The effect of heated breathing circuit on body temperature and humidity of anesthetic gas in major burns
Article information
Abstract
Background
Cold and dry gas mixtures during general anesthesia cause the impairment of cilliary function and hypothermia. Hypothermia and pulmonary complications are critical for the patients with major burn. We examined the effect of heated breathing circuit (HBC) about temperature and humidity with major burned patients.
Methods
Sixty patients with major burn over total body surface area 25% scheduled for escharectomy and skin graft were enrolled. We randomly assigned patients to receiving HBC (HBC group) or conventional breathing circuit (control group) during general anesthesia. The esophageal temperature of the patients and the temperature and the absolute humidity of the circuit were recorded every 15 min after endotracheal intubation up to 180 min.
Results
There was no significant difference of the core temperature between two groups during anesthesia. The relative humidity of HBC group was significantly greater compared to control group (98% vs. 48%, P < 0.01). In both groups, all measured temperatures were significantly lower than that after intubation.
Conclusions
The use of HBC helped maintain airway humidity, however it did not have the effect to minimize a body temperature drop in major burns.
Introduction
Since heating and humidification are not physiologically available in patients who received endotracheal intubation, cold and dry gas mixtures directly reach the bottom of the airway as inspired gases pass through the upper airway of the mucosal lumen. Even if the cold gases are inspired for a short period of time without humidification, it causes various pulmonary complications and hypothermia [1]. The hypothermia that occurs during anesthesia is associated with multiple complications, including wound infection, serious cardiac complications and myocardial damages, recovery delay after anesthesia, discomfort, and mortality increases after serious injuries [2].
The hypothermia during anesthesia causes serious problems, especially in patients at high risk, such as severe burns. Body temperature function in the patients with burns is impaired by external damages, thereby increasing all heat loss. Not only secondary loss due to conduction and convection increases in burned patients but also heat loss related to the evaporation at damaged dermis is much larger in patients with burns than that of ones without burns [3].
In this regard, heated breathing circuit (HBC), which actively provides heat and humidity to anesthetic breathing circuit, is considered to maintain the humidity of inspired gases and reduce the core temperature drop theoretically. Studies reported that the effects of HBC on core temperature varied in patients without burns [4-6]. Therefore, the objective of this study is to investigate the effects of HBC on core temperature and humidity of anesthetic gases in patients with severe burns during general anesthesia.
Materials and Methods
Study protocol was approved by the hospital ethics committee in advance. The study was explained to the patients prior to surgery and written consent forms were obtained. Total of 60 patients with over first-degree burns of 25% total body surface area that were scheduled for escharectomy and skin graft under general anesthesia participated in this study. These patients were 20 to 60 years old who were classified into physical class 2 or 3, based upon American Society Anesthesiologist. The study was conducted prospectively. The patients with following cases were excluded from the study; 1) patients with anamneses of diseases in the heart, liver, kidney, thyroid, and central nervous system, 2) patients who were administering vasodilators or other drugs that affect the temperature control, and 3) pregnant patients. The participants were randomly assigned to the control group, utilizing conventional breathing circuit, including a heat and moisture exchanger (HME), and a HBC group, using heated breathing circuit (RT 212 Adult inspiratory heated breathing circuit, Fisher & Paykel healthcare, Auckland, New Zealand). HBC possesses a Y shaped-connection between 1.5 m of heated inspired limb and 1.76 m of unheated expired limb with a water trap. During the surgery, temperature of beds in both groups was set at 40℃ by using hyper-hypothermia unit (Blanketrol® 2, Cincinnati Sub-Zero, Cincinnati, USA) as an additional external heating method. Temperature of the operating room was maintained at 30-32℃. Also, all fluids and blood products were injected via fluid heating unit setting at 40℃.
As a pre-treatment, 0.2 mg of glycopyrrolate was injected intramuscularly an hour before the anesthesia induction; a standard patient monitoring device was attached in the operating room. Propofol, 2 mg/kg, and rocuronium, 0.8 mg/kg, were administered and then endotracheal intubation was carried out. A portable humidification and temperature measuring device (Medisize, Hillegom, Netherlands) was turned on to operate the automatic calibration system before patients came into the operating room. In the control group, the portable humidification and temperature measuring device was installed between HME connected to the anesthetic device (Aestiva/5, Datex Ohmeda, Helsinki, Finland) and endotracheal tubes; in the HBC group, the device was installed between its own Y-shaped connection and endotracheal tubes. Temperature and absolute humidity of the inspired gases in the breathing circuit were measured in real time and recorded every 15 minutes. After the anesthesia induction, an esophageal thermometer (REF 16561, Instrumentarium Corp. Helsinki, Finland) was inserted on the bottom esophagus orally, in order to measure the core temperature; a stethoscope was mounted at the best place to hear the heartbeats. Based upon the esophageal temperature right after the endotracheal intubation as the reference values, the temperature was measured every 15 minutes for 180 minutes. The temperature drop from the reference values to the measurements were calculated and then compared between the two groups. The anesthesia was maintained at 1.5 L/min of oxygen, 1.5 L/min of nitrous oxide, and 2-3 vol% of sevoflurane 2-3 vol%. Tidal volume, respiration rate, and end-tidal partial pressure of carbon dioxide were held at 8-10 ml/kg, 12-16 rates/min, and 33-38 mmHg, respectively. Near the end of the surgery, pyridostigmine, 0.2 mg/kg, and glycopyrrolate, 0.004 mg/kg, were injected for recovery of muscle relaxation in the patients. Entire bodies except for faces and heads were disinfected with betadine solution in all patients and then the surgery was carried out as being exposed without covering special surgical drapes. Number of patients was calculated to be 24.5 subjects with α (0.05) and 1-β (0.9); the expected difference was 0.4 based upon 35.8 ± 0.5℃, which was the lowest temperature in the control group with HME utilization in previous study [6]. Therefore, the total number of patients for each group was 30 subjects. Statistical analysis was performed using SPSS (SPSS®, IBM, Chicago, USA) 12.0; t-test was carried out to compare the age, height, body weight, and surgical and anesthetic data between these two groups; sex ratio and physical class by American Society of Anesthesiologist were compared utilizing a chi-square test. Replicates of temperature, humidity, and core temperature drop were compared by repeated measures ANOVA. Post-HOC test was performed with Bonferroni correction.
Results
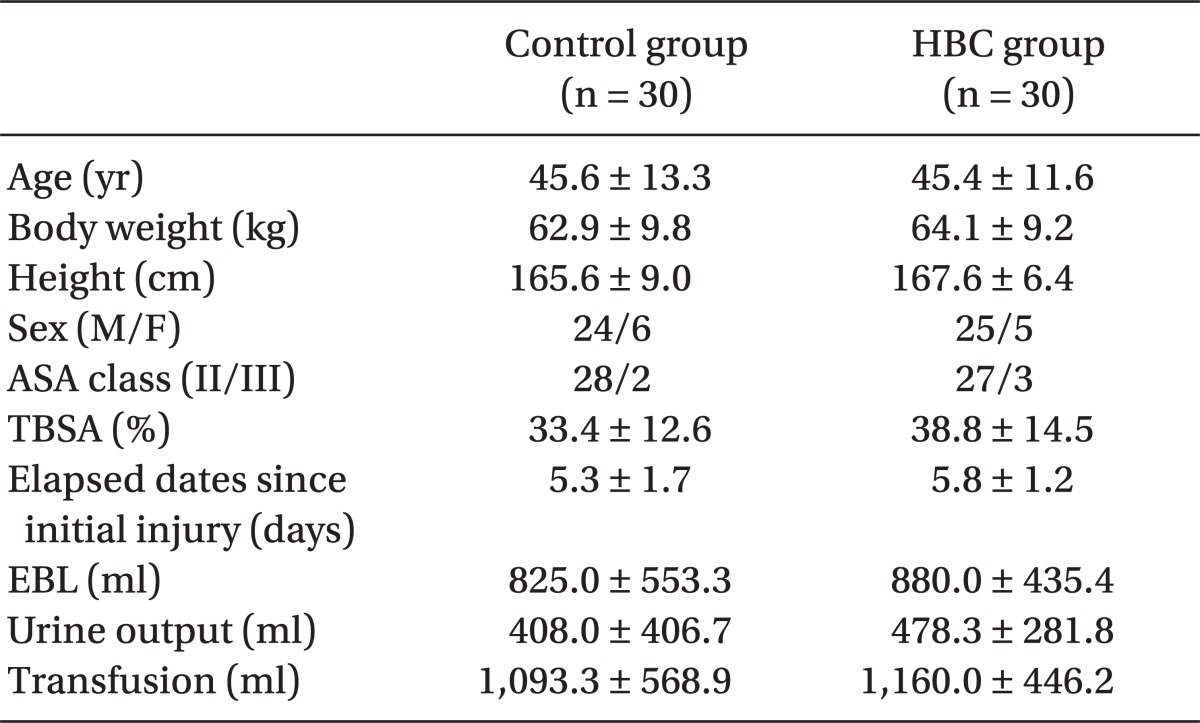
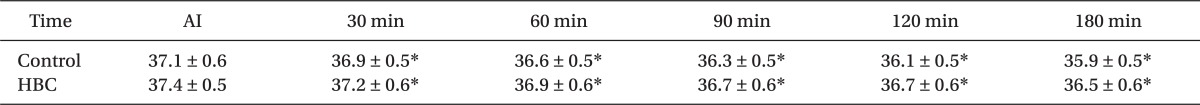
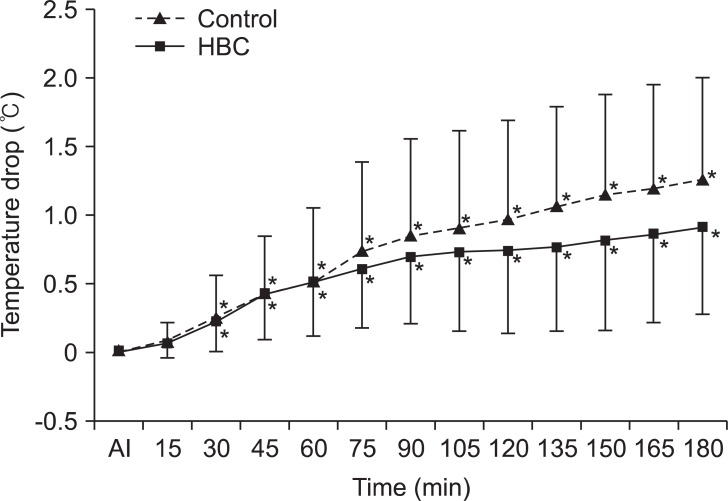
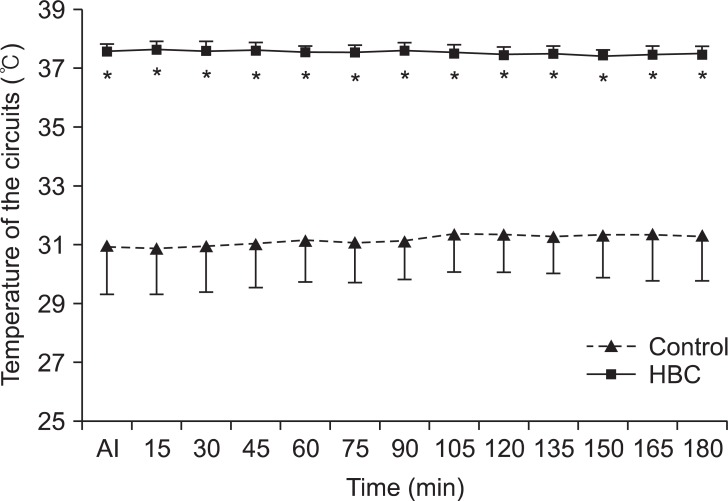
There was no statistically significant difference observed in the patients characteristics (male to female ratio, age, height, and body weight), as well as the surgical and anesthetic indicators (burned area, average elapsed dates since initial injury, urine output up till 180 minutes when temperature and humidity were measured, and transfusion) between these two groups (Table 1). The changes in the core temperature drop throughout the surgery didn't show significant difference between two groups (P = 0.2) (Table 2). In both groups, the core temperature decreased and the temperature drop elevated over time, indicating statistically significant differences (P < 0.01). Fig. 1 represents the temperature drop. The temperature drop when the surgery had been 3 hours showed 1.3 ± 0.8℃ and 0.9 ± 0.6℃ for the control group and HBC group, respectively. Temperature and absolute humidity of the inspired gases at all measurements were significantly higher in the HBC group than that of the control group (P < 0.05) and both groups showed no significant changes over time (Fig. 2 and 3). Absolute humidity and relative humidity were 42.4 mg/L and 98% at average 37.5℃ in the HBC group and 15.3 mg/L and 48% at average 31.2℃ in the control group, respectively.
The difference between temperatures from 0 to 180 min after intubation. There is no statistically significant difference between two groups. In both groups, all measured temperatures except the value at 15 min are significantly lower than that after intubation. HBC: heated breathing circuit, AI: after intubation. *P < 0.05 compared after intubation.
The change of temperatures of the gases in breathing circuit from 0 to 180 min after intubation. The temperatures of the inspired gases in HBC group are significantly greater compared to control group. HBC: heated breathing circuit, AI: after intubation. *P < 0.05 compared to control group.
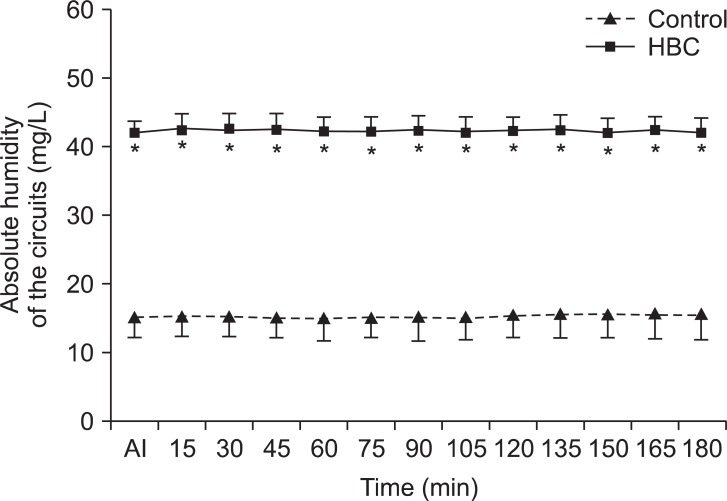
The change of absolute humidity of inspired gas in breathing circuit from 0 to 180 min after intubation. The absolute humidity of the inspired gases in HBC group is significantly greater compared to control group throughout the surgery. HBC: heated breathing circuit, AI: after intubation. *P < 0.05 compared to control group.
Discussion
The present study confirmed whereas HBC, a device providing heat and humidification by electrical heat generation, maintains higher temperature and humidity within the breathing circuit compared to that of the conventional circuit, it was not significantly effective to maintain the body temperature in patients with severe burns. If it is assumed that a healthy individual inhales gases with 50% of relative humidity at 22℃ through a nose, its absolute humidity is 10 mg/L. As inspired gases at 31-33℃ pass by the larynx, moisture content increases with 26-32 mg/L of absolute humidity and the relative humidity reaches 100%. The absolute humidity of the gases that pass by midtrachea and mainbronchi of the airway is 27-34 mg/L at 32-34℃ and 44 mg/L at 37℃, respectively, and the relative humidity is also 100% in the case. When endotracheal intubation is carried out, dry and cold gases reach to the bottom airway as physiological heating and humidification are omitted. This is why there is moisture and heat loss in respiratory systems. It also makes mucous more viscous by decreasing the ciliary transport function; ciliary movement stops when mucous gets severely viscous. So far, all the steps are reversible damages; however, if progressing further, it leads to lung compliance reductions and decreases of functional residual volume, atelectasis, and shunt as pneumocytes are damaged. The occurrence of these phenomena increases as prolonged gas inhalation increases [7].
In the present study, the average temperature and absolute humidity of the HBC group were 37.4 ± 0.1℃ and 41.4 ± 0.2 mg/L, respectively, so that the relative humidity was kept at 96%. In contrast, the control group utilizing conventional breathing circuit showed 48% of relative humidity with 31.2 ± 0.2℃ and 15.3 ± 0.2 mg/L for the average temperature and absolute humidity, respectively. This indicated that all of them were significantly lower than that of the HBC group (P < 0.01). According to Williams et al. [7], ciliary function stopped in rabbits when treating with gases of 50% relative humidity for 30 minutes. After 16 hours with 40% of relative humidity, dogs appeared to have problems in alveolar gas exchange beyond the damages of pneumocytes. In addition, when gases with 60% of relative humidity were utilized in humans for more than 1 hour, the damages were as much as ciliary function impairment, even if they were reversible. In the study, temperature and absolute humidity were 24℃ and 12 mg/L; compared to the results in the control group of the present study (31.2℃, 15.3 mg/L), absolute humidity was relatively higher in the present study, but relative humidity was lower as the temperature of the gases were higher. Since relative humidity is more important than the absolute humidity with regards to the effects of secretions within the airway [8], relative humidity considering temperature should always be regarded. On the other hand, HBC provided optimum conditions close to physiological environments by holding 98% of relative humidity. Especially in the patients with inspired burns due to flame and smoke, pulmonary complications increase even though the bottom airway is not directly damaged [3]. As surgery related to burns is generally carried out for more than 3 hours even in the patients without inspired burns, it is necessary to maintain appropriate humidity during anesthesia for a long period of time. From this perspective, HBC would be greatly helpful in patients with severe burns. Right after anesthesia, body heat is transferred to peripheral parts, which possess a little lower temperature from the core parts because of vasodilatations by anesthetics, thereby occurring redistribution hypothermia that the core temperature decreases. This phenomenon lasts for an hour and the core temperature decreases by approximately 1-1.5℃ in the period. Afterward, the body temperature descends almost straightly by more than 3℃ for 2-3 hours, so that it finally reaches the plateau [9]. Besides, radiation due to the lower atmospheric temperature than that of body temperature, electric heat caused by surgical drapes, and evaporation from the surgical wounds are also the factors determining heat loss. Injection of large volume of cold intravenous fluids also affects temperature changes [10]. Threshold of temperature control in healthy individuals is 36.5-37.5℃; in case of patients with severe burns; however, it is proportional to the burned area. It is known that the threshold increases by approximately 0.03℃ per total body surface area. As such, in case of burns with more than 25%, the threshold is estimated to elevate by 0.75℃ approximately [3]. For such reasons, patients with severe burns feel tremble and discomfort at 36.5℃ and may have vasoconstriction in order to maintain higher body temperature. Hypothermia that occurs during anesthesia, even if it is mild, causes many complications, such as wound infection, extending the period of hospitalization, serious cardiac complications, clotting disorders, and delay the discharge from a recovery room [10]. When hypothermia after anesthesia is recovered slowly in patients with severe burns, it leads to an increase of mortality rate [3]. This is because that surgery in patients with severe burns of 25% total body surface area may have a great amount of blood loss during a large area of skin tissue removal; also as the wound is spread widely, wound infection and blood clotting disorders, if occurring, are lethal. Therefore, careful monitoring and controlling of body temperature and vital signs are essential for safe anesthesia during the surgery of burned patients. About 90% of metabolic heat dissipates through the surface of the skin and only less than 10% dissipates via respiratory system. Hence, there is no doubt that the effects of heating and dehumidification of airway on maintaining body temperature are limited. Considering the mechanisms of redistribution hypothermia, the best way to maintain body temperature is by either heating the entire body before anesthesia or heating the skin during surgery. However, not only it is practically difficult and dangerous to heat the patients with severe burns whose body temperature has already elevated prior to surgery but also skin heating is unavailable in the case as the surgery is carried out while their entire body is disinfected and exposed without any surgical drapes. Due to such reasons, we made efforts to keep the temperature of the operating room higher than 30℃ and heat all fluids, including disinfecting fluids, that were injected to the patients; however, temperature drop was not completely inhibited. Thus, it was expected that the breathing circuit with heating function would reduce the temperature drop as described in other studies [4,5]; but there was no effect observed in this study. This would be because of the body exposure during the surgery due to extensive skin loss in the burned patients. Even if warm disinfecting fluids are spread throughout the whole body when performing either escharectomy or skin graft, surrounding temperature is maximum 32℃, which is much lower than body temperature; hence, the heat of the body dissipates as the disinfecting fluids evaporate and radiation and conduction proceeds. In this condition, the maintained temperature was not significantly effective compared to the conventional breathing circuit, even though additional heat was applied to maintain them. However, body temperature in patients without burns during anesthesia decreased by 1-1.5℃ within an hour and further by more than 3℃ up till 3 hours; in contrast, the present study was found that the control group and the HBC group showed decreases just by 0.5 ± 0.5℃ and 0.5 ± 0.4℃ at 60 minute anesthesia, and 1.3 ± 0.8℃ and 0.9 ± 0.6℃ at 180 minute anesthesia, respectively. This may be caused by the effects of the various heating methods, including high temperature of the operating room. A study in patients with general anesthesia for lower abdominal surgery [6] reported that HBC didn't successfully reduce the temperature drop. They also explained the reasons for the exposure of the surgical sites; exposure of lower abdomen, which is the core of the body that causes heat loss as much as counterbalancing the heat in respiratory system. On the other hand, in a study reporting that HBC was effective on the body temperature maintenance [5], the types of surgery was not notified. In case where several types of surgery were included, the results might not be accurate since the body exposure would not be constantly controlled. Another study investigated [4] that HBC would decrease the temperature drop in early anesthesia compared to that of conventional circuit by reducing the heat loss due to airway evaporation and conduction in the early stage of hypothermia. The study was carried out in patients who received spinal surgery. After anesthesia, limbs and hips except for backs, the surgical sites, were heated in face-down positions utilizing forced air-warmer at 40-42℃. In result, the temperature drop 60 minutes after anesthesia was greater in the experimental group, but it was similar between the two groups up till 3 hours. In addition, the average temperature drop was approximately 1℃; it was also thought to be because of the additional heating device. Although it is difficult to conclude clearly, given the lack of information regarding the temperature of the operation room in the study, it seems that differences between the results might be because the temperature of the operation room of the present study is generally higher than others, so that it offsets the effects of HBC, thereby affecting the temperature drop of early anesthesia in both groups. Limitation of this study is that the effects of HBC only on body temperature are not able to be compared because of utilization of various heating methods, as mentioned previously. However, this study was considered to be reasonable because the effects of additional heating from breathing circuit were investigated under the same heating conditions in both groups and in the optimum environment to maintain body temperature of the patients for safety. In conclusion, the present study confirmed that HBC utilization during general anesthesia in patients with severe burns did not result in significant reduction of the core temperature drop during surgery. However, the humidity of the inspired gases was capable to be maintained ideally. In the future, more studies may need to be done regarding the methods to reduce the core temperature when performing anesthesia in patients with severe burns during surgery.