A pillow of 8 cm height did not improve laryngeal view and alignment of airway axes but increased anesthesiologist discomfort compared to a pillow of 4 cm height during tracheal intubation in adult patients
Article information
Abstract
Background
Neck flexion by head elevation using an 8 to 10 cm thick pillow and head extension has been suggested to align the laryngeal, pharyngeal and oral axis and facilitate tracheal intubation. Presently, the laryngeal view and discomfort for tracheal intubation were evaluated according to two different degrees of head elevation in adult patients.
Methods
This prospective randomized, controlled study included 50 adult patients aged 18 to 90 years. After induction of anesthesia, the Cormack Lehane grade was evaluated in 25 patients using a direct laryngoscope while the patient's head was elevated with a 4 cm pillow (4 cm group) and then an 8 cm pillow (8 cm group). In the other 25 patients, the grades were evaluated in the opposite sequence and tracheal intubation was performed. The success rate and anesthesiologist's discomfort score for tracheal intubation, and laryngeal, pharyngeal and oral axes were assessed.
Results
There were no differences in the laryngeal view and success rate for tracheal intubation between the two groups. The discomfort score during tracheal intubation was higher in the 8 cm group when the patient's head was elevated 4 cm first and then 8 cm. The alignment of laryngeal, pharyngeal and oral axes were not different between the two degrees of head elevation.
Conclusions
A pillow of 8 cm height did not improve laryngeal view and alignment of airway axes but increased the anesthesiologist discomfort, compared to a pillow of 4 cm height, during tracheal intubation in adult patients.
Introduction
The "sniffing position" in which the neck is flexed and head is extended by means of a pillow is commonly used during conventional tracheal intubation with direct laryngoscopy [12]. This position eases tracheal intubation because the laryngeal, pharyngeal and oral axes are positioned in almost a straight line [34]. Elevation of the patient's head 8 to 10 cm with pads under the occiput, with the shoulder remaining on the table, and extension of the head at the atlanto-occipital joint may help align the laryngeal, pharyngeal and oral axes such that the passage and line of vision from the lips to the glottic opening are nearly a straight line [56]. But, the suggestion to use a pad with a height of 8 to 10 cm is not based on clinical investigation.
Clinical studies have evaluated the effect of head and neck positions including a back-up position of 25 degrees [7] or neutral, flexion or extension [8] on the laryngeal view during endotracheal tube insertion. The laryngeal view was assessed using head positions not used commonly in clinical practice. Furthermore, the laryngeal view is not the only factor for successful intubation and the sniffing position has been used mostly for tracheal intubation.
In the present study, tracheal intubation was investigated using different head elevations achieved using a pillow height of 4 cm or 8 cm in the sniffing position. The primary outcome variable was laryngeal view and the secondary outcome variable was discomfort score of anesthesiologist as an index of ease of insertion.
Materials and Methods
Patients and protocol
The Institutional Review Board of our center approved this study. Written informed consent was obtained from all the patients. This randomized controlled trial was registered at clinicalTrials.gov. Fifty adult patients (age range 18–90 years; American Society of Anesthesiologists [ASA] physical status I-II) scheduled for minor surgery (endoscopic sinus surgery or total thyroidectomy) were enrolled. Patients were excluded from this study if they had upper respiratory infection symptoms, limited mouth opening, teeth problems, congenital heart disease, difficult airway (modified Mallampati classification 3 or 4), cardiorespiratory disease or were at risk of aspiration. Patients were randomly assigned to one of two sequences prior to anesthesia induction. Sequence I involved the use a 4 cm pillow first followed by an 8 cm pillow. Sequence II involved a an 8 cm pillow first followed by a 4 cm pillow. The allocation sequence was generated using a computer program (www.randomizer.org). The laryngeal view was evaluated two times using both pillow heights in each patient to decrease interpatient variation.
No premedication was used. A standard anesthesia protocol was used. Monitoring was applied before anesthetic induction and included an electrocardiograph, pulse oximeter, gas analyzer, and noninvasive blood pressure monitor. The patient's head was placed on a pillow that was 4 cm in height (4 cm group) or 8 cm in height (8 cm group) while the patient was supine and tracheal intubation was performed in the sniffing position. Anesthesia was induced with propofol (1–2 mg/kg) and inhalation of 6–8 vol% sevoflurane. Neuromuscular blockade was achieved with rocuronium (0.6 mg/kg). Anesthesia was maintained using 1.5–2.5 vol% of sevoflurane in 50% O2 and air. An intravenous injection of alfentanil 100–200 ug was administered based on the anesthesiologist's decision.
A 7.0 and 7.5 plain endotracheal tube was used for female and male patients, respectively. Mean blood pressure and heart rate were recorded 1 minute before and 1 minute after tracheal intubation. All tracheal intubations were performed by anesthesiology residents with experience in tracheal intubations in more than 60 adult patients per month for more than 6 months. Before induction of anesthesia, the height of the operating table was adjusted to place the patient's forehead at the anesthesiologist's xiphoid process [5]. Tracheal intubation was performed in sniffing position. The laryngeal view was evaluated using a direct laryngoscope while each patient was placed on the two heights of pillows in sequence. The laryngeal view was graded as follows; 1, complete visualization of the vocal cords; 2, visualization of the inferior portion of the glottis; 3, visualization of only the epiglottis; and 4, non-visualization of the epiglottis. The anesthesiologist recorded the degree of discomfort (1 = no discomfort, 2 = mild discomfort, 3 = moderate discomfort, and 4 = severe discomfort) for mask ventilation and tracheal intubation for the two head elevation heights in each patient following completion of anesthesia induction.
An anesthesiology resident who was not aware of the study details photographed the right side of patient while the endotracheal tube was inserted through the oral cavity for tracheal intubation. Two photographs were taken for each patient while the head was sequentially placed on the different pillows. The laryngeal, pharyngeal and oral axes were measured using a protractor from the photographs by three anesthesiologists who were blinded to the study. The laryngeal airway axis was an imaginary midline of neck parallel to the long axis of patient's neck. The pharyngeal axis was an imaginary line from the end of the laryngeal axis to the edge of the eye angle. The oral axis was a perpendicular midline to the imaginary line between the upper and lower lip. The angles from horizontal line to axes were measured and compared. The angular difference of adjacent two axes from horizon was considered as an alignment between the two axes. A less angular difference (pharyngeal axis - laryngeal axis, oral axis - pharyngeal axis) was considered to represent a greater alignment of two adjacent airway axes (Fig. 1).

The airway axes, laryngeal axis (LA): an imaginary midline of neck parallel to the long axis of patient's neck, pharyngeal axis (PA): an imaginary line from the end of the laryngeal axis to the edge of the eye angle and oral axis (OA): an imaginary midline perpendicular to the line between the upper and lower lip.
Airway pressure and end-tidal CO2 concentration were monitored. If insertion failed after two attempts using a same height of a pillow, tracheal intubation was performed using a different height of a pillow in two times. If the trial failed after four attempts, the study was stopped and tracheal intubation was performed using a laryngoscope with a flexible tip or a video laryngoscope. The number of attempts was recorded. The ease of intubation was assessed according to laryngeal view, success rate, and discomfort score. Mask ventilation was not performed between the intubation trials unless the SpO2 decreased by less than 90%.
Sample size analysis
The sample size required was estimated from a similar study [9] in which the Cormack Lehane grade of patients in the control group (sniffing position) was 3 and 2 in patients with head and neck elevation beyond the sniffing position (Cormack Lehane grade difference of 1 was regarded as 33% improvement as it ranges from 1 to 4). When a difference of 33% was accepted, 44 patients per group were required for a two-tailed α error of 5% and a β error of 20%. Six patients were added to each group to compensate for the possible loss of data. As the two heights of pillows were used and evaluated consecutively for each patient, 25 patients in each group were needed.
Statistical analysis
Continuous variables were expressed as the mean (standard deviation) whereas categorical variables were presented as absolute values. Continuous variables were compared using the t-test following normalization test (interincisor distance, thyromental distance, neck circumference, duration for intubation and axes). Categorical variables were compared using the Pearson chi-square test (gender, ASA score, laryngeal view, and discomfort score) or the Fisher's exact test (Mallampati class). A P value of < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
The study was completed in all patients and all data were included for the statistical analyses. There were no differences in patient characteristics between the two groups (Table 1). There were no differences in anesthesiology resident's gender (M/F, 21/4, 19/6, P = 0.363) and grade (15/8/2/0, 10/10/3/2, P = 0.331) between the 4 cm group and 8 cm group, respectively.
The laryngeal view and number of trials during tracheal intubation were not different between the two groups (Table 2). The discomfort score during tracheal intubation was higher in the 8 cm group that was performed in sequence I (Table 2). The objective measured angles from horizontal line to laryngeal, pharyngeal and oral axes were higher in the 8 cm group than 4 cm group, but the angular differences between the two adjacent axes were not different between the two groups (Table 3).
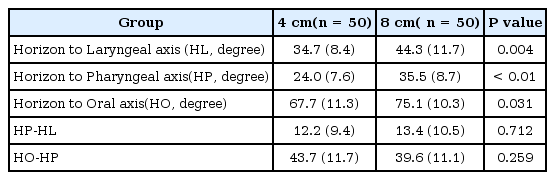
Objective Measured Angle from Horizontal Line to Airway Axes and Angular Differences during Tracheal Intubation
In the 8 cm group, one patient failed to be intubated after two attempts with the 8 cm pillow, with intubation being successful on the first attempt using the 4 cm pillow. For another patient in the 8 cm group, intubation was successful on the second attempt. In the remaining 48 patients, the tracheal intubations were successful on the first attempt.
Discussion
The present study compared the laryngeal view and anesthesiologist's discomfort score during mask ventilation and tracheal intubation according to two head elevations.
The anesthesiologists reported that the limited head extension in the 8 cm group made it harder to open the patient's mouth and insert the laryngoscope into the oral cavity, as the oral axis was near vertical. This might have contributed to the higher discomfort score during tracheal intubation in the 8 cm group. The success rate of tracheal intubation was not different between the two groups as expected because most of the anesthesiologists would exert their maximum effort to secure the airway. The efforts might have contributed to the higher discomfort score for tracheal intubation in the 8 cm group.
The sniffing position has been recommended as a standard for tracheal intubation in the operating room, as the alignment of the laryngeal, pharyngeal and oral axes is facilitated and permitting successful direct laryngoscopy [1234]. The recommendation was not based on scientific clinical studies.
In 80 healthy awake adults, magnetic resonance imaging (MRI) was performed in the neutral, simple extension and sniffing head position to measure the laryngeal, pharyngeal and oral axes, line of vision and angular differences between three axes were [8]. The authors reported that anatomic alignment of the three axes was impossible to achieve in the three positions and no significant differences between angles observed in simple extension and sniffing position.
A clinical study to find the optimal pillow height for the best direct laryngoscopic view was performed without a pillow, and using 3, 6 and 9 cm thick pillows in 50 patients using an integrated video system [10]. They recommended a 9 cm pillow to improve the laryngeal view. The evaluation of the laryngeal view was different from that of the present study; as well, the prior authors did not assess anesthesiologist's discomfort during tracheal intubation.
Improved laryngeal view does not mean facilitated intubation and decreased discomfort of anesthesiologist during tracheal intubation. The pillow height that provides both the comparable laryngeal view and appropriate degree of head extension to open the mouth easily is recommended for tracheal intubation. In the present study, the thinner pillow (4 cm) is recommended versus the thicker pillow (8 cm) as the discomfort of an anesthesiologist during tracheal intubation was lower using the 4 cm pillow. If a certain degree of head elevation provided better laryngeal view only by extreme effort of anesthesiologist to extend the head and open the patient's mouth, it would not be recommendable.
In seven human cadavers, the laryngeal view was measured using a direct laryngoscopy video system and the percentage of glottis opening (POGO) score with a straight laryngoscope blade by progressively increasing head elevation with neck flexion from the head lying as possible [11]. The authors reported that as the head elevation and neck flexion increased, the POGO score improved. The study measured the laryngeal view according to the degree of head elevation but did not assess the anesthesiologist's discomfort score. With the maximum height of a pillow, the head can be elevated maximally, but the degree of head elevation would be limited. The pillow height that improves laryngeal view without limitation in the head extension would be appropriate and recommendable for the tracheal intubation.
Two studies [1213] investigated the ideal head position that provide a good laryngeal view using MRI or a video view system.
The authors reported more objective information but did not assess anesthesiologist's discomfort during tracheal intubation. In the present study, the degree of head elevation that provided comparable laryngeal view and less discomfort for tracheal intubation was the appropriate position, rather than the head elevation that gives best laryngeal view.
There are several limitations in the study. There is no standard for pillow height. The two heights of pillows were selected as they are used commonly in our hospital and are commercially available. Secondly, there are no approved definitions concerning the laryngeal, pharyngeal and oral axes, and it is unpractical to use MRI on every patient to determine axes more objectively. In the present study, the axes were defined according to the authors' decision. Thirdly, the results of the present study are difficult to apply to patients who have difficult airways as the Mallampatti class of the patients in this study were 1-2. Lastly, obesity is one of the causes of difficult airway. Body mass index was not measured.
In conclusion, with the higher degree of head elevation, the laryngeal view and alignment of airway axes were not improved, but anesthesiologist's discomfort was worsened during tracheal intubation in adult patients.


