Hemodynamic effects of continuous intravenous injection and bolus plus continuous intravenous injection of oxytocin in cesarean section
Article information
Abstract
Background
Oxytocin may cause adverse cardiovascular effects, including tachycardia and hypotension, whereas the optimal dose of oxytocin at elective cesarean section is unclear. To determine the lowest effective dose of oxytocin, we studied the hemodynamic effects of three doses during spinal anesthesia for elective single cesarean delivery.
Methods
Sixty women received oxytocin by continuous (0.5 IU/min) or bolus-continuous (2 or 5 IU prior to 0.25 IU/min continuous intravenous injection) intravenous injection after clamping of the umbilical cord. We compared changes in heart rate (HR), mean arterial pressure (MAP) and estimated blood loss (EBL). Uterine tone (UT) was assessed by palpation on a linear analog scale (LAS) at 5, 10, 15, 20 and 25 minutes after the oxytocin injection. In addition, oxytocin-related side-effects such as nausea and vomiting were recorded.
Results
Marked hemodynamic changes such as HR and MAP occurred in the bolus-continuous groups but not in the continuous groups. Although we were not able to observe a variation of EBL in each group, the UT significantly increased in the bolus-continuous groups when compared with that the continuous groups. In addition, the hemodynamic changes such as HR and MAP were lower in the two IU bolus-continuous group than those in the five IU group.
Conclusions
Although bolus-continuous injection of oxytocin resulted in more hemodynamic changes than continuous injection, bolus-continuous injection had a greater effect on uterine contraction. Furthermore, two IU bolus-continuous injection showed lower hemodynamic changes than in the five IU bolus-continuous injection.
Introduction
The hemodynamic changes in parturient women after cesarean delivery may be caused by the elimination of the aorta-caval compression, autotransfusion of uterine contraction, hemorrhage, and vasoconstriction and excitation, but some studies have reported that uterotonic drug is the main factor [1,2]. Uterotonic drug, which is most frequently used for cesarean section, is oxytocin, which induces uterine contraction during cesarean section and peripheral vasodilation along with a decrease in arterial pressure after delivery and thus, reduces hemorrhage [3,4]. However, intravenous injection of oxytocin during cesarean section may cause cardiovascular side effects such as tachycardia or hypotension [1,2] and is reported to cause even cardiovascular collapse and death in the most severe cases [5,6]. Moreover, various other side effects have been reported including fluid pooling or pulmonary edema by the antidiuretic effect of oxytocin [7-9].
Hence, determining the oxytocin concentration for cesarean section is important. However, since the activity of oxytocin varies from individual to individual [10] and an appropriate dose has not been established, 5-20 IU is intravenously injected based on experience [11,12]. There is a recent assertion that bolus intravenous injection or bolus-continuous parallel intravenous injection of oxytocin is more effective than continuous intravenous injection in cesarean section [13,14]. There is also a report that a great quantity of bolus intravenous injection requires caution because it causes hemodynamic changes related to hypotension [1,2]. Therefore, research is necessary on the method of oxytocin injection and the effective minimum concentration for cesarean section to induce uterine contraction without side effects.
In this study, we did continuous intravenous injection or bolus-continuous intravenous injection of oxytocin after clamping of the umbilical cord during planned cesarean sections under spinal anesthesia, and investigated the uterine tone (TU) and hemodynamic changes.
Materials and Methods
This study was approved by the Hospital Ethics Committee. The subjects of this study were 60 singleton gestation pregnant women who were 38 weeks or more into their pregnancy, and were classified as Class 1 or 2 according to the American Society of Anesthesiologist (ASA) physical status classification and were supposed to undergo planned cesarean section under spinal anesthesia in the obstetrics and gynecology department in our hospital. The subjects were visited before the operation and written consent was given by the subjects. Pregnant women who had contraindication for spinal anesthesia, those whose weight was 100 kg or higher, those who had fetal abnormalities, diabetes, gestational hypertension, cardiovascular disease, or cerebral hemorrhage, and those whose labor pain had already started were excluded from the study. The age, height, and weight of the patients were recorded.
About 500 ml of Hartmann solution was rapidly dripped into all the parturient women before inducing anesthesia. An electrocardiograph, automated noninvasive blood pressure device, and a pulse oximeter were attached to the subjects, and oxygen was injected at 5 L/min through a mask. For the spinal anesthesia, the L3-4 or L4-5 lumbar region was punctured with a 25 G Quincke needle when the parturient women were in the left lateral recumbent position, and 0.5% hyperbaric bupivacaine solution (10-12 mg) was injected after verifying the cerebrospinal fluid leakage. Immediately after the anesthesia, the parturient women were asked to take the supine position and the maximum sensory block level was set to T4-6. The blood pressure and HR were measured in five-minute intervals from the time just after the anesthesia started to the end of the operation. However, during the 10 minutes after the oxytocin was injected, the blood pressure and HR were measured in one minute intervals, and delivery of the newborn was set as the baseline. The parturient women were asked if they felt or experienced nausea and vomiting after oxytocin injection and the results were recorded. When some of the parturient women had severe vomiting or continual nausea, the antiemetic drug, ondansetron 8 mg, was intravenously injected. In the cases where the systolic pressure decreased by more than 20% compared to the blood pressure before coming to the operating room, 10 mg of ephedrine was intravenously injected until the blood pressure was normalized, and these cases were excluded from the study.
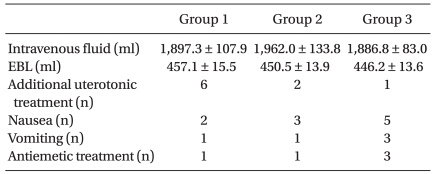
The subjects were randomly divided into three groups, 20 subjects per group. For the oxytocin injection, 5 ml of bolus diluted with normal saline and 40 ml of infusion solution were prepared in advance by a nurse who did not participate in the study. In Group 1, bolus intravenous injection was done for about five seconds with 5 ml of normal saline and then continuous intravenous injection of 20 IU oxytocin diluted with 40 ml of normal saline was done at a rate of 0.5 IU/min for 40 minutes with a syringe pump. In groups 2 and 3, bolus intravenous injection of 2 IU and 5 IU of oxytocin diluted with 5 ml of normal saline was done at a rate of 1 ml/sec, and then continuous intravenous injection of 10 IU of oxytocin diluted with 40 ml of normal saline was done at a rate of 0.25 IU/min for 40 minutes with a syringe pump. The epidemiological data did not show a difference in the age, height, weight, and gestation period of the patients among the groups (Table 1). The obstetrician evaluated the degree of uterine contraction on a LAS in which the grade was determined from a grade of o to 10 (0 = completely atonic, 10 = fully contracted) [15] at five-minute intervals during the operation for 25 minutes from the time just after the newborn was delivered. In the cases where the uterine contraction was considered as insufficient during the operation, intravenously injection of 0.2 mg of methylergonovine was done by the request of the obstetrician, diluting it with normal saline and slowly injecting it over one to two minutes with careful monitoring of the blood pressure. The blood loss was estimated by measuring the weight of the suction bottle and gauze excluding the amniotic fluid.
All the measured values obtained in the experiment were presented as the mean ± standard deviation and 'n.' ANOVA was done to compare age, weight, height, gestational age, fluid injection, and blood loss among the groups. An ANOVA was also performed to compare the HR and MAP among the group. To compare the degree of uterine contraction among the groups, Kruskal-Wallis test, a nonparametric method, was done. A repeated measures ANOVA was done to compare the HR, MAP, and degree of uterine contraction within a group. The Bonferroni method was used for the post-hoc test of the HR and MAP, and the Bonferroni correction was done for the post-hoc test of the degree of uterine contraction. A chi-square correlation analysis was done for each group to compare the frequency of vomiting and nausea and the number of times an antiemetic drug was used. All the statistical analyses were done with SPSS 15.0 (SPSS Inc., Chicago, IL, USA), with a significance level of 0.05.
Results
There was no significant difference in the age, weight, height, and gestational age among the groups (P > 0.05). Hemorrhage was 457.1 ± 15.5 ml in Group 1, 450.5 ± 13.9 ml in Group 2, and 446.2 ± 13.6 ml in Group 3, with no significant difference (P > 0.05, Table 1). The quantity of fluid injected during the operation was almost the same in all the groups, with no significant difference. The number of parturient women who experienced nausea and vomiting after intravenous injection of oxytocin and had antiemetic drugs administered was greater in groups 1 and 2 than in Group 3, but there was no significant difference among the groups (P > 0.05). On the other hand, additional intravenous injection of uterotonic drug was required more in groups 2 and 3 than in Group1, but there was no significant difference among the groups (P > 0.05, Table 2).
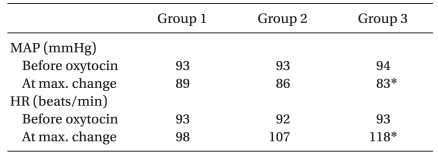
The MAP was similar before the oxytocin intravenous injection. A maximum decrease of 4.5% was observed in Group 1 two minutes after intravenous injection of oxytocin whereas it was 7.6% and 11.8% in groups 2 and 3, respectively, one minute after injection. However, the comparison within the groups showed that the maximum decrease was significant only in Group 3 (P < 0.05, Table 3). There was no case where a hypertensor was used because of hypotension. The MAP decreased after intravenous injection of oxytocin and recovered after four minutes in each group. The comparison among the groups showed that the decrease in groups 2 and 3 at one minute after the injection was significantly greater than that in Group 1, and the decrease in Group 3 was significantly greater than that in Group 2 (P < 0.05, Fig. 1).

Change of maternal mean arterial pressure (MAP) after oxytocin injection during Cesarean delivery. Oxytocin was injected in the following doses; Group 1: 0.5 IU/min continuous injection, Group 2: 2 IU bolus-continuous injection, Group 3: 5 IU boluscontinuous injection. *P < 0.05 compared with each group after oxytocin injection.
The HR in each group was similar before the intravenous injection of oxytocin. A maximum increase of 7.6% was observed in Group 1 two minutes after intravenous injection of oxytocin while it was 17.0% and 26.1% in groups 2 and 3, respectively, one minute after the injection, but the increase was significant only in Group 3 (P < 0.05, Table 3). The comparison among the groups showed that the increase at one, two and three minutes after the injection was significantly greater in groups 2 and 3 than that in Group 1, and the increase in Group 3 was significantly greater than that in Group 2. The increased HR recovered after five minutes in each group.
The degree of uterine contraction at five and ten minutes after the injection of oxytocin was significantly higher in groups 2 and 3 than that in Group 1 according to the LAS score based on the palpation of the obstetrician (P < 0.05). Particularly in Group 1, the LAS score at five minutes after the injection of oxytocin was 8.0, indicating the failure to obtain an appropriate degree of uterine contraction, and thus, another 30% of additional uterotonic drug by intravenous injection was required. All the groups maintained an appropriate state of uterine contraction at ten minutes after the injection, and thereafter, no uterotonic drug by intravenous injection was additionally done because of re-relaxation.
Discussion
Oxytocin, a hormone that is secreted from the pituitary posterior lobe, decreases blood pressure by causing peripheral vasodilation and increasing the HR and induces uterine contraction [3,4]. Uterine contraction by oxytocin is enhanced since there are more intrauterine oxytocin receptors [16]. The oxytocin sensitivity of pregnant women reaches the maximum in the full term of the pregnancy because of the increase of intrauterine oxytocin receptors by gestational estrogen [10]. Hence, during normal delivery, the oxytocin discharged from the pituitary posterior lobe by the obstetric canal stimulus of the fetus can induce labor pain and sufficient uterine contraction with an extreme low-dose of 10 mIU/min [17]. In the case of a planned cesarean section, however, a relatively high-dose of oxytocin (5-20 IU) is intravenously injected since the action of the oxytocin is not normal [11,12]. Since hemodynamic changes are proportional to the intravenously injected dose of oxytocin, studies have been done on effective concentrations and intravenous injection methods.
Sarna et al. [11] reported that oxytocin infusion at a rate of 1 IU/min did not show any difference in uterine contraction and blood loss with that of 5 IU by intravenous injection even though the total dose may have been more than 5 IU. Kim et al. [12] published the same assertion. On the contrary, Zarzur [18] recommended an infusion at a rate lower than 1 IU/min because infusion at a rate higher than 0.25 IU/min may cause such symptoms as hemangiectatic hypotension, tachycardia, increased cardiac output, and myocardial ischemia. In Group 1, in this study, where the infusion was done at the rate of 0.5 IU/min, there was no significant hemodynamic change due to the infusion of oxytocin, but about another 30% of additional uterotonic drug was required for parturient women to obtain an appropriate degree of uterine contraction.
According to many recent studies, oxytocin bolus injection was reported to be more effective than infusion by intravenous injection to reduce blood loss by inducing the appropriate uterine contraction [13], and thus, the minimum bolus dose has been discussed [19-21]. A suggested method to reduce hemodynamic changes is the repeated intravenous injections of a small quantity of a bolus dose and bolus-continuous parallel intravenous injection [14,22]. Svanstrom et al. [6] stated that attention is required because a bolus injection of 10 IU oxytocin may cause temporary hypotension and tachycardia as well as myocardial ischemia, apart from the operation, pregnancy, and autonomic blocking by spinal anesthesia. Pinder et al. [2] recommended 5 IU as the bolus dose since 10 IU of bolus intravenous injection caused severe hemodynamic changes, but they stated that the dose might not be considered as safe, either. On the contrary, Butwick et al. [20] asserted that a dose of more than 5 IU might not be necessary because appropriate uterine contraction occurred even with a bolus dose of 0.5-3 IU. Sartain et al. [14] injected 2 IU and 5 IU of bolus doses, which are the same doses for groups 2 and 3 in our experiment and reported that the use of 2 IU was more effective because the hemodynamic changes were more severe in the 5 IU group even though the uterine contraction were similar in the two groups. These results were similar to our results and the hemodynamic changes were always temporary.
In the case of Group 3 in which 5 IU bolus-continuous intravenous injection was done, the MAP and HR were significantly decreased by 11.8% and significantly increased by 26.1%, respectively, at one minute after the injection of oxytocin. On the contrary, the MAP and HR were not significantly changed in Group 2 in which 2 IU bolus-continuous intravenous injection was done (Fig. 1, 2, Table 3). Thus, it was found that the hemodynamic changes varied by the bolus injected oxytocin dose and changes were recovered from in about 4-5 minutes after oxytocin injection. As shown in this study, delivery of the newborn and the following excitement may affect the HR because parturient women are conscious during cesarean section under spinal anesthesia. However, the main factor of the changes may be the effect of oxytocin itself.

Change of heart rate (HR) after oxytocin injection during Cesarean delivery. Oxytocin was injected in the following doses; Group 1: 0.5 IU/min continuous injection, Group 2: 2 IU boluscontinuous injection, Group 3: 5 IU bolus-continuous injection. *P < 0.05 compared with each group after oxytocin injection.
The half-life of oxytocin is about 5-12 minutes and a blood steady state is reached in about 30-60 minutes after intravenous injection [23,24]. Thus, the oxytocin dose and injection method play an important role in the hemodynamic changes before a steady state is reached. These hemodynamic changes by oxytocin are always temporary and the effect on healthy parturient women is small. However, they may be dangerous to parturient women who have hypovolemia or cardiovascular diseases. Hence, continuous intravenous injection of oxytocin at a low concentration is primarily recommended as a safe injection method for parturient women in a high-risk group [1,2]. Nevertheless, repeated bolus intravenous injection with a small quantity of bolus or parallel intravenous injection of a small quantity of bolus plus continuous injection is also used because of the rapid desensitization by which the hemodynamic changes are significantly decreased in the repeated oxytocin than in the initial injection [14,22]. In our study, a longer time was taken in the continuous intravenous injection group (Group 1) to induce the appropriate uterine contraction with a LAS score of 8.0 than the bolus-continuous parallel intravenous injection groups (groups 2 and 3), and about another 30% of additional uterotonic drug was required in Group 1, but there was no significant difference in the mean blood loss. Nausea and vomiting occurred more in Group 3, but the difference was not significant (Table 2, Fig. 3).

Prevalence of adequate uterine tone (UT) by linear analog scale (LAS) after oxytocin injection during Cesarean delivery. Oxytocin was injected in the following doses; Group 1: 0.5 IU/min continuous injection, Group 2: 2 IU bolus-continuous injection, Group 3: 5 IU bolus-continuous injection. Numerical scores for UT were assessed by the obstetrician using a linear analog scale of 0 (absent UT) to 10 (optimal UT). *P < 0.05 compared with each group after oxytocin injection.
In conclusion, with parturient women undergoing planned cesarean section under spinal anesthesia, infusion of 20 IU of oxytocin was done at a rate of 0.5 IU/min, and 2 IU or 5 IU bolus intravenous injection followed by 10 IU oxytocin intravenous injection at a rate of 0.25 IU/min were done immediately after clamping of the umbilical cord following delivery of the new born, and the results show that a more effective uterine contraction occurred in the bolus-continuous parallel intravenous injection group accompanied by a decreased MAP and increased mean HR which were significantly higher in the 2 IU bolus-continuous parallel intravenous injection group than in the 5 IU bolus-continuous parallel intravenous injection group. These changes may have little effect on healthy parturient women because they can recover within about 4-5 minutes after intravenous injection of oxytocin, as in this study, but the methods that cause the changes are difficult to interpret in women who have uterine atony such as premature separation of placenta or placenta accrete. Although a low-dose bolus intravenous injection may be appropriate to meet the demand of obstetricians who want rapid uterine contraction, they should be careful when using this method in parturient women who are suspected to have hypovolemia or cardiovascular diseases because bolus-continuous parallel intravenous injection of 2 IU oxytocin is accompanied by hemodynamic changes in MAP and HR though they may be relatively mild. Further studies need to be conducted on low-dose intravenous injection with less than 2 IU oxytocin in order to obtain more stable and objective data.