The effect of milrinone infusion on right ventricular function during coronary anastomosis and early outcomes in patients undergoing off-pump coronary artery bypass surgery
Article information
Abstract
Background
During coronary anastomosis in off-pump coronary artery bypass surgery (OPCAB), hemodynamic alternations can be induced by impaired diastolic function of the right ventricle. This study was designed to examine the effect of milrinone on right ventricular function and early outcomes in patients undergoing OPCAB.
Methods
Forty patients undergoing OPCAB were randomly assigned in a double-blind manner to receive either milrinone (milrinone group, n = 20) or normal saline (control group, n = 20). Hemodynamic variables were measured after pericardiotomy (T1), 5 min after stabilizer application for anastomosis of the left anterior descending coronary artery (LAD, T2), the obtuse marginalis branch (OM, T3), the right coronary artery (RCA, T4), 5 min after sternal closure (T5), and after ICU arrival. The right ventricular ejection fraction (RVEF) and right ventricular volumetric parameters were also measured using the thermodilution technique. For evaluation of early outcomes, the 30-day operative mortality and morbidity risk models were used.
Results
There was no significant difference in hemodynamic variables, including mean arterial pressure, between the 2 groups, except for the cardiac index and RVEF. The cardiac index and RVEF were significantly greater at T3 in the milrinone group than in the control group.
Conclusions
Continuous infusion of milrinone demonstrated a beneficial effect on cardiac output and right ventricular function in patients undergoing OPCAB, especially during anastomosis of the graft to the OM artery, and it had no adverse effect on early outcomes.
Introduction
Off-pump coronary artery bypass surgery (OPCAB) is widely performed for its benefit in reducing complications from cardiopulmonary bypass [1-3]. However, since the surgical method moves the pumping heart and limits movement of the surgery site with a tissue stabilizer, it can cause serious hemodynamic changes [4,5]. For example, the function of both ventricles declines due to pressure on the heart during OPCAB via diastolic dysfunction of the right ventricle due to pressure [6,7].
Milrinone, a phosphodiesterase III inhibitor, prevents degradation of cyclic adenosine monophosphate in cardiac myocytes to increase contractile force of the heart muscle, and it relaxes the vascular smooth muscle to reduce systemic vascular resistance [8]. Milrinone helps patients avoid cardiopulmonary bypass by increasing heart function. It also enhances cardiac contractility while not increasing oxygen requirements, unlike dobutamine, and prevents vasospasm during coronary anastomosis [9]. In an animal study in canines with pulmonary hypertension, milrinone significantly improved right ventricular function and reduced pulmonary vascular resistance to improve pulmonary blood flow [10]. Milrinone also prevents reduced cardiac output and mixed venous oxygen saturation in OPCAB [11], and studies on patients with low right ventricular function show that milrinone increases the cardiac index while reducing systemic vascular resistance, showing a beneficial role in improving right ventricular function [12].
There is no research on the effects of milrinone on hemodynamic changes or even on early intensive care unit (ICU) outcomes during and after OPCAB. Lowered function of the right ventricle accompanied by heart failure increases the mortality rate [13-15], but no study has been conducted in OPCAB patients. We therefore evaluated the impact of continuous milrinone infusion using a multi-lumen cardiac thermodilution catheter on hemodynamic changes, right ventricular function, and early outcome hemodynamics.
Materials and Methods
This study was authorized by the Institutional Review Board and was conducted with OPCAB patients after written consent, before giving them anesthetic. A pilot study showed that continuous infusion of milrinone reduced the right ventricular ejection fraction (RVEF) by 20% during anastomosis of the obtuse marginal branch. This result was considered meaningful, and when setting the effect size at 0.95, α error at 0.05, and β power at 0.8, 19 patients are required for each group. Considering a dropout rate of 5% from the authors' other clinical experiences, the studies were conducted with 20 patients in each group, 40 in total.
Exclusion criteria included left or right ventricular ejection fraction of less than 40% from the transthoracic echocardiogram before surgery, valvular heart disease, severe cerebral or renal dysfunction, or emergency surgery. Patients with stenosis at more than 3 coronary arteries were selected. An hour before arriving at the operating rooms, all patients received an intramuscular injection of morphine, 0.05-0.1 mg/kg, as preliminary anesthesia, and other drugs, except digoxin and diuretics, as normal. After arriving at the operating room, the induction of lead II and V5 was continuously monitored by 5-leads electrocardiography, and a catheter was inserted by radial artery puncture for continuous monitoring of hemodynamics and arterial blood sampling. A pulmonary catheter (Swan-Ganz CCOmbo® CCO/SvO2/CEDV, Edwards Lifesciences LLC, Irvine, CA, USA), which can continuously monitor cardiac output of the right internal jugular vein, mixed venous oxygen saturation, the right ventricular ejection fraction, and right ventricular end-diastolic volume index, was inserted through an 9F introducer (AVA HF, Edwards Lifesciences, CA, USA) and monitored using a computerized monitoring system (Vigilance® CCO/SvO2/CEDV Monitor, Edwards Lifesciences, CA, USA).
For inducing anesthesia, endotracheal intubation was performed after giving intravenous injections of midazolam 2.5 mg, sufentanil 1.5-3.0 µg/kg, and rocuronium bromide 50 mg. To maintain anesthesia, sufentanil (0.5-1.5 µg/kg/h) and vecuronium were continuously administered intravenously with 50% oxygen and 50% medical air, as well as sevoflurane with an end-tidal concentration of 0.2-0.4 vol%, and controlled ventilation was conducted to set the end-tidal CO2 tension at 30-35 mmHg. After inducing anesthesia, isosorbide dinitrate (0.5 µg/kg/min) was administered to prevent myocardial ischemia and coronary vasospasm, and a transesophageal echocardiography probe was inserted to continuously monitor cardiac movement from a short-axis mid-papillary muscle view, which shows the left ventricular papillary muscle, or a 4- or 2-chamber view if monitoring was difficult. Moreover, the temperature of the operating room was kept at over 20℃. To maintain blood temperature, as measured by pulmonary artery catheter, at over 35.5℃, a warm mattress, warming blanket, infusion blood warmer, and humidifier with heated wire breathing circuit were used. During dissection of the internal mammary artery for a graft after median sternotomy, an infusion solution of 1,500-2,000 ml was injected for 2 hours to maintain preload of the heart, and then the infusion solution was injected intravenously at a speed of 6-8 ml/kg/hr to keep the volume at a similar level as post-anesthesia induction while monitoring the left ventricular end-diastolic volume from echocardiography. After performing sternotomy, patients received saline (n=20, controls) or milrinone (n=20, Sanofi, Korea) 0.5 µg/kg/min during coronary artery anastomosis. After finishing the dissection of the internal mammary artery, heparin 1 mg/kg was injected intravenously and activated coagulation time was maintained at over 250 seconds. The heart was elevated using a pericardial suture and gauze and rotated to clear vision, and then the movement of blood vessels for vascular anastomosis was prevented with the Octopus Tissue Stabilization system®, Medtronic Inc. USA. Vascular anastomosis was started with the left anterior descending artery (LAD), obtuse marginal branch (OM), and right coronary artery (RCA) to the posterior descending artery (PDA); and a shunt (Florester®, Bio-Vascular Co., USA) inside the coronary artery was used to maintain coronary flow during the operation. All procedures were performed by the same cardiac surgeon and anesthesiologist blinded to the treatment groups. For hypotension during proximal anastomosis of each coronary artery, the Trendelenburg position at 15-20° was taken, and for hypotension during elevating heart or anastomosis, norepinephrine (8 µg/ml) was given to keep the mean arterial pressure over 70 mmHg. A measurement of the variables was conducted after pericardiotomy (T1, base value), every 5 minutes after attaching a cardiac tissue stabilizer for anastomosis of the left anterior descending artery, obtuse marginal and posterior descending artery of the right coronary artery (each LAD:T2, OM:T3 and PDA:T4) and after performing sternum closure (T5); and the time of measuring hemodynamic variables in the intensive care unit was immediately, 6 hours after, and 12 hours after arrival in the intensive care unit. Variables included heart rate, mean arterial pressure, central venous pressure, mean pulmonary artery pressure, pulmonary capillary wedge pressure, mixed venous oxygen saturation, cardiac output, right ventricular volume index, and right ventricular ejection fraction. The systemic vascular resistance index and pulmonary vascular resistance index were calculated while recording the administered volume of norepinephrine. Also, to monitor and compare early outcomes, we recorded permanent cerebral infarction for 30 days after the operation, as suggested by the Society of Thoracic Surgeons, renal insufficiency, mechanical ventilation lasting more than 48 hours, deep sternal infection, re-operation, and the mortality rate [16]. Renal failure was defined as when serum creatine increased more than 2.0 after the operation was performed, when it increased more than 50% compared to the base value before the operation, or when dialysis was required. SPSS 12.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and all values are given as the average ± standard deviation or the number of patients. To compare groups, an independent t-test was used for continuous data, and Fisher's exact test and the chi-square test were used to evaluate categorical data. Comparisons between base and measured values over time was conducted with a paired t-test after setting the estimated value as the control value after performing pericardiotomy. P < 0.05 was considered significant.
Results
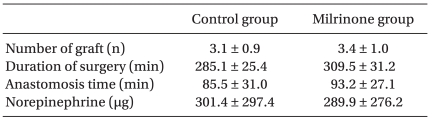
OPCAB was performed successfully without transition to emergency cardiopulmonary bypass. There were no significant statistical differences between the 2 groups for gender, age, medical history of diabetes and hypertension, drug administration, or left ventricle ejection rate (Table 1). The total operation time, coronary artery anastomosis, and total norepinephrine volume were similar for both groups (Table 2). Heart movement and stabilization for anastomosis did not require treatment of arrhythmia.
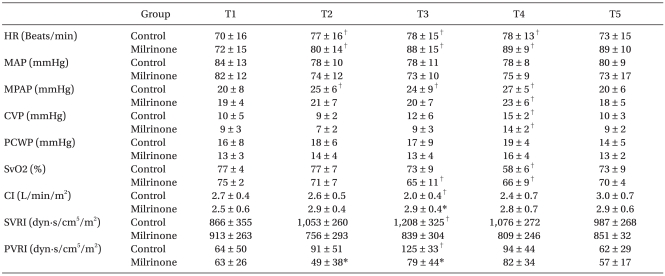
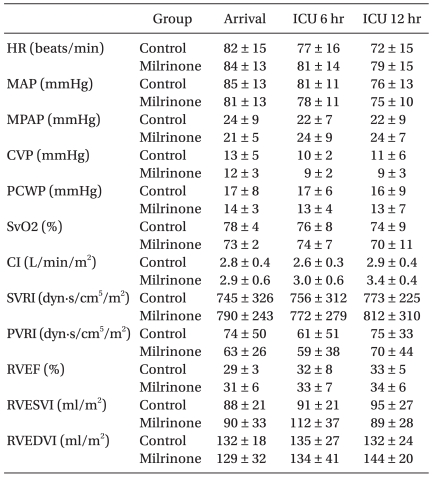
Cardiac index decreased in controls during OM anastomosis, whereas milrinone treatment increased it (P < 0.05, Table 3). Milrinone also blocked the increase in pulmonary vascular resistance index during LAD and OM anastomosis (P < 0.05, Table 3). Milrinone also increased the right ventricular ejection fraction during anastomosis, but did not change other variables (P < 0.05, Table 4). During anastomosis, mean arterial pressure remained steady but heart rate increased with time. Pulmonary artery pressure increased during anastomosis in controls, but only during PDA anastomosis in the milrinone group. Central venous pressure was increased for both groups during PDA anastomosis. Mixed venous oxygen saturation decreased in the milrinone group during OM anastomosis, and in both groups during PDA anastomosis. The cardiac index decreased significantly compared to baseline during OM anastomosis for controls, whereas the systemic vascular resistance index and pulmonary vascular resistance index were increased significantly during OM anastomosis (P < 0.05, Table 3).
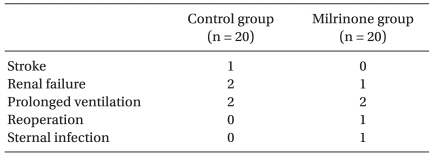
The hemodynamic variables checked immediately after arrival in the ICU, 6 hours after arriving, and 12 hours after arriving did not show significant gaps between the groups (Table 5), and there were no early deaths; both groups showed similar rates of myocardial infarction, cerebral infarction, renal failure, mechanical ventilation lasting more than 48 hours, re-operation, and infections (Table 6).
Discussion
The study focused on the effect of milrinone infusion on right ventricular function during coronary anastomosis and early outcomes in patients undergoing OPCAB. Milrinone infusion prevented reductions in the right ventricular ejection fraction during anastomosis of the obtuse marginal artery, on the posterior slope of the heart, and did not greatly influence early outcomes. OPCAB can reduce the incidence of complications related with external circulation, including pulmonary dysfunction, kidney injury, brain injury, and hematoma, but can cause hemodynamic instability when the heart is elevated and stabilized for the anastomosis [17,18]. Elevating the heart vertically to expose blood vessels for anastomosis decreases cardiac output and blood pressure and increases central venous pressure, but reducing central venous pressure with a pump that delivers blood to the pulmonary artery via cannulation of the right atrium increased right heart function and improved hemodynamic instability in animals [19]. Increasing ventricular preload by postural changes, including the head-down tilt position, helps maintain ventricular function [20]. Dysfunction of the right ventricle from stabilizer pressure can cause hemodynamic disorders during OPCAB, particularly during vascular anastomosis of the posterior border of the heart [21]. For most OPCAB patients, coronary artery anastomosis does not cause serious hemodynamic disorders, but obtuse marginal artery anastomosis on the posterior border of heart can decrease both right and left ventricle function [22,23]; milrinone infusion could block the decreases in cardiac index during obtuse marginal artery anastomosis and the right ventricular ejection fraction. Right ventricle function significantly influences left ventricle function through interdependence, and shows a close interrelationship with congestive heart failure and the short-and-long-term survival rate of OPCAB patients [13,14,24]. Milrinone improved RVEF by enhancing left ventricle function, increasing the cardiac index, and decreasing systemic vascular resistance, as well as improving right ventricular function by blocking increases in pulmonary vascular resistance. Milrinone increases the cardiac index for congestive heart failure patients at plasma concentrations of 66-427 ng/ml [25]. Continuous intravenous injection of milrinone at 0.5 µg/kg/min after bolus injection of 50 µg/kg brought plasma concentrations up to 100 ng/ml, and the infusion rate was appropriate for the treatment of weaning of cardiopulmonary bypass [26]; the milrinone infusion rate of 0.5 µg/kg/min produces plasma concentrations of 100-300 ng/ml. A bolus loading of milrinone ,may cause hypotension [27], but continuous intravenous injection alone (without bolus) can produce effective plasma concentrations within an hour [28]. Milrinone injection was started after sternotomy and reached effective levels because it requires more than 1 hour from excoriating the internal mammal artery to coronary artery anastomosis. Although milrinone can induce hypotension and arrhythmia, we did not observe these side effects here. The RVEF, as estimated by a pulmonary artery catheter using the thermodilution method, reflects right ventricle function with high reliability and reproducibility [29,30]. Thermodilution may be more reliable than transesophageal echocardiography (TEE) [31] for measuring right ventricle function during surgery. The RVEF using a pulmonary artery catheter is sensitive to preload changes, but we did not detect differences in the right ventricular diastole volume index, a measure of preload. OPCAB patients have chronic ischemic heart disease due to a drastic decline of coronary artery blood flow to both ventricles, so transitioning the heart to the coronary artery site for anastomosis would worsen the function of both ventricles by reducing cardiac output [32]. In particular, because the obtuse marginal artery produces more functional disorders than other coronary arteries during anastomosis, intensive monitoring and treatment of ischemic heart disease is required to avoid declines in ventricle function [19]. Milrinone may therefore stabilize ventricle function during obtuse marginal artery anastomosis, as assessed by the RVEF and cardiac index via a pulmonary artery catheter. The Society of Thoracic Surgeons measures early OPCAB outcomes such as mortality rate within 30 days, stroke, renal failure, reoperation, continuous mechanical ventilation, and infection frequency of the sternum [16]. Both groups showed a similar complication rate, indicating that milrinone does not affect early outcomes.
One limitation of our research is that RVEF using a pulmonary artery catheter is very sensitive to preload and afterload, which may change based on patient position. Secondly, complication rates were similar in both groups, but larger studies are needed to confirm this. Thirdly, the time of obtuse marginal artery anastomosis may be less than 10 minutes on average, meaning that it is clinically meaningless for the ischemic preconditioning heart. Lastly, we only included patients with normal left ventricle function, and further work should include patients with abnormal ventricular function.
In conclusion, milrinone infusion during OPCAB surgery blocked reductions in RVEF during obtuse marginal artery anastomosis and maximal levels of hemodynamic instability with similar complication rates as controls.