Effect of transportation method on preoperative anxiety in children: a randomized controlled trial
Article information
Abstract
Background
This study was performed to evaluate the effect of a wagon as a transport vehicle instead of the standard stretcher car to reduce children’s anxiety of separation from parents. The secondary goal was to evaluate whether this anxiolytic effect was related to age.
Methods
We divided 80 children (age 2–7 years) into two groups. The stretcher group was transferred to the operating room on a conventional stretcher car, whereas the wagon group was transferred using a wagon. The level of anxiety was evaluated three times using the Modified Yale Preoperative Anxiety Scale (mYPAS): in the waiting area (T0), in the hallway to the operating room (T1), and before induction of anesthesia (T2).
Results
The mYPAS score was significantly lower in the wagon group (36.7 [31.7, 51.7]) than in the stretcher group (51.7 [36.7, 83.3]) at T1 (P = 0.007). However, there was no difference in the mYPAS score between the two groups at T2 (46.7 [32.5, 54.2] vs. 51.7 [36.7, 75.0], respectively, P = 0.057). The baseline anxiety tended to be lower with increasing age (r = −0.248, P = 0.031). During transportation to the operating room, the increase in the mYPAS score (T1-T0) was greater as the age of children decreased in the stretcher group (r = −0.340, P = 0.034). However, no correlation was observed in the wagon group (r = −0.053, P = 0.756).
Conclusions
The wagon method decreased preoperative anxiety, suggesting that it may be a good alternative for reducing preoperative anxiety in children.
Introduction
In general, children show more severe preoperative anxiety than adults. In addition, children under the age of eight years often show more preoperative anxiety during the process of separation from their parents [1,2]. Preoperative anxiety has been reported to result in adverse outcomes and negative postoperative sequelae such as emotional disturbance, cognitive disturbance, behavioral problems, bad dreams, sleep disturbance, and disobedience [3]. To reduce children’s anxiety, it has been suggested that the parents move together with their children to the operating room or sedative agents should be provided [4].
However, moving to the operating room with parents has some problems. First, parents must be educated to prevent operating room contamination. Second, parents should not appear anxious to avoid influencing their children’s anxiety [5]. Third, parents should also wear surgical suits, which may be not effective in reducing children’s anxiety. The use of sedative drugs can be an effective way to reduce children’s anxiety, but it is difficult to determine the effective dosage because children have a narrow safety margin and a large variation among sedative drugs [6]. Thus, several studies have been conducted to reduce anxiety in children by nonpharmacological methods. Numerous nonpharmacological methods have been investigated, including music [7], clowns [8], toys, comic books [9], and watching videos using smartphones or tablets [10]. Some of these strategies have been reported to reduce preoperative anxiety, with effects equivalent to or better than parental presence or sedative drugs.
Traditional pharmacological and nonpharmacological methods have their own pros and cons. Their effectiveness also depends on the children’s characteristics or hospital conditions. Generally, a patient scheduled to undergo an operation is transferred using a stretcher car, which may be stressful for the patient. Moreover, children may show severe anxiety because of the synergistic effect of separation from their parents. In 1988, it was reported that the use of a pleasant mode of transportation, such as a little red wagon, could keep children calm and distracted during transport to the operating room [11], and this method has been introduced in literatures as a nonpharmacological anxiolytic intervention for children. Until recently, however, this simple method has not been evaluated through clinical trials. Only a very recent study by Liu et al. [12] compared the anxiolytic effect of transport in a children’s toy car to that in a conventional transport vehicle, and favorable results were obtained in children aged 2–5 years. However, there is still limited evidence to support the effect of the transport method on reducing preoperative anxiety among children, and furthermore, it is not clear whether this anxiolytic effect varies according to the age of the children.
The primary goal of this study was to evaluate the effect of a wagon as a transport vehicle instead of the standard stretcher car to reduce children’s anxiety related to separation from their parents. The secondary goal was to evaluate whether this anxiolytic effect was related to age.
Materials and Methods
The study population consisted of 80 children aged 2–7 years, classified as American Society of Anesthesiologists physical status I and scheduled for elective surgery under general anesthesia. After receiving approval by the Institutional Review Board of our hospital (CNUH-2016-185) and registration at clinicaltrials.gov (NCT03018145), the parents of all the children provided informed consent. Children with a history of anesthesia or surgery, with developmental delay, weighing over 34 kg, with severe pain, or who were administered psychotomimetic drugs within 24 h were excluded. From January to April 2017, 80 children scheduled for elective surgery were randomly allocated into one of two groups using a computer-generated method on the day of surgery: one group used a standard transport stretcher (Stryker®; Stryker Medical, USA; Fig. 1A) as a transportation method from the preoperative waiting area to the operating room (stretcher group, n = 40); the other group used a wagon (All Around Canopy Wagon™; Step2, USA; Fig. 1B) instead of a standard stretcher car (wagon group, n = 40). For analysis concerning the age of the children, we allocated the same number of children to the stretcher and wagon groups by computer-generated randomization with a block size of four with stratification for age (2–4 years or 5–7 years).
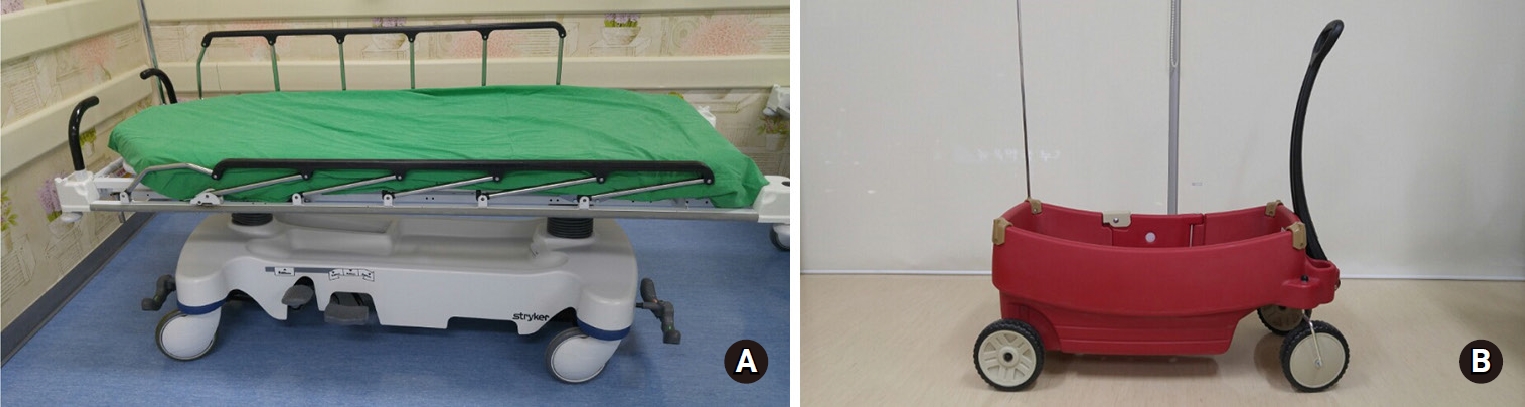
Transporting vehicles. (A) Conventional transport stretcher (Stryker®), (B) Wagon (All around canopy wagonTM).
Each child was evaluated three times by the same anesthesiologist: before separation from his/her parents in the preoperative waiting area (T0), after separation from his/her parents in the hallway of the waiting area to the operating room, immediately before entry into the operating room (T1), and in the operating room before the induction of general anesthesia (T2). An anesthesiologist used the Modified Yale Preoperative Anxiety Scale (mYPAS) to assess the child’s anxiety in five domains of behavior: activity, emotional expression, state of arousal, vocalization, and the presence of a parent [13]. In this method, each domain is rated from 1 to 4 except for the vocalization domain, which is rated from 1 to 6, with higher scores indicating a greater level of anxiety. The total mYPAS score was calculated by dividing each domain’s rating by its highest possible rating. Parents were not allowed to enter the operating room, and so accompanied the child only in the preoperative waiting area. After separation from the parents, the interaction with the parents was assessed by slightly modifying the original components of the ‘use of parent’ because of parental absence.
Before the surgery, each child answered the EAS questionnaire (The Emotionality, Activity, and Sociability Temperament Survey for Children: Parental Ratings) to evaluate the child’s activity and sociability temperament. All children had a fasting time of over 6 h and did not take any premedication. After arrival at the preoperative waiting area with parents, the children’s mYPAS scores were assessed by an anesthesiologist (T0). The children were moved to the transport vehicle and then allowed to stay with parents for 2–3 min to adapt to the vehicle. After separation from the parents, the children were transferred to the assigned operating room through the hallway with the anesthesiologist, surgeon, and nurse for safety. At the end of the hallway, the anesthesiologist assessed the mYPAS scores before entry into the operating room (T1). In the operating room, the children were moved to the operating table for general anesthesia, and then the anesthesiologist assessed the mYPAS score again (T2).
Statistical analysis
The sample size calculation for the present study was based on the difference in the mYPAS after separation from the parents (T0 to T1). According to the results of a pilot study (n = 8 in each group, total n = 16), the mean difference was 10 and the standard deviation was 15 in each group (effect size = 0.6666667). With an estimated sample size for 80% power with a set α of 0.05 for the Student’s t test, a total sample size of 74 was calculated (n = 37 per group). We assigned 40 children per group to account for potential dropout. All statistical analyses were performed using statistical software (IBM SPSS Statistics version 20; IBM Corp., USA). Continuous variables were verified for normal distribution using the Kolmogorov-Smirnov test. The children’s age, weight, and EAS score were analyzed using an independent t test, and the results are presented as the mean ± SD. Differences in the mYPAS scores between groups at each time point were analyzed using the nonparametric Mann-Whitney test and are presented as the medians (1Q, 3Q). Within-group mYPAS changes were analyzed using Wilcoxon’s signed-rank test. Categorical data were analyzed using Pearson’s chi-square test. The relationships of children’s ages to mYPAS scores or mYPAS score changes were analyzed by Spearman correlation analysis. A P value < 0.05 was deemed to indicate statistical significance.
Results
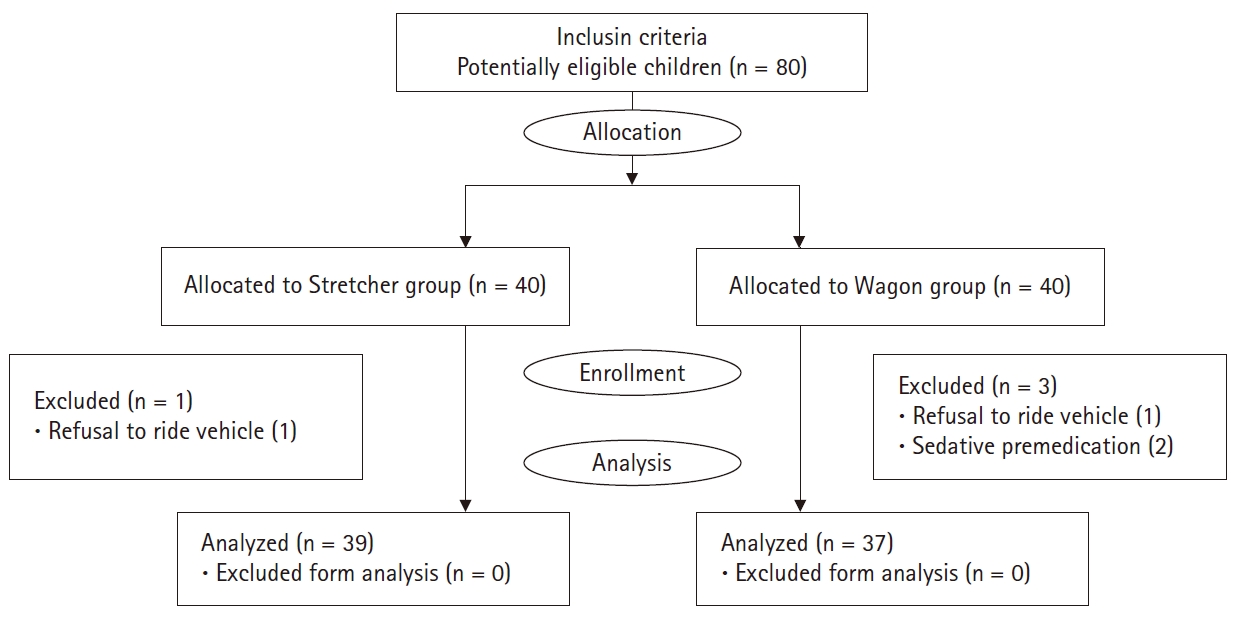
The final data were collected from 76 children: 39 forming the conventional standard group (Stretcher group), and 37 forming the intervention group (Wagon group). Two children refused to ride the wagon or stretcher car, and two children took sedative premedication (Fig. 2.).
There were no significant differences in demographic variables or EAS questionnaire ratings between the groups, and there was no correlation between the EAS rating and mYPAS score (Table 1).
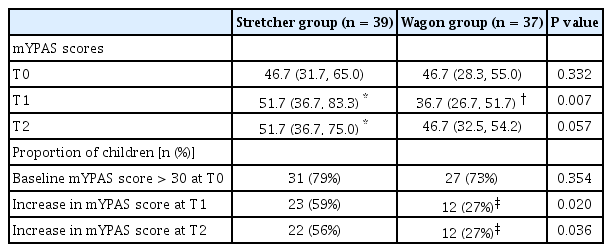
In the preoperative waiting area (T0), both groups showed similar mYPAS scores. In the Stretcher group, there was a significant increase in mYPAS during transportation after separation from parents (T1–T0, P = 0.001) and before induction of anesthesia (T2–T0, P = 0.003) compared with that in the waiting area (T0). The mYPAS score was significantly lower in the Wagon group during transportation than in the Stretcher group (T1, P = 0.007). However, use of the wagon did not prevent an increase in mYPAS scores before induction of anesthesia (Table 2).
Fifty-eight children (31 in the Stretcher group and 27 in the Wagon group) showed baseline anxiety (mYPAS scores > 30). The percentage of children with an increase in mYPAS from baseline was significantly higher in the Stretcher group than the Wagon group (Table 2).
Children’s age was weakly related to the baseline mYPAS score, with the baseline anxiety level tending to be lower with increasing age (r = −0.248, P = 0.031). During transportation to the operating room, relative increases in the mYPAS score from baseline (T1–T0) were negatively correlated with the age of children in the stretcher group (r = −0.340, P = 0.034), indicating that younger children tended to be more anxious in the Stretcher group. However, no such correlation was observed in the Wagon group (r = −0.053, P = 0.756) (Fig. 3).
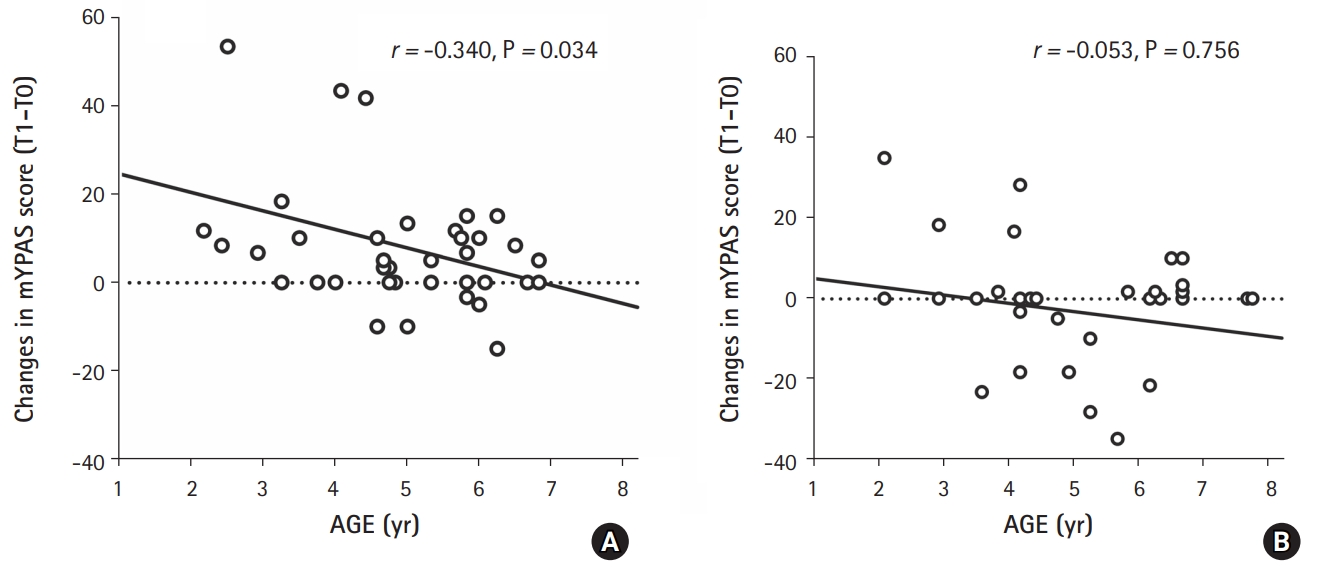
Relation of children’s age to mYPAS score changes during the transportation to the operating room (T1-T0). (A) Stretcher group, (B) Wagon group. mYPAS: Modified Yale Preoperative Anxiety Scale. T0: in the waiting area with parents; T1: on the transporting vehicle after separation from parents.
Subsequently, the mYPAS scores were compared between children aged 2–4 years and 5–7 years according to the transport method. In younger children (2–4 years), the mYPAS scores at T1 were significantly lower in the Wagon group (50.0 [23.3, 68.3]; n = 19) compared with the Stretcher group (83.3 [36.7, 95.0]; n = 19) (P = 0.018), and the mYPAS scores at T2 were also significantly lower in the Wagon group (46.7 [23.3, 53.3]) compared with the Stretcher group (73.3 [46.7, 96.7]) (P = 0.017). In older children (5–7 years), the mYPAS scores at T1 was lower in the Wagon group (28.3 [26.7, 37.9]; n = 18) than in the Stretcher group (50.0 [29.2, 55.0]; n = 20) (weak significance, P = 0.046), and the mYPAS scores at T2 were similar in both groups (44.1 [35.8, 55.4] in the Wagon group vs. 45.8 [36.7, 58.2] in the Stretcher group, P = 0.851).
Discussion
In the present study, we measured children’s anxiety using the mYPAS, ranging from 23.33 to 100. It is well known that mYPAS has strong interrater reliability [14]. A cutoff value of 30 is regarded as anxiety. In the present study, 76% of children showed anxiety (mYPAS > 30) even though they were with their parents. These results are comparable with those of a previous study that reported 80.5% of children had anxiety [15]. In that study, more than 60% of children showed an increase in mYPAS score after separation from their parents. This result was similar to ours in the Stretcher group (59%).
In the Wagon group, the median mYPAS score of 36.7 after separation from their parents was similar to that in another study (33.4) in which children came into the operating room together with their parents [16]. In addition, the proportion of children with increased anxiety compared to baseline was significantly lower in the Wagon group until induction of anesthesia. These results suggest that the wagon can play a role in the management of preoperative anxiety in children, comparable to other nonpharmacological methods such as parental presence or video distraction [16].
The anxiety-reducing effect of the wagon may be related to its greater familiarity to children compared to the stretcher car, and it may distract the children similar to watching a video or playing with toys. It also feels like going on a ride and will be fun for children. In addition, children mostly lie down in the stretcher car to reduce the risk of falling, but they can sit up in the wagon, and so children can freely see their surroundings and feel less restrained.
In general, one of the most commonly used methods to reduce children’s anxiety is oral or parenteral sedative medication [4,17,18]. However, sedative drugs sometimes have several undesirable effects, including respiratory depression, hypotension, seizure-like activity, and paradoxical reactions [18,19]. Moreover, it is difficult to determine the effective dosage because children have a narrow safety margin and a large variation among sedative drugs [6]. According to previous studies, a combined therapy with nonpharmacological and pharmacological interventions was more effective than medication alone [8,10]. The wagon as a transport vehicle can be used in combination with conventional pharmacological and nonpharmacological methods.
Previous studies showed that younger children have more anxiety than older children [20,21]. We allocated children to both younger and older groups for analysis related to the children’s ages. According to our protocol, we included children aged between 2 and 7 years; because the median age was 5 years, we divided the children into a younger subgroup aged 2.0–4.9 years and an older subgroup aged 5.0–7.9 years. In our study population (2.0–7.9 years), younger children showed greater baseline anxiety than older children, as shown in previous studies [8,20]. This result suggests that older children are more likely to endure or overcome stress than younger children.
In the present study, change in anxiety after separation from parents decreased as the children’s age increased in the Stretcher group. The intensity of separation anxiety is known to peak at around one year of age, and then declines with age, largely because of increasing cognitive abilities [22]. Therefore, the intensity of separation anxiety in younger children is usually higher than that in older children. In the Wagon group, however, children’s age was not related to change in anxiety. These results suggest that use of the wagon may have offset the increase in anxiety in younger children that was observed in the stretcher group. Thus, use of the wagon may be expected to be more effective in younger children than in older children.
However, before induction of anesthesia (T2), the wagon did not prevent increases in the mYPAS score, although the proportion of children in whom the mYPAS score increased at baseline (T0) was lower in the Wagon group than in the Stretcher group. This may have been because preoperative anxiety in older children often originates from the fear of surgery rather than the distress of separation [10]. Similarly, Kain et al. [23] suggested that interactive music therapy may be useful in alleviating preoperative anxiety due to separation from parents and entrance to the operating room; however, music therapy did not appear to alleviate children’s anxiety at induction of anesthesia.
A recent randomized controlled study demonstrated that riding in a toy car significantly reduced preoperative anxiety compared with riding on a stretcher among children with or without premedication, which was consistent with our results [12]. Interestingly, the anxiolytic effect of riding in a toy car was similar to that of oral midazolam, even just before anesthesia induction in the previous study [12]. These favorable results may have been due to the age range of the study population (2–5 years), which corresponds to the younger children in the present study. As suggested above, the anxiolytic effect of the transport method may be affected by the children’s age, and it would have a greater effect in younger children.
The present study had several limitations. First, our results showed higher baseline mYPAS scores than those reported in previous studies [15,16]. This may have been due to the lack of sedative premedications, which were administered in other studies. Here, we wanted to eliminate the effects of drugs. Similarly, another study in which children did not take premedication in the waiting area showed a higher mYPAS score [10]. Second, blinding was impossible in this study because the transportation vehicles were visible to the investigators, and therefore observer bias may have influenced assessment of anxiety levels. Third, we were unable to calculate the ‘use of parents’ item of the mYPAS accurately at the T2 time point because of parental absence. Therefore, the components of the use of parent may have affected the psychometric integrity of the mYPAS.
In summary, most children scheduled for surgery showed anxiety during transportation to the operating room and before the induction of anesthesia. Younger children showed more anxiety than older children. The wagon as a transport method decreased this anxiety compared with the standard stretcher car. This result suggests that wagons may be a good alternative to reduce children’s preoperative anxiety. In addition, the wagon also has a number of advantages: it is a very simple change in transportation and can be used in combination with pharmacological or other nonpharmacological methods.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Sun-Hong Park (Data curation; Investigation; Writing – original draft; Writing – review & editing)
Sanghee Park (Data curation; Formal analysis; Writing – review & editing)
Seongheon Lee (Conceptualization; Formal analysis; Writing – review & editing)
Jeong Il Choi (Methodology; Supervision; Writing – review & editing)
Hong-Beom Bae (Methodology; Supervision; Writing – review & editing)
Youngwook You (Data curation; Investigation; Writing – review & editing)
Seongtae Jeong (Conceptualization; Formal analysis; Methodology; Writing – original draft; Writing – review & editing)