Impact of an ultrasound-guided regional anesthesia workshop on participants' confidence levels and clinical practice
Article information
The use of ultrasound-guided regional anesthesia (UGRA) has increased, leading to a growing demand for UGRA training [1]. Education may be particularly challenging for those already in established practice because educational opportunities are less obvious. In 2009, the American and European Societies of Regional Anesthesia published guidelines for training pathways in UGRA [2]. For practicing anesthesiologists, they recommended workshops consisting of “didactic teaching and hands-on experience [2].” However, there is limited evidence [3] suggesting that these workshops are effective and can impact participants' clinical practice. We aimed to assess if attendance at a UGRA workshop improved confidence in block performance and impacted clinical practice.
Since 2004, the regional anesthesia group at Toronto Western Hospital, University Health Network has conducted semi-annual UGRA workshops. These 2-day workshops consist of didactic lectures, live scanning of models under expert supervision, and needling practice on low fidelity simulators. The course curriculum includes teaching on upper and lower limb blocks, truncal blocks, and neuraxial ultrasound. To assess the impact of the workshop, participants were sent an online survey after completion of two courses in 2018.
The primary outcome assessed with our survey was the change in participants' confidence levels post-workshop. Secondary outcomes included participants' perceptions on whether or not the workshop made a relevant impact on their clinical practice and to identify the important factors, which can increase the use of UGRA in clinical practice.
Of the 99 people who participated in the two workshops, 58 (59%) responded to the follow-up survey, and 34% of the participants stated that they felt confident in performing UGRA blocks prior to attending the workshop, which increased to 66% after the workshop (P < 0.001; McNemar's test) (Fig. 1A). The major reason participants said they were not confident was the lack of needling practice (67%). Other common reasons included inadequate scanning practice (20%) and insufficient knowledge of block procedure (13%). For less experienced participants (defined as having previously performed less than 50 blocks), there was a significant increase in the percentage of participants who felt confident after the workshop. The number of confident participants in the less experienced group rose from 6% before the workshop to 61% after (P < 0.001; McNemar's test) (Fig. 1B). In contrast, more experienced participants (defined as having previously performed more than 50 blocks) showed no change in their confidence levels before and after the workshop (Fig. 1B).
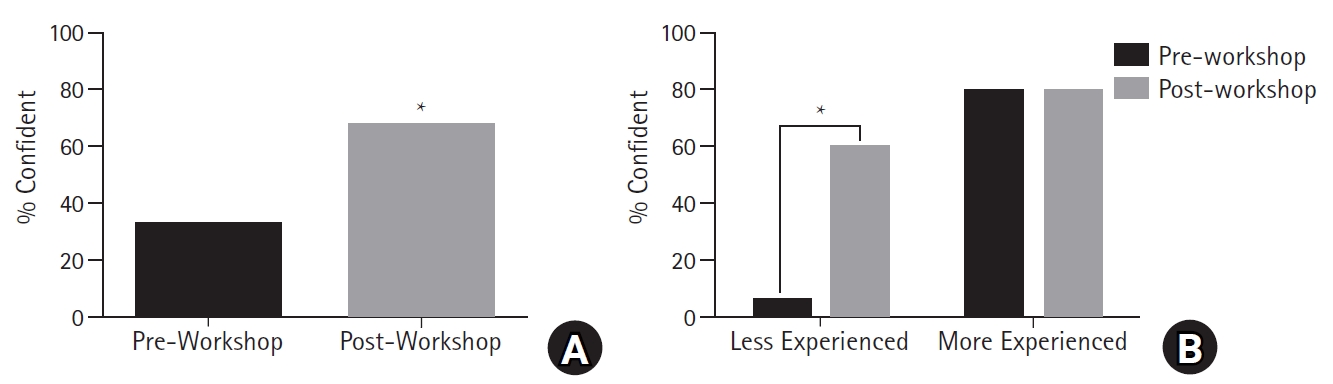
Confidence levels of workshop participants in ultrasound-guided regional anesthesia. (A) Confidence of participants in performing ultrasound-guided regional anesthesia pre- and post-workshop. (B) Confidence of less experienced participants (those who had performed ≤ 50 blocks) versus more experienced participants (those who had performed > 50 blocks) pre- and post-workshop. *P < 0.001.
Most (95%) participants stated that the workshop made a relevant impact on their clinical practice. When asked about the most important factor increasing the use of UGRA in their practice, adequate training, adequate time for performing the UGRA blocks, and more surgical procedures were stated by 33%, 19%, and 13% of the participants, respectively. Other factors included buy-in by surgical colleagues (11%), adequate mentorship (9%), refreshment of skillset (7%), refreshment of knowledge (4%), and adequate equipment (4%).
Results of our survey provided evidence for the training recommendations made by the American and European Societies of Regional Anesthesia [2]. The workshops were effective in improving participants' confidence levels in performing UGRA; however, this was only seen for participants with less experience. A study assessing the impact of an UGRA workshop among anesthesiology residents demonstrated a similar finding [3]. With less previous exposure, it is reasonable that participants with less experience have more to gain. Additionally, most participants stated that the workshop made a relevant impact on their clinical practice. Kim et al. [4] also assessed an UGRA workshop for practicing anesthesiologists, reporting that participants performed more UGRA blocks after the workshop. The subjective findings from our survey offer support that workshop attendance facilitates changes in clinical practice.
Adequate training was the most commonly cited factor increasing the use of UGRA in clinical practice. In a survey by the American Society of Regional Anesthesia and Pain Medicine in 2010, the most frequently cited reason for not practicing UGRA was the lack of training [5]. These findings emphasize on the importance of effective educational tools to facilitate the translation of skills to clinical practice. Few participants stated adequate equipment as a factor increasing their use of UGRA. The study by Kim et al. [4] also demonstrated that available equipment was not a barrier for most practicing anesthesiologists. These findings are in contrast to the 2010 survey, which found that the most difficult challenge to overcome for members was the availability of ultrasound equipment [5]. As such, it is possible that ultrasound equipment is becoming more readily available.
Future work should aim to improve the workshops by investigating the appropriateness of the workshop for physicians with varying degrees of experience. One possibility is to have separate workshops with a more advanced curriculum for trainees with more experience. Another consideration is to make the workshops more flexible in content, catering to the learning needs of the specific participants. In response to our survey, we have started offering advanced UGRA workshops where more complex and novel techniques are taught. The participants are given a chance to choose the blocks that they would like to learn, and each technique is taught via small group learning.
In conclusion, we found support for UGRA workshops targeted at practising physicians. Future work remains to elicit the most effective structure and content of these workshops.
Acknowledgements
The authors would like to thank Rongyu Jin for her help with developing and conducting the survey. Dr. Vincent W.S. Chan has received honorarium from Heron Therapeutics.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Dong An (Formal analysis; Writing – original draft; Writing – review & editing)
Nicholas D. Black (Formal analysis; Writing – original draft; Writing – review & editing)
Sarah Tierney (Conceptualization; Investigation; Methodology; Writing – review & editing)
Vincent W.S. Chan (Conceptualization; Investigation; Methodology; Writing – review & editing)
Ahtsham U. Niazi1 (Conceptualization; Formal analysis; Investigation; Methodology; Supervision; Writing – original draft; Writing – review & editing)
