Non-inflatable supraglottic airways
Article information
As a 1st grade anesthesiologist trainee, I recall seeing the laryngeal mask airway (LMA) for the first time in 1993, and I was surprised at the developer's great idea and design. Today, the variety of supraglottic airways is bewildering and the market for supraglottic airways is extensive in the field of anesthesia and intensive care medicine. It seems that several of these new devices will provide benefits over the classic LMA airway in certain clinical situations; but which devices and when?
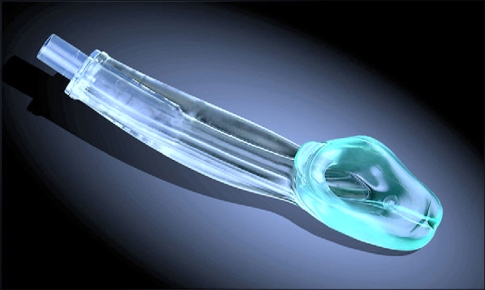
The streamlined liner of pharyngeal airway (SLIPA, Medical Ltd., UK, Fig. 1) is a latex-free supraglottic airway that substitutes for LMA. The manufacturer states that an anatomically preformed SLIPA™ shape lines the pharynx, meaning excellent positive pressure ventilation may be achieved without the cuff inflation that is required in all other airway types [1]. This device meets the need for an inexpensive, disposable, hands free airway that requires minimal expertise for insertion and with a lower risk for aspiration in the event of regurgitation or collection of pharyngeal secretions. There are six adult sizes of SLIPA airway available (47-57) each with a color-coded connector, with numbering indicating the width (in mm) at the bridge of the SLIPA airway and relevant to sizing from the thyroid cartilage.
The SLIPA forms an effective airway that it is as easy to use as a conventional LMA [2]. However, there is an increased risk of gastric inflation with the device, with a 19% incidence of gastric insufflation that may increase the risk of aspiration. This finding raises again issues regarding inflatable or non-inflatable supraglottic airways and choice of sizes. Blood on the device is also more common with SLIPA (20/50 vs. 6/50 with LMA; P = 0.001) and SLIPA insertion increases blood pressure more than LMA [3].
In the Korean Journal of Anesthesiology this month, Choi et al. [4] show that there is a significant rise in hemodynamic responses from the pre-insertion value at one minute after SLIPA insertion, but not for LMA. Further studies may examine these clinical issues with these device and/or new noninflatable supraglottic airways such as i-Gel (Fig. 2).
i-Gel airway designed to create a non-inflatable, anatomical seal of the pharyngeal, laryngeal, and perilaryngeal structures.
