Unexpected visualization of the dorsal scapular artery during supraclavicular block
Article information
The presence of the dorsal scapular artery (DSA) within the brachial plexus is a risk factor for complications when performing a supraclavicular block [1]. Vascular puncture-related cardiovascular and cerebrovascular complications can threaten the safety of the patient. Preoperative sonographic assessment, however, can significantly reduce the incidence of such complications.
This letter describes the unexpected visualization of the DSA during pre-operative sonographic assessment in a 60-year-old woman who was scheduled for surgery due to a fracture of the distal radius in January 2021. The DSA, a vessel branching from the subclavian artery, was identified beneath the inferior trunk while attempting to optimize imaging of the corner pocket (Fig. 1). Because the DSA was directly in the needle pathway, the corner pocket approach could not be utilized. Therefore, the intertruncal approach was used to inject between the trunks [2]. We first carefully injected a small amount of local anesthetics consisting of a 1 : 1 mixture of 1% lidocaine and 0.75% ropivacaine to open up to open up the adipose tissue layer between the inferior and middle trunk and subsequently by securing a safe route for needle advancement in the intertruncal plane [3].
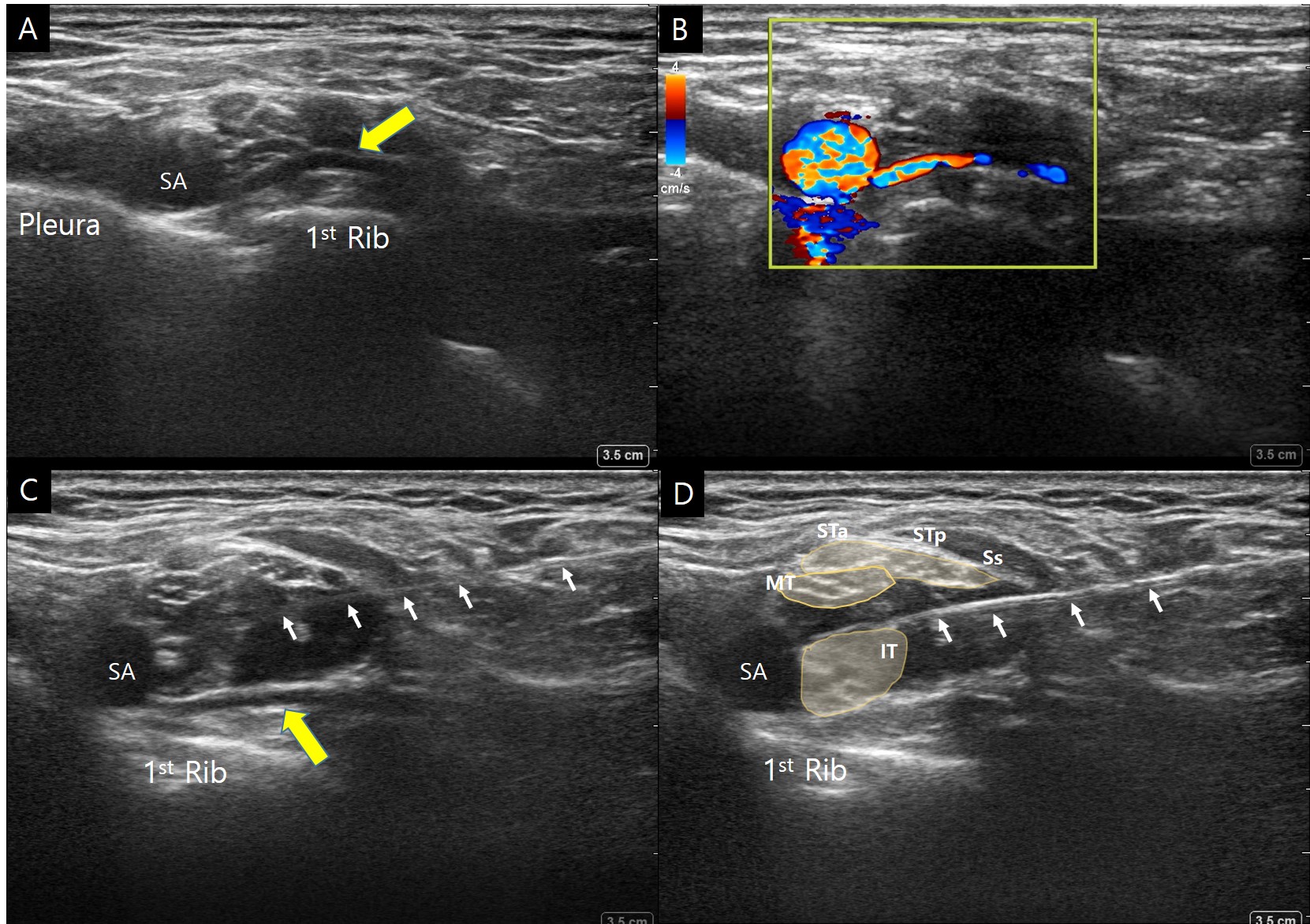
Visualization of the dorsal scapular artery (DSA) while attempting to obtain the optimal sonographic image for the corner pocket block technique. (A) Image showing the DSA (yellow arrow) passing beneath the inferior trunk. (B) Color Doppler image showing that the DSA originated from the subclavian artery. (C) Image showing the needle (small arrows) aimed above the inferior trunk. (D) Image showing the injection of local anesthetics between the inferior and middle trunks. SA: subclavian artery, IT: inferior trunk, MT: middle trunk, Ss: suprascapular nerve, STp: posterior division of the superior trunk, STa: anterior division of the superior trunk.
The DSA often crosses the brachial plexus compartment, mostly between the inferior and middle trunk or between the middle and superior trunk [4]. Although this may increase the risk of vascular-related complications, the DSA has been rarely visualized on optimal sonographic images for the corner pocket approach [5]. If the DSA crosses beneath the first thoracic nerve root, as in the present patient, it lies directly in the path of the needle when performing the corner pocket approach. Moreover, the DSA has been reported to pass beneath the inferior trunk in 6.6% of cadavers [4]. Thus, although this condition is relatively uncommon, it is important to confirm the absence of the DSA during sonographic pre-assessment before utilizing the corner pocket approach. If the DSA is visible, an alternative technique should be used.
Notes
Funding
This research was supported by the National Research Foundation of Korea (NRF-2019R1G1A1099660).
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Boohwi Hong (Conceptualization; Data curation; Project administration; Resources; Writing – original draft)
Chahyun Oh (Conceptualization; Data curation; Writing – review & editing)
Yumin Jo (Conceptualization; Data curation; Visualization)
Woosuk Chung (Conceptualization; Project administration; Supervision; Writing – original draft; Writing – review & editing)
