Simply modified percutaneous tracheostomy using the Cook® Ciaglia Blue Rhino™: a case series
Article information
Abstract
When first introduced, percutaneous dilatational tracheostomy (PDT) was performed using a bronchoscope. The bronchoscope itself, however, has several disadvantages, including interruption of ventilation. Modifications of the standard PDT technique have suggested that PDT can be safely performed without a bronchoscope. However, the safety of these modifications is unclear and many modifications have yet to be widely adopted. This study retrospectively evaluated the safety of a simplified PDT technique using the Cook® Ciaglia Blue Rhino™ in 186 patients. After confirming the underlying structures by palpation, PDT was performed without a bronchoscope or blunt dissection, 2.0 cm below the cricothyroid membrane. Ultrasonography was used only when palpation was difficult. Except for bleeding in three patients with coagulopathy, none of the patients experienced any early or late complications, and there were no deaths related to PDT. These findings confirm that PDT can be safely performed using a simplified technique, which may be useful in situations with limited equipment and medical personnel.
Bedside percutaneous dilatational tracheostomy (PDT) has been shown to be a safe and cost-effective procedure in the intensive care unit (ICU) [1]. Although several PDT techniques have been developed [234], use of a fiberoptic bronchoscope (FOB) has been recommended, regardless of the PDT method, to ensure proper positioning and avoid potentially severe complications. However, the FOB itself has complications, such as prolonged ventilation interruption [56] and the need for additional medical personnel and equipment [5]. PDT techniques have therefore been modified to avoid the routine use of a bronchoscope while allowing PDT to be performed more safely and efficiently. Some of these modifications, which have included technical alterations [7] and the simplification of previous techniques [8910], have been shown to be efficient and safe. However, the safety of modifications that omit the bronchoscope remains unclear and many have yet to be widely adopted. Use of the Cook® Ciaglia Blue Rhino™ technique for PDT has been shown to be safe without a bronchoscope. Rather than use a bronchoscope, this approach utilizes direct palpation of the tracheal rings with or without blunt dissection of subcutaneous tissues [158910]. The present study evaluated the safety of a simplified technique of PDT without the use of either a bronchoscope or blunt dissection. The results confirmed that the simplified Cook® Ciaglia Blue Rhino™ technique is relatively safe.
Case Report
This retrospective study was approved by the Institutional Review Board of our hospital (2014-09-037). Between November 2011 and October 2014, 245 patients in the ICU underwent bedside PDT with a Ciaglia Blue Rhino® percutaneous tracheostomy set (Cook Medical, Bloomington, IN, USA) due to prolonged endotracheal tube insertion. PDT was not performed in patients aged under 18 years, those with any pulsation palpated over the tracheostomy site, patients with a history of surgery or radiotherapy in the cervical region, and those with coagulopathy (increased prothrombin time, INR > 2). The first four procedures were performed by two physicians and one nurse using the standard technique, with one physician operating the bronchoscope while the other performed PDT. The next 55 procedures were performed by one physician and one nurse, with the physician using the bronchoscope only to confirm and evaluate the proper depth for the endotracheal tube before performing PDT using the simplified method described below. The remaining 186 procedures were performed using the simplified technique after repositioning the endotracheal tube at the predetermined depth (17 cm for males and 15 cm for females at the incisor). The demographic characteristics of the 186 patients are shown in Table 1.
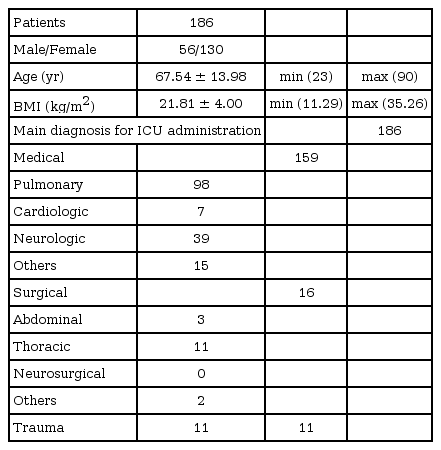
Demographic Data and Stratification of Patients Who Underwent Percutaneous Dilatational Tracheostomy
All PDTs were performed by a single physician and one nurse, both of whom fully understood the entire procedure. The nurse administered sedatives and analgesics, as well as repositioning the endotracheal tube. Except for patients with limited neck extension, a small pillow was placed under the patient's shoulders to slightly extend the neck. Transverse markings were made at the cricothyroid membrane and 2.0 cm toward the sternal notch (Fig. 1A). A 1.5 cm vertical mark was also made in the midline of the trachea by holding the trachea between the thumb and index finger. The middle of the vertical mark intersected with the transverse mark 2.0 cm below the cricothyroid membrane (Fig. 1B). If the cricothyroid membrane could not be palpated, ultrasonography was used to identify the anatomic structures. The cricoid cartilage and tracheal rings were identified by placing the linear probe 45 degrees from the sagittal plane, and the area between the second and third tracheal rings was marked with a skin marker (Figs. 1E and 1F). The linear probe was positioned vertical to the trachea to confirm its midline (Figs. 1G and 1H). After all anatomical markings were made, FIO2 was increased to 1.0, and 5–7 cmH2O positive end-expiratory pressure was applied to all patients receiving ventilator care. In patients who were receiving oxygen supplementation via a Hydro-Trach T-piece, oxygen flow was increased to 10 L/min. The PDT site was disinfected with povidone iodine solution and a sterile drape was used before subcutaneously injecting 2% lidocaine. A vertical skin incision (1.5 cm) was made through the midline vertical marking, and the endotracheal tube was withdrawn until the tube depth was 17 cm for males and 15 cm for females (Fig. 1C). The trachea was punctured at the middle of the incision (Fig. 1D) using a 5 cm-introducer needle, included in the Cook® Ciaglia Blue Rhino™ set, and proper needle position was confirmed by air regurgitation with a syringe containing normal saline. A guide wire was inserted after slightly tilting the needle caudally. The remaining PDT procedure was performed using the previous standard method with a #7 tracheostomy tube (Twist, Tracoe, Germany). A #8 tube was used only in patients in whom bronchoscopic lavage was planned (about 10 patients).
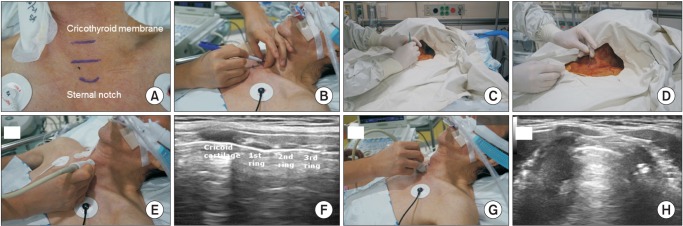
Simplified technique of percutaneous dilatational tracheostomy (PDT). (A) The underlying anatomical landmarks were marked with a skin pen. The incision point was 1-finger breadth (about 2.0 cm) below the cricothyroid membrane. (B) The trachea was placed between the thumb and index finger. A vertical line was drawn in the middle of the trachea at the point of incision. (C) After making a vertical incision (1.5 cm), a nurse withdrew the endotracheal tube (17 cm at the upper incisor in males, 15 cm in females). (D) A 15 gauge, 5 cm introducer needle was used for puncture and confirmed via air aspiration with a saline containing syringe. (E, F) When anatomical landmarks could not be easily palpated, ultrasonography was used to confirm the second and third tracheal rings. (G, H) Ultrasonographic confirmation of the vertical line being in the middle of the trachea.
The most frequent acute complication was bleeding, which was observed in three patients. However, all 3 patients were receiving either extracorporeal membrane oxygenation or continuous renal replacement therapy and had an abnormal coagulation status. Bleeding in all three was well controlled by bipolar electrocautery in the ICU. Long-term (> 7 days) follow-up in 150 patients showed no late complications and no deaths related to PDT.
Discussion
Although use of a FOB during PDT has been recommended for precise positioning and to avoid complications, bronchoscopy itself can cause complications [56]. Also, an additional physician is required and additional costs may result from damage to the FOB. Thus, several studies have assessed the safety of PDT without a FOB, including technical modifications [7] and simplified procedures [8910]. Direct visualization of the larynx with a laryngoscope confirmed adequate endotracheal tube repositioning depth prior to PDT, while direct or indirect palpation of the trachea confirmed the proper tracheostomy site. Direct palpation of the trachea is enabled by blunt subcutaneous dissection [1510]. Although these simplified techniques have been shown to be safe, they have not been widely adopted.
This study assessed the safety of a simplified PDT technique using the Ciaglia Blue Rhino, by repositioning the existing endotracheal tube at a pre-determined depth and determining proper PDT site by superficial palpation. Early complications of PDT include loss of airway, bleeding, conversion to open tracheostomy and death, with later complications including tracheostomy occlusion, tracheal stenosis and granulation. A retrospective study comparing early and late complications of PDT, with or without FOB assistance, using the Ciaglia Blue Rhino™ kit in 243 patients found no between group differences in early and late complications, but one patient experienced cardiac arrest during the use of a FOB due to loss of airway [5]. In this study, only 3 patients experienced bleeding after PDT, with all 3 receiving extracorporeal membrane oxygenation or continuous renal replacement therapy and having an abnormal coagulation status. No patient in this study experienced late complications. However, we were unable to assess long-term complications in patients who were transferred to other facilities.
Precise positioning is critical when performing PDT [1112], thus requiring use of a FOB or direct palpation of the trachea. The biggest disadvantage of our modified percutaneous method was the inability to confirm the PDT site. In five patients, where the underlying structures could not be adequately palpated, ultrasonography was used to identify the underlying anatomy. Another disadvantage is the lack of precise endotracheal tube repositioning, which can be achieved with a laryngoscope [89]. Although a FOB was used to determine the proper tube depth in 55 patients, the needle and guidewire entered the Murphy eye of the tube twice. PDT was successfully performed by retracting the tube an additional 1–2 cm in both cases. Although none of these patients experienced endotracheal cuff failure due to needle puncture, accidental cuff puncture may occur. Moreover, in contrast to subcutaneous dissection, physicians using our modified technique may be unable to identify vessels between the skin and trachea. Ultrasonography, which was used when anatomical structures were not readily identifiable, also has the advantage of screening such blood vessels.
Since all PDTs were performed at a single center by two physicians, and the proper endotracheal tube depth was evaluated in a Korean population, it may be difficult to generalize the safety of our simplified technique. Another limitation was the absence of patients in which PDT is believed to be difficult, such as patients with severe obesity. Although studies have suggested that PDT is safe in obese patients, use of additional equipment, such as a FOB or ultrasonograph, has been recommended [1131415]. We have not performed PDT in morbidly obese patients who may also require extra-long tracheostomy tubes. Currently, therefore, a FOB should be used when performing PDT in difficult situations, such as in patients with morbid obesity, anatomic alterations or neck stiffness.
In conclusion, our results show that PDT with the Ciaglia Blue Rhino technique can be safely performed without a bronchoscope and blunt dissection. This simplified technique is a relatively safe procedure that can be especially useful in situations of limited equipment and medical personnel.
Acknowledgments
The authors thank all medical personals in the ICU (Chungnam National University Hospital) for providing care for the patients included in this study. No funds are involved in this study.
Notes
It was presented IARS annual meeting, May 2014, The Fairmont Queen Elizabeth, Montreal, Canada.
