Propofol abuse among healthcare workers: an analysis of criminal cases using the database of the Supreme Court of South Korea’s judgments
Article information
Abstract
Background
Due to its abuse potential, propofol has been classified as a controlled substance since February 2011 in South Korea. Healthcare workers are exposed to propofol abuse considering their easy access to this substance in hospitals. Therefore, we aimed to investigate propofol abuse among healthcare workers through the database of the Supreme Court in South Korea.
Methods
We retrospectively analyzed adjudicated criminal cases related to propofol abuse among healthcare workers from January 1, 2013, to December 31, 2020, using the database of the Supreme Court of South Korea’s judgments. We collected the clinical characteristics and punishment-related information of healthcare workers who abused propofol.
Results
Of the 194 cases collected using the search term ‘propofol,’ 20 were included in the final analysis. The most common healthcare workers who abused propofol were nursing aides (n = 15). Among them, 40% (n = 8) of the defendants had previously been punished for substance abuse, and 35% (n = 7) had a history of psychological disease. Of the defendants, 65% (n = 13) self-administered propofol more than twice, and the median number of self-administrations was three. Except for two, the defendants were sentenced to imprisonment, including suspended sentences, and the median values of their duration of prison and probation were 9 months and 24 months.
Conclusions
Despite propofol being strongly regulated as a controlled substance in South Korea, its abuse among healthcare workers remains. Healthcare workers should be vigilant against its abuse among themselves.
Introduction
Propofol has been the most widely used intravenous hypnotic agent for general anesthesia and sedation; however, it has a risk of abuse [1]. It is known to activate the mesocorticolimbic dopaminergic system through the gamma-aminobutyric acid A receptor, which can contribute to abuse potential [1]. In a prospective study conducted in Korean patients receiving gastric endoscopy, propofol showed a high euphoria effect, which is higher than that of marijuana [2]. According to the practice guidelines for propofol sedation by the Korean Society of Anesthesiologists (KSA), physicians should be acquainted with its abuse potential and carefully evaluate the presence of psychological dependence before administration [3]. Against this backdrop, for the first time worldwide, propofol has been classified as a controlled substance in Korea since February 2011 [4,5]. Moreover, on February 9, 2018, the Korean Ministry of Food and Drug Safety classified propofol as a psychoactive drug of priority control [6]. Currently, details of propofol from manufacturing to sales are required to be reported in the narcotics information management system in South Korea.
Since an anesthesiologist’s first propofol abuse case was reported in 1992 [7], several propofol abuse cases among healthcare workers have been reported [8]. Healthcare workers are more likely to be exposed to propofol abuse than laypeople considering their easy access to this substance in hospitals [4]. They can directly acquire propofol at the hospital where they work or use the remaining propofol after administering it to patients [9]. In the previous peer-reviewed literature between 1992 and 2009, 45 cases of propofol abuse have been reported, of which 40 (89%) were identified in healthcare professionals [8]. In the retrospective cohort study regarding substance use disorder (SUD) among anesthesiology residents in the United States from 1975 to 2009, 384 (2.2%) individuals had confirmed SUD during their residency [10]. Eleven of these individuals reported that the substance used during their initial episode of abuse was propofol [10]. In another retrospective study regarding SUD among anesthesiologists conducted from 2004 to 2013 in Australia and New Zealand, propofol was the most commonly abused medication among anesthesiologists (n = 18/44; 41%) [11].
However, to our knowledge, few studies conducted before 2011—when propofol was not classified as a controlled substance [12,13]—have addressed propofol abuse among healthcare workers in South Korea. According to the recent report published by the Korean Supreme Prosecutors’ Office, the number of medical personnel who committed a crime related to psychoactive drugs increased from 55 in 2016 to 196 in 2020 [14]. Therefore, we aimed to investigate the current state and specific characteristics of propofol abuse among healthcare workers by analyzing adjudicated criminal cases. Further, we aimed to discuss our role as anesthesiologists in preventing its abuse through this study.
Materials and Methods
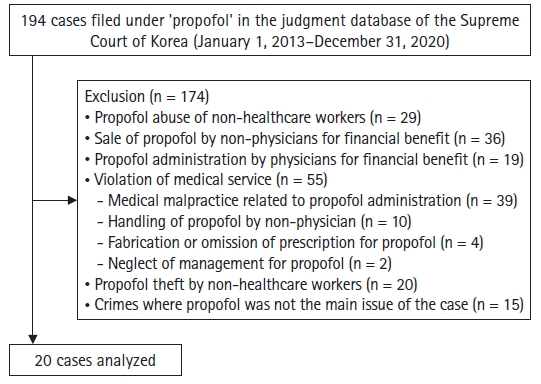
Adjudicated criminal cases that are publicly accessible in the database of the Supreme Court of Korea’s judgments were analyzed. Criminal cases closed from January 1, 2013, can be searched on the Internet through the public service of the Supreme Court of Korea [15]. Without personally identifiable information, the details of each case were provided to the researcher. All criminal cases that were sentenced from January 1, 2013, to December 31, 2020, were searched using the term ‘propofol.’ We included the cases in which the defendant was a healthcare worker and propofol abuser. We excluded cases unrelated to propofol abuse by healthcare workers based on the authors’ judgment (HY Cho and H-J Lee). After the initial analysis, we judged that there were cases indirectly related to propofol abuse among the cases excluded from this study. Therefore, we additionally classified the excluded cases as follows: propofol abuse of non-healthcare workers, sale of propofol by non-physicians for financial benefit, propofol administration by physicians for financial benefit, violation of medical service, propofol theft by non-healthcare workers, and crimes where propofol was not the main issue of the case. This study was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (IRB no. 2111-125-1275), which waived the need for informed consent due to the nature of the study.
In each lawsuit text, a detailed description of the case and the court decisions regarding criminal punishment were observed. The judgment texts were reviewed by two board-certified anesthesiologists (HY Cho and H-J Lee), who collected the following information independently: type of violation, the criminal record of drug abuse, history of psychological diseases, route of propofol acquisition, number of propofol administrations, use of illegal drugs other than propofol, and punishment-related information (prison sentence, suspended sentence, and penalty). In the case of a disagreement between the two authors, the decision was made after a discussion with a third author (SH Shin).
Using the MedCalc Statistical Software version 18.6 (MedCalc Software bvba, Belgium), descriptive statistics were used. Continuous and categorical data are described as median (Q1, Q3) or mean ± SD and percentages, respectively.
Results
There were 194 cases during the study period, 20 of which were related to propofol abuse by healthcare workers (Fig. 1). Among the excluded cases, 19 involved physicians administering propofol to their patients for financial benefit. In the two cases, the physician was fined Korean Won 5,000,000 for neglecting the management of propofol.
Characteristics of the cases are presented in Table 1. The most common healthcare workers who abused propofol were nursing aides (n = 15/20; 75%). The most common location for propofol abuse was a residential area in 65% (n = 13) cases. Of the defendants, 40% (n = 8) had previously been punished for substance abuse, and 65% (n = 13) of the defendants self-administered propofol more than twice (maximum number of self-administrations, 39). The median number of propofol self-administration was three and stolen propofol ampules was 11 (maximum number of stolen propofol ampules, 65). The proportion of defendants who self-administered other drugs with propofol simultaneously (benzodiazepine, n = 5; ketamine, n = 2; fentanyl, n = 2; nalbuphine, n = 1) was 40% (n = 8). In four of the 15 cases of propofol abuse by nursing aides, the residual propofol was stolen after its administration to the patient, while in 11 cases, it was stolen directly from the storage by obtaining its password or stealing the key. There were three physicians who had abused propofol; two of them had a history of conviction for substance abuse (propofol, methamphetamine). Further, two of them had self-administered propofol for stress relief and the third to resolve sleep disturbance.
Judgment statuses are shown in Table 2. The defendants in all cases were punished for violating the narcotics control act, and a theft charge was added in the cases of nursing aides who were not eligible for the management of propofol. Three defendants who had a criminal history of the same offense within the last three years were imprisoned without suspension, and their duration of imprisonment was 4, 12, and 18 months, respectively. The median additional collection amount was 31,796 Korean won—an additional charge for stolen propofol.
Discussion
Although the recognition of the abuse potential of propofol has increased and the control over it has also been strengthened, propofol abuse among healthcare workers still occurs in South Korea. Additionally, although not included in our analyses, other problems associated with propofol abuse, such as propofol trading by a physician, neglect of its management, and propofol theft, were also identified in this study. Considering the increased use of propofol as a sedative agent [16], healthcare workers should be wary of its abuse potential.
Previous studies have reported propofol abuse by non-healthcare professionals as well as healthcare professionals in South Korea. The first study regarding propofol abuse in South Korea was conducted among healthcare professionals working in the operating room [12]. This study was a nationwide survey of 95 councilors of the KSA working at 61 hospitals. In this study, nine propofol abusers working at seven hospitals were identified (anesthesiology resident, n = 4; non-anesthesiology resident, n = 2; nurse in anesthesiology, n = 1; not described, n = 2). In the autopsy study related to propofol abuse in South Korea, nine of the 16 subjects were healthcare professionals (three physicians and six nurses) [17]. Among them, the cause of death in 14 subjects was drug intoxication, and that in two subjects was hanging. In another structured survey conducted on 38 non-healthcare professional propofol abusers, stress relief was the most common reason for the first-time administration of propofol, and most of them had received propofol two or three times a week during the last 12 months [18]. Although our study could not investigate the reason for the first administration of propofol in all cases, the most common cause of its first administration was also stress relief. Additionally, as repeated abuse of controlled substances increases the probability of being apprehended, it was noted that propofol administration continued after the first one in 65% of abusers in our study.
Our study included information related to punishment for propofol abuse that was not covered in previous studies [12,17,18]. The recidivism and number and dosage of abused drugs act as important factors in the judgment regarding drug abuse cases [19]. If the defendant is currently under probation for another criminal offense, a prison sentence is inevitable. In our study, all three imprisoned defendants were under probation due to another drug abuse. Additionally, the probation period is judged to be one and half to two times longer than the prison period in South Korea, and in this study, the mean value of the prison period was 8.5 months and the median value of the total period including the probation and prison periods was 24 months. Additional collection charge was imposed on the defendant according to the price of propofol, which was administered and could not be confiscated.
Recently, a notification system was introduced to notify doctors who inappropriately prescribed propofol based on the predefined criteria regarding propofol prescription to reduce propofol abuse [20]. The predefined criteria included that propofol should be prescribed and administered only for general anesthesia or sedation, and the number of propofol administrations for sedation should not exceed once a month. It also included the appropriate dose of propofol for general anesthesia and sedation [21]. This strong regulation can increase physicians’ awareness of propofol abuse and reduce propofol abuse caused by inappropriate prescription and administration. After implementing this system, the number of inappropriate prescriptions based on the predefined criteria decreased by 64% from 3,815 to 1,371 [22]. However, because this strong regulation can limit the use of propofol in clinical practice, which has advantages as an anesthetic or sedative agent, its advantages and disadvantages should be discussed.
Our results suggest that the following precautionary measures are needed to reduce propofol abuse by healthcare workers. First, handlers of antipsychotics should pay more attention to its management. Despite antipsychotics being stored in a locked place according to the Narcotics Control Act in South Korea, propofol was stored in an uncontrolled place in half of our cases (Table 1). Additionally, we could identify two cases in which doctors were fined for neglecting the management of propofol in the excluded cases. An exhaustive monitoring system is also needed for the remaining amount of propofol after administration to the patient. In four cases in this study, defendants self-administered the remaining propofol after administration to the patient (Table 1). Propofol handlers should pay special attention to the remaining amount of propofol after administration. Second, a systematic treatment and rehabilitation program with the active support of the government should be prepared. In the aforementioned study, five out of the nine propofol abusers had a previous history of drug abuse other than propofol, and only two of the nine abusers participated in the relapse prevention program [12]. In another study, the relapse rate of SUD related to hypnotics in anesthesiology residents has been reported to be 29% [10]. The recidivism rate of the abuse of psychotropic substances has been reported to be 37.2% in South Korea [14], and in our study, 40% of the defendants had a history of substance abuse. Active treatment and rehabilitation of addicted healthcare workers will help prevent their recurrence of substance abuse. However, conflicting results have also been reported for its effectiveness [23,24], and their cost-effectiveness should be discussed. Finally, to fundamentally prevent substance abuse, periodic education on the seriousness of substance abuse is also needed for healthcare workers.
This study has some limitations. First, the judicial cases analyzed did not always contain detailed clinical information, such as the reasons for the first abuse and previous history of psychological disease. Second, our results could not represent all propofol abuse by healthcare workers. The mortality rate of propofol abuse has been reported to be as high as 28% to 38% [1,25], and healthcare workers who died from propofol abuse could not be included in this study. Additionally, we hypothesized that the number of medical personnel legally punished for propofol abuse does not accurately represent the number of medical personnel who actually abuse propofol. According to the aforementioned study, it is estimated that all propofol abusers were not legally punished [12]. As a result, the small number of cases in this study made it difficult to perform additional analyses other than descriptive statistics. Further, the results of our study should be interpreted cautiously because the aforementioned limitation might have resulted in biased results for a specific department of occupation.
In conclusion, our study identified several propofol abuse cases by healthcare workers in South Korea. Despite an increased awareness of propofol abuse and strengthening the regulation on the management of propofol in South Korea, its abuse is steadily occurring. Healthcare workers should be vigilant against the abuse risk of propofol and continue to strive to prevent its abuse among their colleagues.
Acknowledgements
The authors thank Youkang Ko of the Seoul National University School of Law for consultation on legal contents.
Notes
Funding
None.
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Hye-Yeon Cho (Data curation; Formal analysis; Writing – original draft)
Yoonbin Hwang (Data curation)
SuHwan Shin (Conceptualization; Methodology)
Susie Yoon (Writing – review & editing)
Ho-Jin Lee (Conceptualization; Methodology; Writing – review & editing)