The degree of labor pain at the time of epidural analgesia in nulliparous women influences the obstetric outcome
Article information
Abstract
Background
The increased pain at the latent phase can be associated with dysfunctional labor as well as increases in cesarean delivery frequency. We aimed to research the effect of the degree of pain at the time of epidural analgesia on the entire labor process including the mode of delivery.
Methods
We performed epidural analgesia to 102 nulliparous women on patients' request. We divided the group into three based on NRS (numeric rating scale) at the moment of epidural analgesia; mild pain, NRS 1-4; moderate pain, NRS 5-7; severe pain, NRS 8-10. The primary outcome was the mode of delivery (normal labor or cesarean delivery).
Results
There were significant differences in the mode of delivery among groups. Patients with severe labor pain had a significantly higher cesarean delivery compared to patients with moderate labor pain (P = 0.006). The duration of the first and second stage of labor, fetal heart rate, use of oxytocin and premature rupture of membranes had no differences in the three groups.
Conclusions
Our research showed that the degree of pain at the time of epidural analgesia request might influence the rate of cesarean delivery. Further research would be necessary for clarifying the mechanism that the augmentation of pain affects the mode of delivery.
Introduction
The degree of pain during labor progress has been suggested to be associated with prolonged labor or the frequency of the cesarean delivery [1,2,3]. Labor pain differs greatly from individual's physical and mental condition and became severe as uterine cervical dilation increases while labor progresses. Several studies reported an association between obstetric outcome and pain score in relatively advanced labor [1,3], whereas two previous reports have suggested that the degree of pain at the time of epidural analgesia can influence the obstetric result. In 1989, Wuitchik et al. [2] demonstrated that pain in the latent phase was predictive of mode of delivery and duration of labor, however, they did not provide any information about analgesic method including epidural analgesia. On the contrary, Beilin et al. [4] did not found an association between the labor pain at the time of epidural analgesia and mode of delivery in their retrospective study. Many variables including the timing of epidural analgesia and pain assessment method were not controlled that could affect their results.
In this prospective research, we investigated the effect of the severity of labor pain at the time of epidural analgesia on the mode of delivery in nulliparous women. We hypothesized that labor pain at the time of epidural analgesia would be associated with the entire labor process including the mode of delivery.
Materials and Methods
This study was approved by the Hospital Ethics Committee at our institution and written informed consent was obtained from all women. The American Society of Anesthesiologists physical status I-II nulliparous women who requested epidural analgesia during working hours were enrolled from January to December 2013. The inclusion criteria were singleton pregnancies, gestational ages of 35-41 weeks, cervical dilatation of less than 4 cm and vertex fetal presentations. We considered a cervical dilatation under 4 cm to indicate latent phase of labor. The women who had pregnancy complications, contraindication of epidural analgesia or fetal abnormality were excluded.
The epidural analgesia was done when the patients requested epidural analgesia for pain relief. The patient's pulse, blood pressure, oxygen saturation, fetal heart rate and the cervical dilatation were checked before the procedure. The pain was evaluated with numeric rating scale (NRS; 0, no pain to 10, unimaginable pain) at the time of epidural analgesia. Based on this NRS scores, the patients were divided into three groups; 1-4 for mild pain, 5-7 for moderate pain, and 8-10 for severe pain.
Before epidural analgesia, we injected 500-1,000 ml of lactated Ringer's solution. The patient was placed in the right lateral decubitus position. A 17-gauge Tuohy needle was inserted towards the epidural space with the loss of air resistance method at the lumbar spine between L2-L5. We inserted a catheter into the epidural space and brought the catheter tip above 4 cm from the insertion level. We injected 3 ml of chirocaine 0.375% including a concentration of 1 : 200,000 epinephrine as a test dose. The patient was turned to a supine position with a wedge beneath the right side for left uterine displacement. After confirming no sign of subarachnoid injection and blood vessel injection, 10 ml of ropivacaine 0.15% including fentanyl 50 µg was injected as a loading dose. This was followed by a continuous epidural infusion of ropivacaine 0.1% and fentanyl (1.5 µg/ml) at a speed of 10 ml/h through the machine (AC 110, Ambix, Ehwa Medical, Seoul, Korea).
After the procedure, blood pressure, pulse of the patients and fetal heart rate were recorded. Sensory blockade level by using alcohol cotton and pain score by NRS were assessed 30 minutes after injection of loading dose. The first stage of labor was defined as the time from the moment performing epidural analgesia to the instant when the cervix dilated about 10 cm. The second stage of labor was defined as the time from 10 cm dilated cervix to delivery. The primary outcome was the mode of delivery; spontaneous vaginal delivery or cesarean delivery. The duration of the first and second stage of labor, usage of oxytocin, amniorhexis, fetal weight at the time of delivery and Apgar score were recorded.
Statistical analysis
SPSS (ver. 18.0, Chicago, IL, USA) was used for the statistical analysis. Data are presented as mean ± standard deviation (SD) or median with interquartile range (IQR) as appropriate. The Kolmogorov-Smirnov test was used to test for normality of the distribution. Continuous variables were analyzed by ANOVA or Kruskal-Wallis test after assessment for normality. Discrete variables were analyzed using chi-square test. Then, a Bonferroni correction was applied for three comparisons between groups and adjusted P value (P < 0.05/3 = 0.017) was considered statistically significant. Otherwise, P values of less than 0.05 were considered statistically significant.
Results
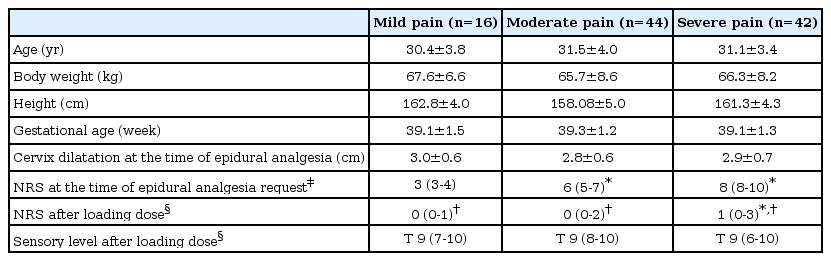
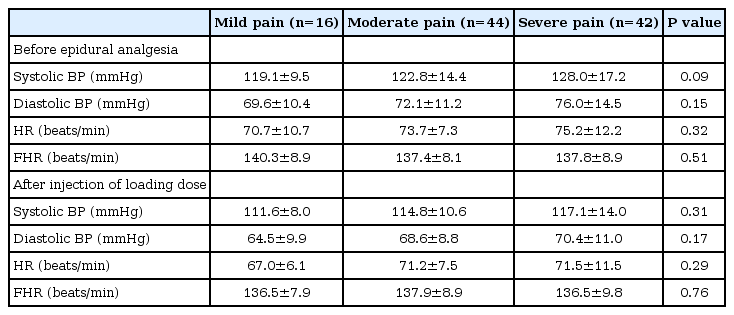
During the period of the study, 102 nulliparous women received epidural analgesia during working hours. Of these, 16, 44 and 42 women had the mild, moderate and severe pain at the time of epidural analgesia, respectively. There were no differences in age, height, weight, gestational age and the degree of cervical dilatation at the time of epidural analgesia in the three groups. Thirty minutes after epidural injection of the loading dose, satisfactory sensory blockade and significant pain relief was achieved in all groups although there was a statistical difference in NRS among groups (Table 1). The parturient women's blood pressure, pulse and fetal heart beats before and after epidural analgesia showed no differences, and none of the patients had any abnormal findings such as hypotension or bradyarrhythmia (Table 2).
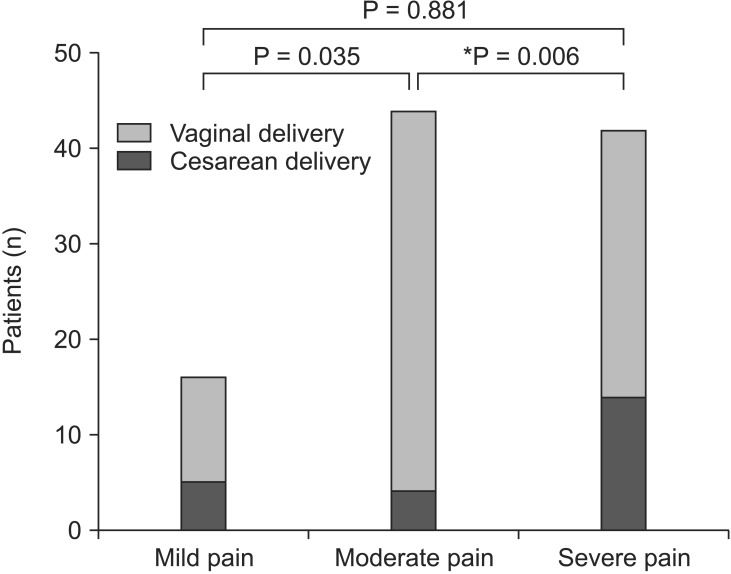
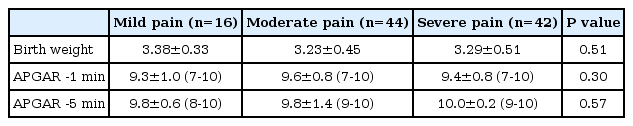
There were significant differences in the mode of delivery among the three groups (P = 0.018); 5 of 16 patients, 4 of 44 patients and 14 of 42 patients in the low, moderate and severe pain group, respectively (Fig. 1). The patients with severe labor pain had a significantly higher cesarean delivery compared with moderate pain group (P < 0.017) but revealed no significant difference in the mode of delivery when compared with mild pain groups (P > 0.017). Cesarean delivery was performed at the discretion of the obstetrician, as indicated. In patients with mild pain, two were performed for fetal distress and three for dystocia. In patients with moderate pain, three had cesarean delivery for fetal distress and one for dystocia. In patients with severe pain, eight had cesarean delivery for fetal distress and six for dystocia. The other parameters such as oxytocin usage, premature rupture of membranes and duration of the first and second stage of labor had no differences among the three groups (Table 3). Neonatal outcome, weight or Apgar score at 1 or 5 minute showed no differences either. There was no newborn baby whose Apgar score was under 7 (Table 4). Our results achieved a power of 0. 99 and an α of 0.05. (chi-square test).
Discussion
We investigated whether the degree of labor pain at the time of epidural analgesia, latent phase of labor, affected labor progress in nulliparous women who underwent epidural anesthesia. We found that the degree of labor pain in the latent phase was associated with the mode of delivery. The cesarean delivery rates were higher in the group experiencing severe pain (33.33%) than in the group experiencing moderate pain (9.09%). The degree of labor pain at the time of epidural analgesia was not related to the duration of the first and second stage of labor. The present study minimized bias against the impact of epidural analgesia on the cesarean delivery by conducting a prospective study by standardization of patient management such as analgesic methods. Moreover, previous lots of studies used indirect studies that evaluated pain by the number of requests for an additional analgesics [1,2,3,5,6,7,8,9,10,11,12], while this study divided into groups on the basis of only initial pain. There was also no difference among three groups in maternal, fetal and obstetric factors that could have an impact on labor pain and dystocia.
There has been an ongoing debate about the issue that epidural analgesia during labor can increase cesarean delivery rates. Some authors demonstrated that epidural analgesia could increase the rate of forceps and cesarean delivery [5,6,13,14]. However, most recent studies show that epidural analgesia using a low concentration of local anesthetic and narcotics do not increase cesarean delivery rates while it can extend labor times [7,8,9,10,11]. The increased rate of cesarean delivery in individuals who received epidural analgesia can be explained by various factors such as mother or fetus' factors, not by a direct relationship with epidural analgesia. Among them, labor pain is one of the factors to relate with the obstetric outcome and can be a confounding factor when interpreting effects of epidural analgesia on labor outcome [1,2,3,6,12].
The target groups in this study were divided into three groups using a NRS on the basis of previous studies [4,15,16,17]. Usually the pain of the NRS 1-4 belongs to mild pain with a minimal impact of pain and NRS 5-6 indicated moderate pain with a greater impact on the functioning. The pain of the NRS 7 or higher indicated a severe pain with the greatest impact on the functioning [15]. According to measurement using a visual analog scale by Collins et al. [16], moderate pain and severe pain were the average 49 and 75, respectively. Also, Wallenstein et al. [17] showed that the average VAS score of moderate pain and severe pain were 50 and 80, respectively.
The frequency of receiving the cesarean delivery due to dystocia among pregnant women who received epidural analgesia was vary from 5 to 25%, which indicated that other various factors were involved beside epidural analgesia itself [1,2,3,6,12]. The labor progress is very complex and dystocia can be induced by various causes such as a fetus size, fetal presentation, the anatomy of the pelvic, a uterine malformation, maternal age, use of oxytocin, and uterine activity.
It was highlighted that the pain and cognitive activity in the latent phase, not in the active phase, were a prognostic of obstetric outcome of labor progress [2], which was consistent with our results. Those authors reported that patients who complained of severe pain in their latent phase showed prolonged labor time, increased frequency of dystocia and surgical labor rates, when compared with the patients who had less pain. On the other hand, Beilin et al. [4] presented their retrospective results that nulliparous women showed no difference cesarean delivery rates regardless of labor pain at the time of epidural placement. However, this retrospective study included more patients experiencing pre-diagnosed dystocia than other studies, which led to much higher cesarean delivery rates in all groups.
Little has been known about the mechanism that the augmentation of pain increases dystocia. Severe pain in the latent phase could increase the levels of catecholamine and cortisol and reduce uterine activity [2,18]. Our results showed that cesarean delivery frequency in patients with severe pain was significantly higher than that in patients with moderate pain. However, there was no difference between mild and severe pain group. We considered these results for two reasons. First, the number of patients with mild pain was less than other groups. Second, there is a possibility that the epidural analgesia was too early conducted because it was performed on the patients' request. There is a controversy over whether the time of epidural analgesia is a factor that can affect labor outcome, although most recent studies have concluded that early placement of epidural analgesia do not increase the cesarean delivery rates [9,19]. Holmes et al. [20] reported that women who present to hospital at 0-3 cm of cervical dilatation have a higher risk of caesarean delivery regardless of epidural analgesia.
There were some limitations of this study. First, a few patients relatively participated in this study. This was because that the overall delivery rates have been declined, and only nulliparous women with fetuses in vertex presentation were selected. The criteria of cervical dilation was determined up to 4 cm, and overnight deliveries were excluded. Second, as patients were allowed to choose the time of epidural analgesia on their request, the measurement of the NRS at the moment of epidural analgesia might be affected. Third, supplemental boluses except for a constant epidural continuous infusion were not administered during the labor progress.
In conclusion, the pain score at the time of epidural analgesia might affect the methods of delivery. The severe pain at the latent phase should be considered not as the low pain thresholds of patients simply but as a marker of intrinsically difficult labor and more careful management would be needed. Also, the labor pain at latent phase can play a role of potential confounding factor in the study regarding an association between the epidural analgesia and the cesarean delivery rate. As labor progress is influenced by complex factors, further studies will be needed in order to find out the mechanism that the augmentation of pain increases dystocia.