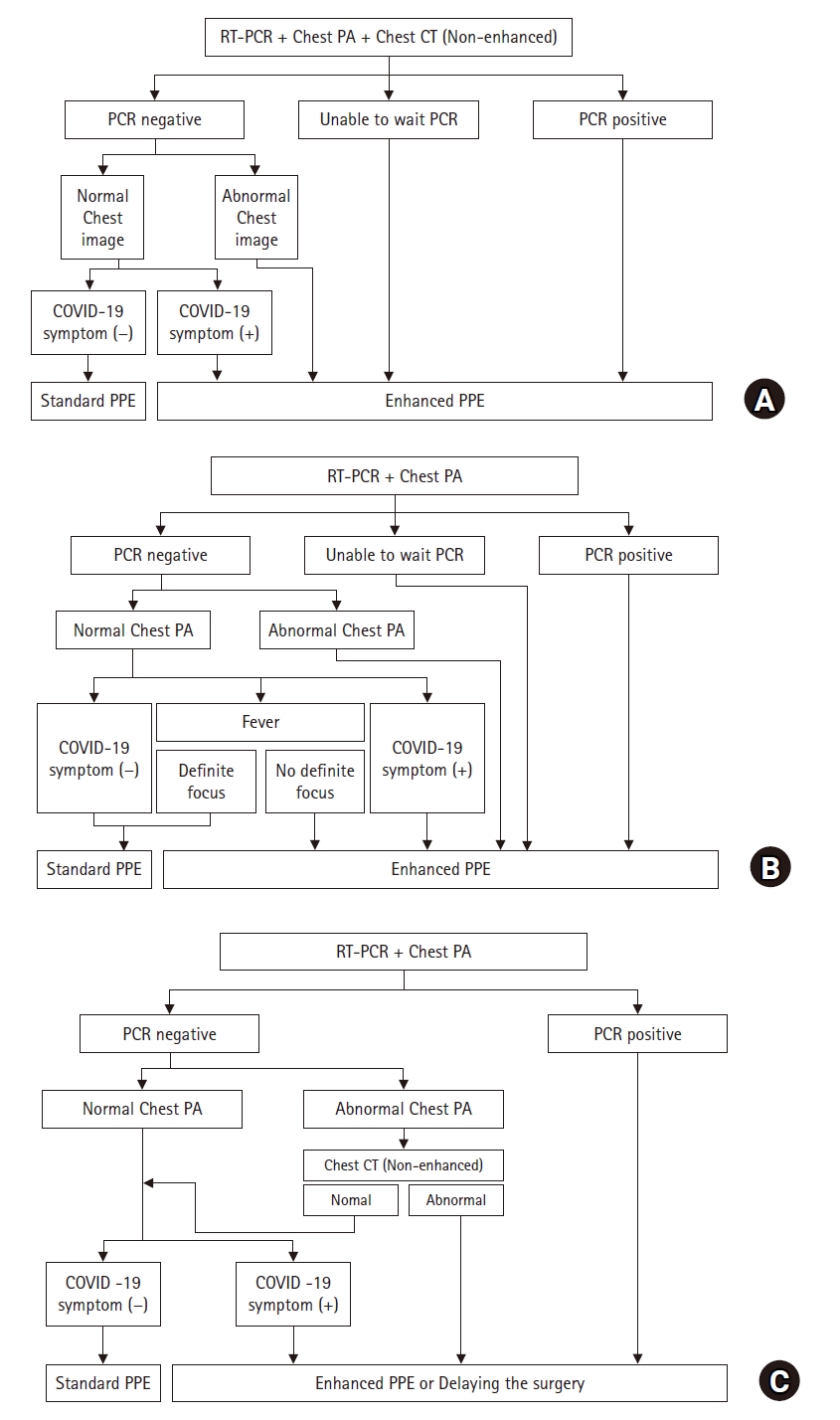
Guidelines for operation during the Coronavirus disease-19 (COVID-19) outbreak. Enhanced personal protective equipment (PPE) includes N95 mask, full body impermeable suit, double gloves, shoe covers, and hood with surgical cap. Standard PPE includes goggle, N95 mask, plastic gown, and disposable surgical gloves. (A) Guideline for emergent surgery. (B) Modified guidelines for cesarean section. (C) Guideline for elective surgery. COVID-19 symptoms include fever, cough, dyspnea, myalgia or fatigue, sputum production, headache, and diarrhea. RT-PCR: reverse transcription-polymerase chain reaction, Chest PA: chest posteroanterior, Chest CT: chest computed tomography.
C-sec preparations were performed in the operating room, which is a negative-pressure room in the delivery center temporarily designed as part of the hospital policy for COVID-19 related C-sec. Unnecessary instruments for the surgery were removed and built-in instruments in the operating room were covered using plastic paper. Fluids, drugs, and other equipment required for surgery and anesthesia were prepared in sufficient quantities. Equipment and unused drugs and fluids were wiped using sodium dichloroisocyanurate solution immediately after surgery and before storage. Initially, spinal anesthesia was considered; however, equipment for general anesthesia was prepared in case of failed spinal anesthesia. These included a ventilator, breathing circuit, video laryngoscope (McGRATH MAC, Aircraft Medical Ltd., UK), high-efficiency particulate air (HEPA) filter, and drugs. All the health care workers (HCWs) wore enhanced personal protective equipment (PPE), including an N95 mask, full-body impermeable suit, double gloves, shoe covers, hood with a surgical cap, and powered air-purifying respirator (PAPR) before the patient arrived at the operating room (Fig. 2A). Standard PPE (Fig. 2B) was applied to HCWs who cared for asymptomatic COVID-19 exposed patients. Standard PPE includes surgical gloves, surgical gowns, eye shields and N95 mask. All 8 cases had COVID-19 suspected symptoms, HCWs all wore enhanced PPE.
After the anesthesiologist, surgeon, and nurses were ready and the operating room was set-up, the patients were transferred from the quarantine room to the operating room. Upon patient entry to the operating room, the door was not allowed to open. Patient intraoperative monitoring included electrocardiogram, non-invasive blood pressure, and SpO2. Seven patients underwent spinal anesthesia while one (case #2) underwent general anesthesia. For this procedure, a well-experienced anesthesiologist and one nurse were present in the operating room while another anesthesiologist was on call for unexpected situations. For spinal anesthesia, a 25-gauge Pencan spinal needle was inserted into the lumbar 3rd–4th intervertebral space; subsequently, 0.5% heavy bupivacaine 9 mg/1.8 cc with fentanyl 20 μg/0.4 cc was intrathecally injected. After 5 min, the neuraxial blockade was confirmed to reach the T4 level. The patient wore an N95 mask during anesthesia, surgery, and recovery. Case #2 underwent general anesthesia due to the failure of regional anesthesia caused by severe edema. A HEPA filter was applied between the breathing circuit and face mask where the patient was preoxygenated for 5 min. Subsequently, rapid sequence intubation without manual ventilation was performed to prevent the aerosolized virus from spreading in the room. Next, a video laryngoscope was used to increase the successful intubation rate. After the operation was completed, extubation was performed after confirmation of established regular breathing, adequate spontaneous ventilation, eye opening, and obeying commands. Further, 100% O2 2 L was supplied via a nasal cannula, which was covered with an N95 mask.
After surgery completion, the patients recovered in the operating room without being admitted to the post-anesthesia care unit. The anesthesiologist and nurse involved in the C-sec were similarly involved in the patient’s postoperative recovery. The patients who received spinal anesthesia recovered until the blockage level decreased to T8–T10. The patient who underwent general anesthesia was considered to have recovered when her post anesthetic recovery score was ≥ 9. In case of pain complaints, previously prepared analgesic agents, including opioids and non-steroidal anti-inflammatory drugs, were intravenously administered. We followed the post-anesthesia care unit discharge criteria as appropriate; however, given the fatigue of the HCWs, the recovery time was limited to 1 h. After recovery, the confirmed patient was transferred to the COVID-19 ward while the suspected patients were transferred to the COVID-19 suspect ward through an exclusive passage and elevator for patients with COVID-19. On the first post-operative day, all eight patients were confirmed to be negative by RT-PCR and were transferred to the general ward for postoperative treatment.
Discussion
COVID-19 is a quick-spreading virus; therefore, it is important to prevent its transmission from the operating room to vulnerable surgical patients and HCWs. Consequently, both confirmed and suspected patients should be isolated in the management of the operating room. For patients with any suspected symptoms, strict guidelines for isolation and operation room management are necessary [4]. Jiang et al. [5] reported that COVID-19 is clinically manifested as fever (> 90%), cough (around 70%), dyspnea (up to 50%), myalgia or fatigue (31–44%), sputum production (20–28%), headache (6.5–16%), and diarrhea (2–14%). Further, 81%, 14%, and 5% of patients present with mild, severe, and critical symptoms, respectively. The fatality rate is about 2.3% and it increases with age [6]. Therefore, early diagnosis and treatment are necessary even for mild symptoms [7]. In case of emergency C-sec patients with suspected symptoms, further evaluation and follow-up for COVID-19 diagnosis are required even after a successful operation.
According to our hospital’s emergency surgery guidelines for COVID-19, radiologic findings, RT-PCR findings, and clinical symptoms are the main diagnostic tools for COVID-19. Among the radiologic imaging tools, chest computed tomography (CT) is a highly helpful tool for early infection detection and access to the disease course of COVID-19 pneumonia [8]. Even with suspected COVID-19 symptoms without significant abnormal findings in chest imaging, guidelines for confirmed patients should be followed. All eight mothers were not outpatients of our hospital; however, they were transferred from other hospitals as per the hospital policy. Therefore, the mothers required urgent C-sec before the COVID-19 RT-PCR results were received. HCWs should wear enhanced PPE and the surgery should be performed in a negative pressure operating room as per emergency surgery guidelines for COVID-19 (Fig. 1A). However, there are difficulties in following these guidelines for urgent C-sec cases. First, obtaining the RT-PCR results requires more than 6 h and it is necessary to urgently perform emergency C-sec cases before receiving the results. Second, although chest CT requires a short duration of 5 min, it was not applied to all mothers given the need to avoid the radiation exposure of the fetus. All eight patients were managed according to the guidelines shown in Fig. 1A; therefore, we were required to wear enhanced PPE in all cases. Based on the aforementioned difficulties, we removed the chest CT from the guidelines and we now apply revised emergency C-sec guidelines (Fig. 1B).
After the COVID-19 outbreak in Daegu, our institution was designated for the delivery of suspected or confirmed mothers with COVID-19 with several delivery cases being expected. Therefore, the entire delivery center was converted to a negative pressure environment. To avoid interfering with other elective surgeries, C-sec cases were performed in a separate delivery center from the main operating room. Fortunately, since our hospital was designated for C-sec of COVID-19 confirmed and suspected mother, those without COVID-19 symptoms were not admitted during this period. Given that the delivery center was not originally designed as an operating room, the exact negative pressure could not be measured. Therefore, the smoke test was used to confirm the negative pressure in the C-sec operating room [9].
There are two anesthesia options: general and regional anesthesia. For general anesthesia, intubation should be performed with endotracheal intubation and extubation considered as high-risk aerosol-generating procedures [10]. Therefore, all HCWs, especially anesthesiologists, should wear enhanced PPE with PAPR. In the aerosol state, COVID-19 is viable for > 3 h in case of aerosol transmission [11]. Therefore, operations on suspected patients should be performed in a negative pressure room with the assumption that the aerosolized virus can spread. Moreover, there is a need for sufficient post-intubation or post-extubation time to remove airborne contaminants. According to the Center for Disease Control and Prevention, when the air changes/hour (ACH) is 12 times, 99% airborne-contaminant removal efficiency takes 23 min while 99.9% takes 35 min [12]. The ACH of our hospital is 12–16 times. Consequently, the door is not allowed to open for at least 30 min after extubation, which is informed to all the HCWs participating in the surgery. Given the aforementioned reasons, we preferred regional anesthesia over general anesthesia. For regional anesthesia, the mother wears an N95 mask to minimize the possibility of virus transmission.
Among the seven mothers suspected of COVID-19 infection, six presented with fever; among them, two delivered stillborn babies, two had preterm labor, and two had PROM. Two of the seven suspected patients presented with dyspnea, which improved after child-birth. Dyspnea is common during pregnancy and could occur during severe labor pain [13]. All suspected patients lacked additional post-delivery symptoms and the COVID-19 was negative after several post-surgery hours. Despite the aforementioned results, it is currently difficult to differentially diagnose the presence or absence of COVID-19 even with mild symptoms. Therefore, in cases where COVID-19 results cannot be waited for, strict guidelines for managing the operating room are required. In addition, there have been reports of presymptomatic (silent) patients [14] who were reported by Song et al. [15] to reach about 10% (3 of 28 patients). Moreover, there are guidelines for elective surgery patients in pandemic situations regarding operation room management to distinguish presymptomatic patients from uninfected patients (Fig. 1C).
In conclusion, it is essential to isolate the confirmed patients as per the institutional perioperative COVID-19 infection prevention protocol. These case reports emphasize on the perioperative management guidelines for suspected COVID-19 cases to prevent virus transmission. Therefore, suspected patients with symptoms should be managed using strict guidelines similar to those of confirmed patients.
Notes
Funding Statement
This study was supported by the Research Program of Medicity Daegu Council funded by Daegu Metropolitan City (fund code : COVID19_DM23).
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Jeongmin Oh (Writing – original draft)
Eunju Kim (Conceptualization)
Hyunkyum Kim (Data curation)
Sang-Ah Lee (Methodology)
Kyeong Hee Lee (Resources)
Mi Hyae Yu (Resources)
Jihyun An (Visualization; Writing – review & editing)


