Risk factors associated with outcomes of hip fracture surgery in elderly patients
Article information
Abstract
Background
Hip fracture surgery on elderly patients is associated with a high incidence of morbidity and mortality. The aim of this study is to identify the risk factors related to the postoperative mortality and complications following hip fracture surgery on elderly patients.
Methods
In this retrospective study, the medical records of elderly patients (aged 65 years or older) who underwent hip fracture surgery from January 2011 to June 2014 were reviewed. A total of 464 patients were involved. Demographic data of the patients, American Society of Anesthesiologists physical status, preoperative comorbidities, type and duration of anesthesia and type of surgery were collected. Factors related to postoperative mortality and complications; as well as to intensive care unit admission were analyzed using logistic regression.
Results
The incidence of postoperative mortality, cardiovascular complications, respiratory complications and intensive care unit (ICU) admission were 1.7, 4.7, 19.6 and 7.1%, respectively. Postoperative mortality was associated with preoperative respiratory comorbidities, postoperative cardiovascular complications (P < 0.05). Postoperative cardiovascular complications were related to frequent intraoperative hypotension (P <0.05). Postoperative respiratory complications were related to age, preoperative renal failure, neurological comorbidities, and bedridden state (P < 0.05). ICU admission was associated with the time from injury to operation, preoperative neurological comorbidities and frequent intraoperative hypotension (P < 0.05).
Conclusions
Adequate treatment of respiratory comorbidities and prevention of cardiovascular complications might be the critical factors in reducing postoperative mortality in elderly patients undergoing hip fracture surgery.
Introduction
A significant proportion of hip fractures affect the elderly, and most cases require surgical treatment [1]. Elderly patients usually present multiple comorbidities, including cardiovascular and respiratory diseases, which contribute to their high mortality rate following hip fracture surgery [2]. The rates of postoperative complications after hip fracture surgery range between 12.5 and 30.0% [345]; the mortality rate during the acute phase (i.e., within one month of the injury) is about 4.5-10.0% [46], while the rate in the first year of the injury is about 14-36% [7]. These high morbidity and mortality rates lead to increased medical expenses [8].
Analyses of the factors related to postoperative mortality and complications in older hip fracture surgical patients can contribute to improving their clinical outcomes. Among the various factors affecting the postoperative prognoses of hip fracture patients, the patients' medical condition - as defined by their American Society of Anesthesiologists (ASA) physical status - is known to have the greatest effect on the complications and mortality rates of elderly patients [59]. Studies have reported that factors such as old age, male gender [3], arthroplasty [10], general anesthesia [10], and long delays between the admission time and surgery [10], were associated with high mortality rates. However, further research is required to verify these conclusions, as other studies have reported contradictory results [591112].
This retrospective study set out to determine the factors that contribute to postoperative deaths and cardiovascular and respiratory complications in elderly patients who have undergone hip fracture surgery. In addition, it analyzed the factors affecting intensive care unit (ICU) admission, prolonged ICU stay, and prolonged postoperative length of hospital stay.
Materials and Methods
This study was conducted with the approval of the Institutional Review Board of our hospital. The subjects were elderly patients aged 65 or older who had undergone orthopedic surgery at our hospital for a femur neck fracture or intertrochanteric fracture of the femur under either general or regional anesthesia between January 2011 and June 2014. After excluding patients with multiple trauma, accompanying pelvic bone fractures, accompanying avascular necrosis of the femur head, periprosthetic fractures, metastatic malignant tumors, and those undergoing reoperations, a total of 464 out of 494 eligible patients were included in the study.
The collected data were limited to the patients' medical records taken during their hospitalization for hip fracture surgery. Factors such as the patients' gender, age, height, weight, ASA physical status, comorbidities, type and duration of anesthesia, type of surgery, and time from injury to operation (TimeINJ-OP) were examined.
Preoperative medical conditions and comorbidities were confirmed by the consultation records. Preoperative hypertension, arrhythmia, heart failure, ischemic heart disease, cardiac valvular disease, and cardiomyopathy were classified as cardiovascular comorbidities, while chronic obstructive pulmonary disease and asthma were categorized as respiratory comorbidities. In addition, histories of cerebrovascular accident, dementia, or Parkinson's disease were regarded as neurological comorbidities. The patients' medical records were also checked for the presence of renal failure, delirium, or other accompanying diseases (diabetes, liver disease, or peripheral arterial obstructive disease). Furthermore, the patients' premorbid ambulatory state, emergency surgery, type of surgery, and frequent intraoperative hypotension (i.e., more than three occurrences of systolic pressure under 90 mmHg) were also examined.
Patients' deaths during their hospital stay and the occurrence of postoperative complications were recorded as outcome variables. Any occurrence of postoperative complications was confirmed by the department's consultation records. More specifically, the medical records were reviewed to evaluate the presence of any postoperative cardiovascular complications (myocardial infarction, heart failure, cardiogenic shock, or newly-occurring or aggravated arrhythmia), respiratory complications (pneumonia, pulmonary edema, atelectasis, pleural effusion, or hypoxemia), sepsis, delirium, stroke, pulmonary embolism, or wound infection. Furthermore, the patients' postoperative ICU admission, length of ICU stay, and postoperative length of hospital stay were investigated.
Statistical analysis
The data are presented as the mean ± SD or number of patients (percentage). The R for windows (version 3.2.0, R Foundation for Statistical Computing, Vienna, Austria) was used for the statistical analyses. A logistic regression analysis based on a binomial generalized linear model was performed to identify the factors affecting the postoperative outcomes. Death, cardiovascular complications, respiratory complications, delirium, ICUADM (ICU admission), ICULONG (a stay of more than two days in the ICU or death in the ICU), and a prolonged postoperative length of hospital stay (postoperative hospital stay > 30 days), were considered as the postoperative outcomes. In order to identify the factors affecting each outcome, we first performed a univariate analysis to determine the factors with a P value under 0.2, and included these factors in a multivariate analysis. The items with P values under 0.05 in the multivariate analysis were considered statistically significant.
In order to identify the factors affecting the postoperative mortality, we analyzed the associations between the preoperative factors, including the patients' characteristics, medical conditions, and comorbidities and deaths. The following factors were set as independent variables: the age, gender, height, weight, ASA physical status, cardiovascular comorbidity, respiratory comorbidity, neurological disorder, renal failure, other accompanying diseases, delirium, TimeINJ-OP, ambulatory condition prior to injury, type of surgery, emergency surgery, and frequent intraoperative hypotension.
Moreover, the association of the postoperative mortality with the following postoperative variables was analyzed: low-molecular-weight heparin (LMWH) administration, cardiovascular complication, respiratory complication, pulmonary embolism, sepsis, acute renal failure, delirium, and wound infection.
A logistic regression analysis was performed using the aforementioned preoperative factors as independent variables in order to determine the factors associated with postoperative complications (cardiovascular complications, respiratory complications, and delirium).
The relationship between the preoperative variables and the ICUADM was also examined. In addition, a logistic regression analysis was performed with the above-mentioned preoperative and postoperative variables in order to identify the factors associated with ICULONG and a prolonged postoperative length of hospital stay.
Results
The subjects of the study (464 subjects) were aged 79.5 ± 7.3 years. The patients' characteristics, anesthesia- and surgery-related information, as well as their existing accompanying diseases, are detailed in Tables 1 and 2. Eight patients (1.7%) died during hospitalization, and 22 (4.7%), 91 (19.6%), and 99 patients (21.3%), respectively, suffered from postoperative cardiovascular complications, respiratory complications, and delirium (Table 3). The length of time from admission to discharge was 25.9 ± 11.6 days; 33 patients (7.1%) were admitted to the ICU after surgery, and they stayed for about 6.8 ± 9.3 days (Table 3).
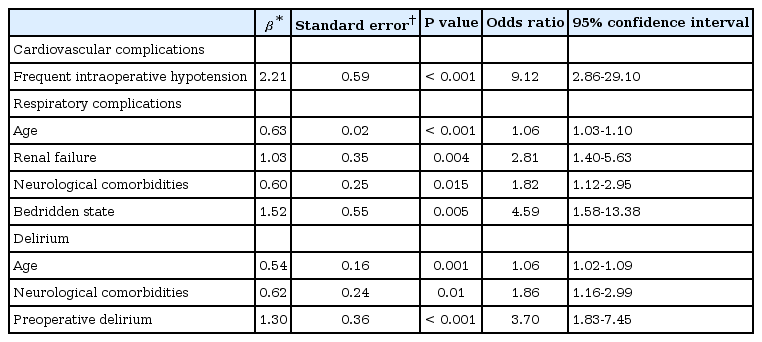
The results of the logistic regression analysis performed to identify the associations between the different variables and postoperative outcomes are presented in Tables 4, 5 and 6. No multicollinearity was found between the variables in the logistic regression. The presence of a respiratory comorbidity prior to the surgery was associated with postoperative death (P = 0.035); furthermore, postoperative cardiovascular complications were significantly associated with postoperative death (P = 0.012) (Table 4). Postoperative cardiovascular complications were associated with frequent intraoperative hypotension (P < 0.001). Postoperative respiratory complications were associated with the patient's age (P < 0.001), preoperative renal failure (P = 0.004), existing neurological comorbidities (P = 0.015), and a bedridden life prior to injury (P = 0.005). Of the 99 patients with postoperative delirium, 20 patients already suffered from delirium before the surgery, while 79 patients did not. Postoperative deliriums were significantly associated with the patients' age (P = 0.001), preoperative neurological comorbidities (P = 0.01), and preoperative delirium (P < 0.001) (Table 5). The age of the patients with postoperative delirium was 82.0 ± 7.1 years.

Logistic Regression for the Influence of Risk Factors on ICUADM & ICULONG & Prolonged Postoperative Stay
Sixteen out of the 33 patients admitted to the ICU after surgery had initially been scheduled to stay in the ICU for better postoperative management of their accompanying diseases; thirteen were admitted to the ICU unexpectedly on account of an unanticipated postoperative problem; and the remaining four patients were already in the ICU prior to surgery and stayed in the ICU after surgery. The specific reasons for ICU admission are shown in Table 3. Incidences of ICU admission were associated with the TimeINJ-OP (P = 0.002), preoperative neurological comorbidities (P = 0.008), and frequent intraoperative hypotension (P < 0.001) (Table 6). The TimeINJ-OP for all the subjects was 6.1 ± 5.0 days, while that for the 33 patients admitted to the ICU was 9.2 ± 7.0 days, and that for the patients who were not admitted to the ICU was 5.9 ± 4.7 days.
Twenty patients out of the 33 ICU-admitted patients stayed in the ICU for more than two days, or died in the ICU (ICULONG). These patients were significantly associated with preoperative neurological disorders (P = 0.001) and open reduction and internal fixation (ORIF) types of surgeries (P = 0.002) (Table 6).
Forty-eight patients stayed in the hospital for more than 30 days after the surgery, with a postoperative length of hospital stay of 44.3 ± 14.5 days. Postoperative pulmonary embolisms (P = 0.012), wound infection (P = 0.002) and preoperative renal failure (P < 0.001) were significantly associated with a prolonged postoperative length of hospital stay (Table 6).
Discussion
In this study, the rate of mortality in the course of hospital stays after hip fracture surgery was 1.7%. This was relatively low in comparison with the 4.5-10.0% found in previous studies [46]. However, unlike in these studies, which had examined the mortality rates over a specific period of time (e.g., for one month after surgery) [46], the present study surveyed the mortality rate of hospitalized patients during their hospital stay only; therefore, it only followed up on patients for a short period of time, as the postoperative length of hospital stay for most patients was about 17.9 ± 5.4 days, with the exception of 48 patients who stayed for more than 30 days.
Postoperative death was associated with several factors. In this study, the patients' respiratory comorbidities and postoperative cardiovascular complications were significantly associated with postoperative death. The existing literature reports various factors associated with postoperative death. Eiskjaer and Ostgard [9] found that patients' medical conditions had the greatest effect on postoperative death, while Kenzora et al. [5] stated that the postoperative mortality rate was increased when patients presented more than four comorbidities. It was reported that regional anesthesia was associated with a reduced mortality, as compared with general anesthesia [10]. However, another study found no difference between general anesthesia and regional anesthesia in terms of postoperative mortality [12]. There have been contradictory reports on the effects of delayed surgery on the mortality rate [913]. Emergency operations have been associated with a higher mortality rate and greater incidence of postoperative complications than elective surgeries [14]. In one study, older age was associated with a higher mortality rate [3], while in another, the age was inversely proportional to the mortality rate in the first year after surgery [11]. There have been inconsistencies in the associations between gender and mortality [35], as well as in the effect of postoperative LMWH administration on postoperative mortality [1516].
The factors shown to affect postoperative mortality in previous studies were not significantly associated with this outcome in the present study. On the other hand, respiratory comorbidities and postoperative cardiovascular complications were found to be significantly associated with postoperative mortality. This was in line with the results reported by Takamine et al. [17] and Lawrence et al. [18], whose studies identified respiratory diseases and postoperative cardiovascular complications, respectively, as important risk factors of mortality. The fact that postoperative cardiovascular complications were significantly associated with postoperative death suggests that postoperative care is critical for patients who have undergone hip fracture surgery.
In this study, postoperative cardiovascular complications - a major risk factor of mortality - were related to frequent intraoperative hypotension. According to Walsh et al. [19], postoperative myocardial damage occurs more frequently when the intraoperative mean arterial pressure is lower than 55 mmHg even for a short period. Hence, the taking of precautions to prevent intraoperative hypotension is presumed to be helpful in reducing postoperative cardiovascular complications and mortality.
A premorbid ambulatory state may be an indication of functional impairment. One study reported that the postoperative mortality rates were higher in bedridden patients and patients who were only capable of walking indoors than in patients with normal ambulation [20]. In the present study, a premorbid ambulatory state did not have a significant impact on postoperative mortality but was an important factor of postoperative respiratory complications. Moreover, the patients' age, preoperative renal failure, and neurological comorbidities were associated with postoperative respiratory complications; other studies also found that old age and preoperative renal failure were associated with postoperative respiratory complications [221]. The frequency of postoperative respiratory complications in this study was 19.6%, a higher rate than that reported by Lawrence et al. (4%) [18]. This was presumed to be caused by the inclusion of frequently-occurring hypoxemia as one of the respiratory complications in this study.
There has been debate about the effect of postoperative delirium on the mortality rate after hip fracture surgery. Mazzola et al. [22] suggested that postoperative delirium was a significant predictor of postoperative death, while Gottschalk et al. [23] did not find a significant relationship between the two, in keeping with the results of this study. However, delirium must be carefully managed in elderly patients, as it can affect other postoperative complications as well as the length of the hospital stay [24]. In the present study, the patients' age, preoperative neurological disorders, and preoperative delirium had significant effects on the incidence of postoperative delirium. Juliebo et al. [25] suggested that cognitive dysfunction, indoor injury, and a body mass index under 20 were important risk factors of postoperative delirium among hip fracture patients. Moreover, Bitsch et al. [26] suggested that old age and dementia were strongly associated with postoperative delirium in hip fracture patients. These results were consistent with our findings.
Patients can be admitted to the ICU after surgery for the treatment of serious postoperative complications or existing comorbidities. According to Kamath et al. [27], patients who had been scheduled to be admitted to the ICU for the management of existing diseases had a better postoperative prognosis than those who were taken to the ICU unexpectedly on account of postoperative complications. Similarly, in the present study, five out of the 13 patients who required unexpected ICU admission died, against only one out of the 20 patients scheduled for planned ICU admission. A number of previous studies have also examined the relationship between postoperative admission to the ICU and the anesthetic method. AbdelSalam et al. [28] observed that patients who had received general anesthesia were more frequently taken to the ICU after surgery. By contrast, no significant correlation was found between the type of anesthesia and the incidence of postoperative admission to the ICU in the present study; however, the TimeINJ-OP, neurological comorbidities, and frequent intraoperative hypotension had significant effects on the incidence of postoperative admission to the ICU. In the present study, most of the patients admitted to the ICU for comorbidities or unstable vital signs before or after surgery did not develop any serious complications, and were transferred to a general ward within two days. Therefore, the patients included in the ICULONG category presented relatively more severe conditions than the rest of the patients admitted to the ICU. In general, the patients with an existing neurological disorder or those who had undergone ORIF surgery stayed in the ICU for more than two days.
Basques et al. [29] reported that the postoperative length of the hospital stay after hip fracture surgery was longer when the time from admission to operation had been long and when the patients had received regional anesthesia. In a different study, regional anesthesia contributed to shorter hospital stays after surgery [12]. The type of surgery was also associated with the postoperative length of hospital stay [29]. In the present study, the anesthetic method and type of surgery did not affect the postoperative length of hospital stay; however, preoperative renal failure, postoperative pulmonary embolism, and wound infection were significantly associated with a prolonged postoperative stay.
Unfortunately, the results of this study cannot be generalized as the study was only conducted in one healthcare institution. Another limitation of this study lies in the fact that it did not follow up on the patients after discharge, as the focus was on the postoperative deaths and complications taking place during the hospital stay. Hence, this study cannot suggest predictors for death or long-term complications. Future studies should conduct prospective investigations in multiple institutions and with long-term follow-up in order to address these limitations.
This study analyzed the factors affecting the postoperative outcomes of elderly patients having undergone hip fracture surgery. Preoperative respiratory comorbidities and postoperative cardiovascular complications were associated with postoperative death. Therefore, the appropriate treatment of patients' existing respiratory diseases and the prevention of postoperative cardiovascular complications should be emphasized in order to improve the outcomes of hip fracture surgery. In addition, intraoperative hypotension, which is associated with cardiovascular complications and ICU admission, should be managed appropriately. As old age, preoperative neurological disorders, renal failure, and a bedridden state are associated with postoperative respiratory complications, extra care should be taken to prevent respiratory complications in patients presenting these factors.