The intermittent bolus infusions of rapid infusion system caused hypothermia during liver transplantation
Article information
Hypothermia is frequently encountered during major operations despite many efforts to prevent this complication. Numerous reports have identified the adverse effects of hypothermia including coagulopathy, acidosis, alterations in response to pharmacological agents, detrimental cardiac arrhythmias, and a mortality rate of near 100% for cases with a core body temperatures of 32℃ [1,2]. Therefore, a variety of devices have been developed to achieve rapid fluid warming and infusion because prevention of hypothermia via intravenous infusion of warm fluid is probably the most cost effective intervention, particularly for circumstances in which large volumes of fluid are required. However, after the utilization of the rapid infusion system (RIS) in liver transplantation (LT) recipients, we noticed a considerably lower intraoperative body temperature (BT) compared to the recipients before RIS. Therefore, in this study, we aimed to compare the BTs of LT recipients before and after receiving RIS.
Medical records of adult patients who underwent first LT were reviewed. Twenty-three recipients were divided into non-RIS (n = 12) and RIS (n = 11) groups. The exclusion criteria included patients with model for end-stage liver disease score less than 9 or greater than 25, total input greater than 20 L, and RIS infusion less than 4 L. After induction, either RIS (Haemonetics Corp., Braintree, MA, USA) or Level 1 (Level 1 Technologies, Rockland, MA, USA) was connected to the Advanced Venous Access catheter (Edwards Lifesciences LLC, Irvine, CA, USA) placed in the right internal jugular vein. For external methods of warming and body temperature preservation, a water circulating heating mattress was used and the extremities were insulated with cotton rolls and vinyl covers. The operating room temperature was set to 24℃. Ward BT one hour before surgery (T-ward), seven intraoperative BTs, lowest intraoperative BT, and the first BT upon arrival at the intensive care unit (ICU) were compared between the two groups. In addition, the temperature of the fluid in the tubing of RIS was measured with increasing time intervals from 1 minute to 5 minutes after recirculation. BTs in the ward before operation and at ICU after operation were measured by a digital thermometer from the patient's axilla. Intraoperative BT and temperature of the fluid in the tubing of RIS (the end of the tubing which would be attached to the patient) were measured with a pulmonary artery catheter (Model 774HF75, Edwards Lifesciences LLC, Irvine, USA) connected to a Vigilance monitor (Edwards Lifesciences LLC, Irvine, USA). Statistical comparisons were performed using the t-test for parametric data and the Mann-Whitney U test for non-parametric data. The chi-square test was used to examine gender. A P value < 0.05 was considered statistically significant.
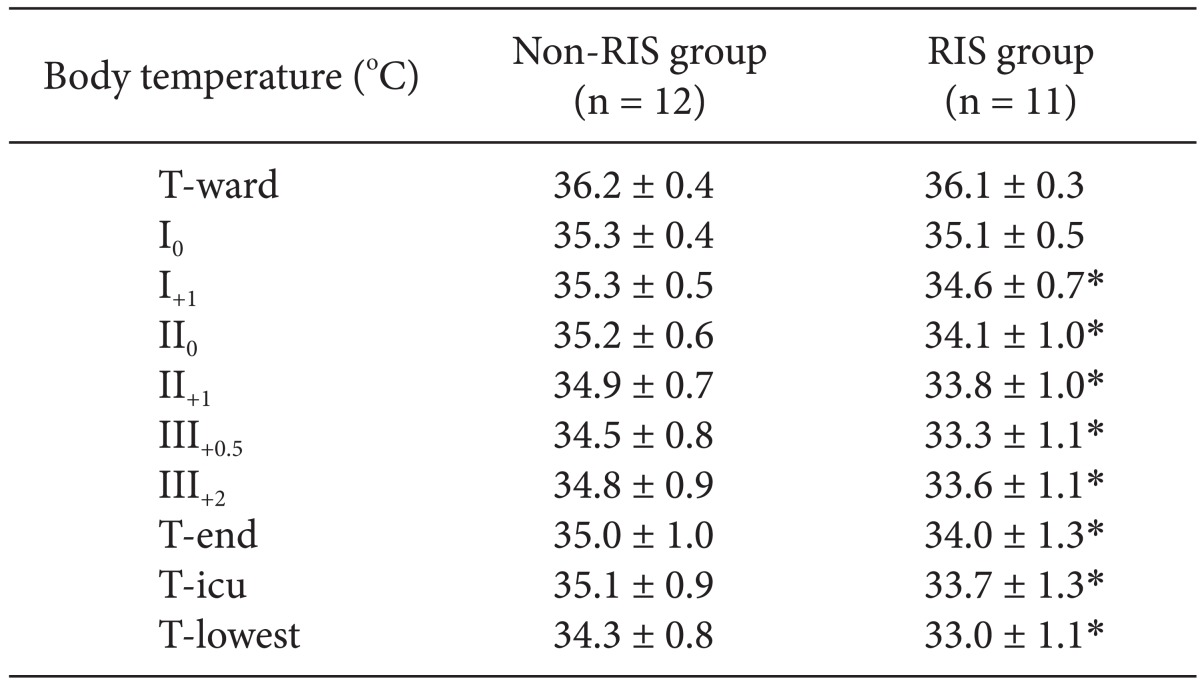
The BTs in the ward one hour before operation (T-ward) and skin incision (I0) were not different between the two groups. However, a greater decrease was observed in the RIS group over the period from one hour after skin incision to arrival at ICU compared with the non-RIS group (Table 1). The temperature of the fluid in the tubing of RIS showed a progressive decrease with increasing time intervals (38.1, 36.1, 34.3, 32.8, 31.4, and 30.2℃ for the initial, 1, 2, 3, 4, and 5 min after recirculation, respectively). The total fluid input of the non-RIS group was 11455.7 ± 3350.9 ml, that of the RIS group was 12482.4 ± 4313.1 ml.
Fluid management with intermittent bolus infusion from RIS is associated with more rapid decrease of BT in LT recipients and it may be attributed to the cooling of the fluid in the infusion line outside the recirculation circuit between each bolus infusion. The RIS group in comparison to those with continuous infusion with Level 1 showed a more rapid decrease in BT in LT recipients. In addition, the temperature of the fluid in the tubing of RIS rapidly decreased with increasing time intervals. These results collectively show that intermittent bolus infusion from RIS can cause significant hypothermia.
Gradually, RIS has become a life-saving device in major surgeries, including aortic dissections and severe traumas such as liver laceration, because it can rapidly resuscitate hypotension and reduce hypothermia by delivering blood, crystalloids, or colloids warm up to the normal body temperature at a rate up to 1,500 ml/min [3]. Furthermore, the well-known benefits of RIS are minimization of lactate levels and coagulopathy while optimizing the hemoglobin level [4]. Most blood warmers including RIS are most effective at moderate to high flow, whereas at a low flow of less than 50 ml/h by conventional dry-wall warmers, the temperature of the fluid reaching the patient drops because of cooling within the tubing [5].
In our study, the BT of patients at the beginning of the operation showed no difference between the non-RIS and RIS groups, but 1 hour later, the BT in the RIS group displayed a significant decrease and remained low throughout the operation. In addition, inspite of warming the fluids by recirculation, the temperature of the bolus injectate of RIS rapidly decreased from 38.1 to 30.2℃ over 5 min intervals. Such substantial decrease in the temperature of the bolus injectate of RIS may compromise the patient if the infusion of these cooled fluids continue. The volume of the fluid in the infusion line outside the recirculation circuit of RIS was 105 ml. This means that the intermittent bolus infusion of 100 ml or 500 ml will invariably deliver the entire or part of this cooled fluid to the patient. Therefore, it is advised that bolus infusion of fluids from RIS should be preceded with special caution since the rapid decrease of the temperature of the bolus injectate proved that rewarming of fluids via recirculation does not warm up the fluid outside the recirculation circuit of RIS.
The limitation of our study is that we used two different methods of BT measurement: pulmonary artery catheter and digital thermometer measurements at the axilla reflecting core and shell temperatures, respectively. However, the same method was used to measure BTs at each time point between the two groups and the differences in BT were sought in each session of BT measurement.
In conclusion, the results of our study demonstrate that RIS may not ensure infusion of warmed fluids in cases of intermittent bolus infusion. Therefore, clinicians should proceed with caution when using bolus attempts from RIS.