Continuous peripheral nerve blocks compared to thoracic epidurals or multimodal analgesia for midline laparotomy: a systematic review and meta-analysis
Article information
Abstract
Background
Continuous peripheral nerve blocks (CPNBs) have been investigated to control pain for abdominal surgery via midline laparotomy while avoiding the adverse events of opioid or epidural analgesia. The review compiles the evidence comparing CPNBs to multimodal and epidural analgesia.
Methods
We conducted a systematic review using broad search terms in MEDLINE, Embase, Cochrane. Primary outcomes were pain scores and cumulative opioid consumption at 48 hours. Secondary outcomes were length of stay and postoperative nausea and vomiting (PONV). We rated the quality of the evidence using Cochrane and GRADE recommendations. The results were synthesized by meta-analysis using Revman.
Results
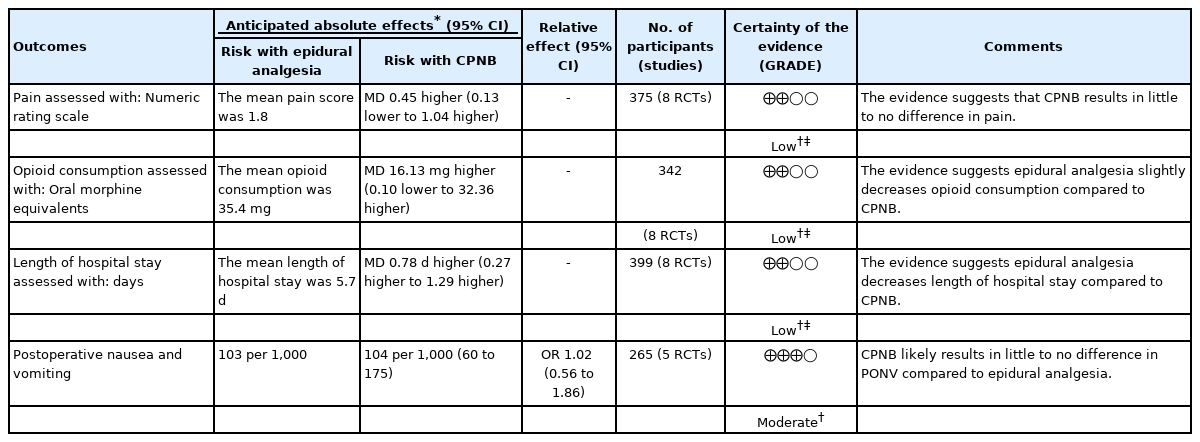
Our final selection included 26 studies (1,646 patients). There was no statistically significant difference in pain control comparing CPNBs to either multimodal or epidural analgesia (low quality evidence). Less opioids were consumed when receiving epidural analgesia than CPNBs (mean difference [MD]: –16.13, 95% CI [–32.36, 0.10]), low quality evidence) and less when receiving CPNBs than multimodal analgesia (MD: –31.52, 95% CI [–42.81, –20.22], low quality evidence). The length of hospital stay was shorter when receiving epidural analgesia than CPNBs (MD: –0.78 days, 95% CI [-1.29, -0.27], low quality evidence) and shorter when receiving CPNBs than multimodal analgesia (MD: -1.41 days, 95% CI [-2.45, -0.36], low quality evidence). There was no statistically significant difference in PONV comparing CPNBs to multimodal (high quality evidence) or epidural analgesia (moderate quality evidence).
Conclusions
CPNBs should be considered a viable alternative to epidural analgesia when contraindications to epidural placement exist for patients undergoing midline laparotomies.
Introduction
It is estimated that 43.8% of the North American population will undergo abdominal surgery during their lifetime [1]. These procedures are associated with high rates of complications, particularly for comorbid or older patients [2]. Many physiologic insults are associated with inadequate pain control [3]. Given that pain increases postoperative morbidity, recovery time, duration of opioid use, health care costs, and quality of life impairment, optimizing pain control can help mitigate the negative consequences of surgery [3].
Open laparotomies, particularly those in the upper abdomen, are associated with respiratory complications if pain is not adequately controlled [4]. The incidence of postoperative pulmonary complications can be as high as 39% in high risk abdominal surgery, with increasing incidence each day that patients are not mobilized [5]. Currently, intravenous opioids are the most common medication for postoperative pain control following surgery [6]. Intravenous opioids attenuate the pain response and associated complications; however, in high doses some complications are exacerbated including respiratory depression, pneumonia, and ileus that in turn contribute to longer hospital stays and higher health care costs [7].
The most common regional anesthetic technique used for abdominal surgery is thoracic epidural [8]. Studies have consistently found that patients using thoracic epidural analgesia experience superior pain control and quality of life after laparotomy [9]. Guidelines for ‘Management of Postoperative Pain’ and ‘Enhanced Recovering After Surgery (ERAS) for Gastrointestinal Surgery’ both strongly recommend thoracic epidural analgesia [10,11]. There is reservation regarding the use of epidurals due to potentially devastating complications, such as epidural hematoma and abscesses [12]. In an attempt to avoid complications from systemic opioids or epidural placement, peripheral nerve blocks have been investigated. Initial reports described single shot nerve blocks that were effective at reducing pain; however, most reduction in opioid consumption occurs within the first 24 h [13,14]. Additionally, these studies do not compare the techniques to each other; thus, their relative efficacy and risk remain unclear.
Previous reviews have compared single shot transversus abdominus plane (TAP) blocks to placebo and wound infiltration [14]. Another review compared paravertebral blocks to epidural catheters, with only four of 20 using continuous catheters [15]. One systematic review examined the analgesic efficacy of wound infiltration compared to epidural analgesia [16]. The review included multiple types of incisions increasing the clinical heterogeneity. The purpose of this review is to determine the relative analgesic efficacy of continuous peripheral nerve blocks (CPNBs) compared to (i) multimodal analgesia and (ii) epidural analgesia in patients undergoing abdominal surgery via a midline laparotomy.
Materials and Methods
Search strategy
Our protocol was registered on PROSPERO (2017, https://www.crd.york.ac.uk/PROSPERO, no. CRD42017051770). at the beginning of the review process. Using broad search terms, we conducted a comprehensive search of three databases: Ovid MEDLINE, Embase, and the Cochrane Library. Our search strategy was developed in consultation with an expert medical librarian. We adapted the search terms used in Ovid MEDLINE (Supplementary Table 1) for other databases. We initially completed the search on November 30, 2016 later repeating it on July 1, 2018.
We did not apply language restrictions to this search. We conducted a search of the grey literature using OpenSIGLE (Supplementary Table 2) and conference abstracts. Once studies were selected for inclusion, a reference search and a forward citation search (using Web of Science) were conducted for each included study.
Inclusion criteria
Population
We included randomized controlled trials (RCTs) and cohort studies involving adult patients (aged > 18 years) undergoing elective abdominal surgery via a midline laparotomy. Urology, general surgery, or vascular surgery procedures performed through an open midline laparotomy were included.
Intervention
We included studies using regional anesthesia techniques to block pain transmission from the peripheral nerves of the abdominal wall. To be included, the technique must have blocked pain transmission on a continuous basis either by continuous infusion of a local anesthetic agent via a catheter for > 48 h, intermittent bolus injection of local anesthetic for > 48 h, or by administering liposomal bupivacaine. We included studies that compared these techniques to 1) continuous epidural analgesia covering the abdominal dermatomes and/or 2) multimodal analgesia with systemic opioids.
Outcomes
The primary outcomes of interest were pain control as measured by a visual analog scale (VAS) or a Numerical Rating Scale (NRS) and opioid consumption at 48 h. All VAS pain scores reported on a scale from 0 to 100 mm were converted to NRS pain scores by dividing by 10. Opioid consumption was compared by converting the reported consumption into oral morphine equivalents (OME) [17]. To be included, studies must have reported either pain scores or opioid consumption up to 48 h postoperatively. Secondary outcomes of interest were length of stay (LOS) in hospital and postoperative nausea and vomiting (PONV).
Exclusion criteria
Studies were excluded if they involved obstetrical, gynecologic, or trauma surgery. Studies involving children (< 18 years) or animals were also excluded. Case studies, case series, and reviews were excluded. If > 20% of patients were treated on an urgent or emergent basis, the study was excluded. Likewise, studies involving > 20% laparoscopic procedures were excluded. Patients undergoing procedures via other incisions were excluded.
Selection procedure
Two investigators (JB, CM) independently reviewed the title, abstract, and full text to assess inclusion and exclusion criteria. If consensus could not be reached between the two investigators, then a third investigator (RC, KK) resolved the disagreement.
Risk-of-bias assessment
We critically appraised each cohort study that met the inclusion criteria for potential biases using a modified version of the quality in prognosis studies (QUIPS) tool for cohort studies [18]. Each RCT was assessed using the Cochrane Risk of Bias Tool [19]. Two of the four investigators (JB, CM, RC, or JK) independently rated each domain in every study [19]. We categorized a study as having a high risk of bias in a domain if the bias was likely to change the results significantly [19].
Once all the studies were assessed independently, the reviewers came to a consensus on each domain. If a consensus was not reached, a third reviewer resolved the disagreement. Funnel plots were created for the primary outcomes to assess for publication bias if more than 10 studies reported a particular outcome. The overall certainty of the evidence was rated using the Cochrane handbook risk-of-bias tool and summarized using GRADEpro software (Evidence Prime, Inc., McMaster University, Canada) [19].
Data extraction
One of the four reviewers (JB, CM, RC, or JK) extracted pertinent data points from each included study using a standardized data extraction form. Each data point was then checked for accuracy by a second reviewer (JB, CM, RC, or JK). If further information or clarification was required, we contacted the corresponding author of the study.
Statistical analysis
We synthesized the data using random-effects meta-analysis with Revman 5.3.5 software (The Nordic Cochrane Centre, Denmark). We analyzed continuous data using inverse-variance mean differences and dichotomous data using Mantel–Haenszel odds ratios. Statistical heterogeneity was assessed using an I2 statistic. Forest plots are displayed and interpreted using mean difference (MD) rather than standardized MD since pain scores were all converted to NRS and all opioid consumption was converted to OME in keeping with the Cochrane recommendations [19]. For any study with three comparison groups, the overall means of the shared control group with half the number of patients were used for comparison as per the Cochrane recommendations [19]. Since this review included various CPNBs, forest plots included subgroup analyses for each CPNB separately. These subgroup analyses were planned to evaluate the relative contribution of each technique toward the combined effect, and to evaluate the efficacy of each CPNB separately.
Our PROSPERO registration included two planned sensitivity analyses. First, any study found to have a high risk of bias in one or more categories would be removed. Since 19 of our 26 studies had at least one high risk of bias category, we modified our sensitivity analysis to remove studies with two or more high risk categories. A sensitivity analysis was performed to examine the effect of upper versus lower midline laparotomy (i.e., above or below the umbilicus) on the primary outcomes. In addition to the planned sensitivity analyses, we conducted additional post-hoc sensitivity analyses. We separated the results of those studies using an epidural solution that included opioids. We performed a sensitivity analysis removing cohort studies from the meta-analyses.
Results
Our search strategy yielded 19,889 results. Using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [20], we generated a flow chart of our selection process (Fig. 1). We contacted 31 authors for additional information. Of these authors, nine responded with the specific data we requested [21–29]. One author [30] responded by providing us with the raw anonymized study data. Two authors responded but did not have the data requested. One author declined to provide additional information unless given authorship on this review. Two authors had emails that were not current, and we were unable to reach them.
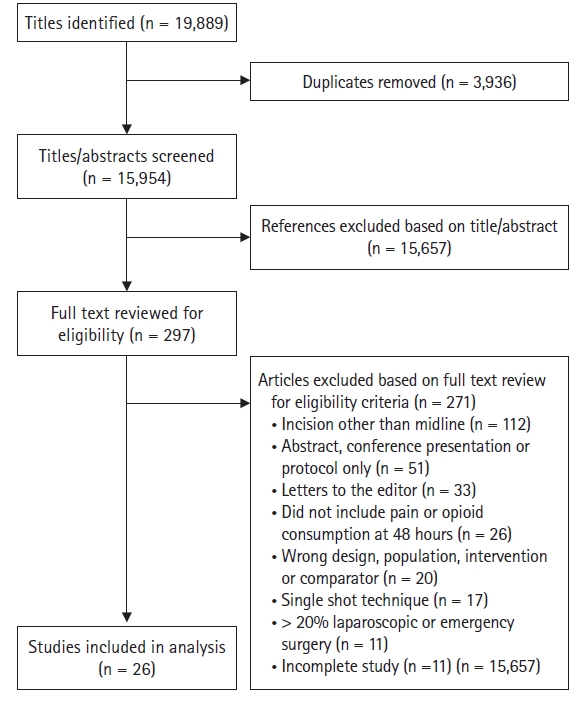
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow chart of included studies.
After title/abstract screening, correspondence with authors, hand-searching, and full-text assessment for eligibility, 26 studies involving 1,646 patients met the final inclusion for this review. Two studies [31,32] were cohort studies, while the rest were RCTs. Two studies [33,34] were divided into two subgroups for a total of 28 comparisons.
Risk of bias
We found that 19 studies had high potential for bias in one domain and, of those, nine had high potential for bias in at least two domains. The most common source of bias was blinding of participants and personnel. Blinding of personnel was considered to be high risk of bias if the study protocol allowed for differential treatment. Random sequence generation was considered to be high risk of bias if the described technique was known to not adequately randomize, whereas studies were rated as moderate or unclear risk of bias if the technique was not adequately described in the paper. Blinding of outcome assessment was deemed high risk of bias if the assessors were aware of the assignment to a study group.
Funnel plots did not suggest publication bias for pain scores or opioid consumption comparing between CPNB and multimodal analgesia (Supplementary Fig. 1). The funnel plots were not created for the comparisons between CPNB and epidural analgesia since there were less than 10 studies.
Multimodal analgesia
The types of multimodal analgesia were not specified a priori in our protocol. Two studies did not describe their multimodal analgesia approach [35,36]. The following agents were used as part of the multimodal analgesia strategy in included studies: Acetaminophen/Paracetamol (20 studies), non-specific NSAIDs (12 studies), COX-2 inhibitors (four studies), gabapentin (three studies), and tramadol (three studies). In two studies, both the intervention and control groups were provided with patient-controlled epidural analgesia [25,37]. These studies were considered multimodal in this review. The intervention group also received epidurals, lessening the potential effect of the CPNB.
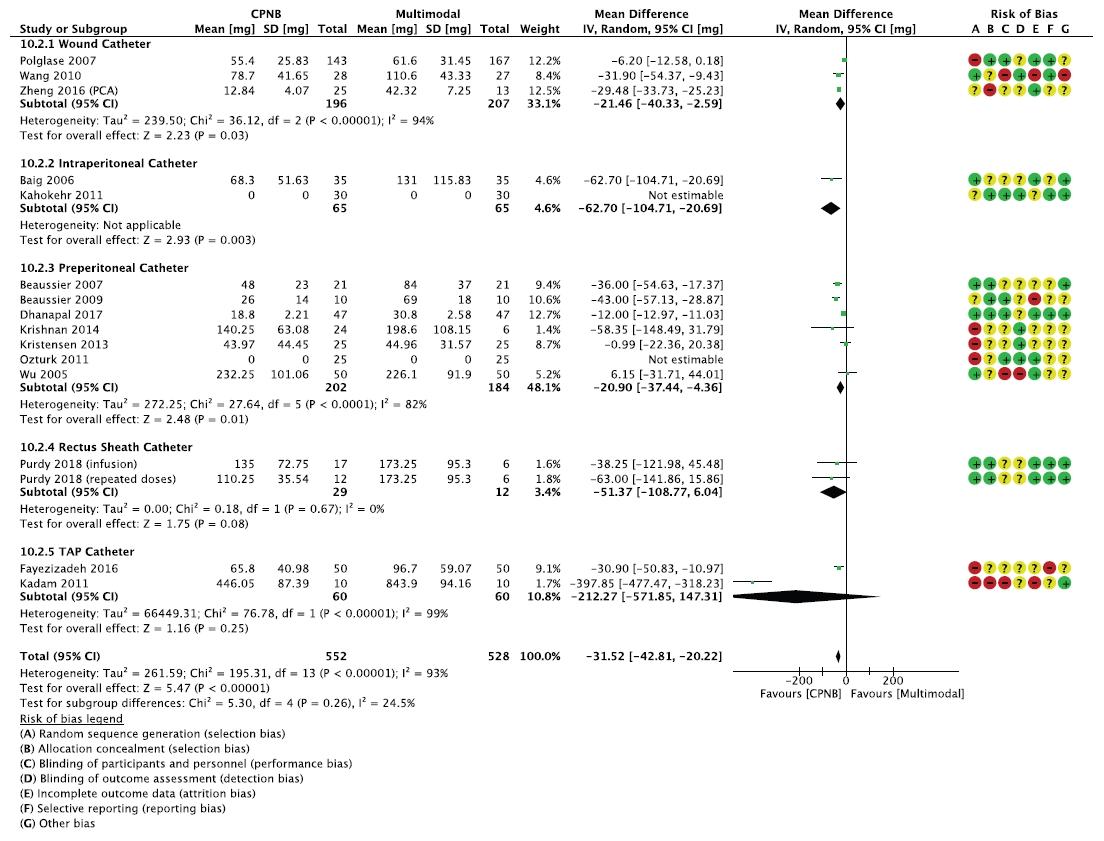
Wound catheter
Three studies evaluated the effectiveness of wound catheters on pain management following midline laparotomies [28,34,38]. All three studies compared the use of wound catheters to systemic opioids, while Zheng et al. also compared wound catheters to epidurals. See Table 1 for baseline characteristics, local anesthetic dosing, and comparison groups. The wound catheters were all placed by surgeons.
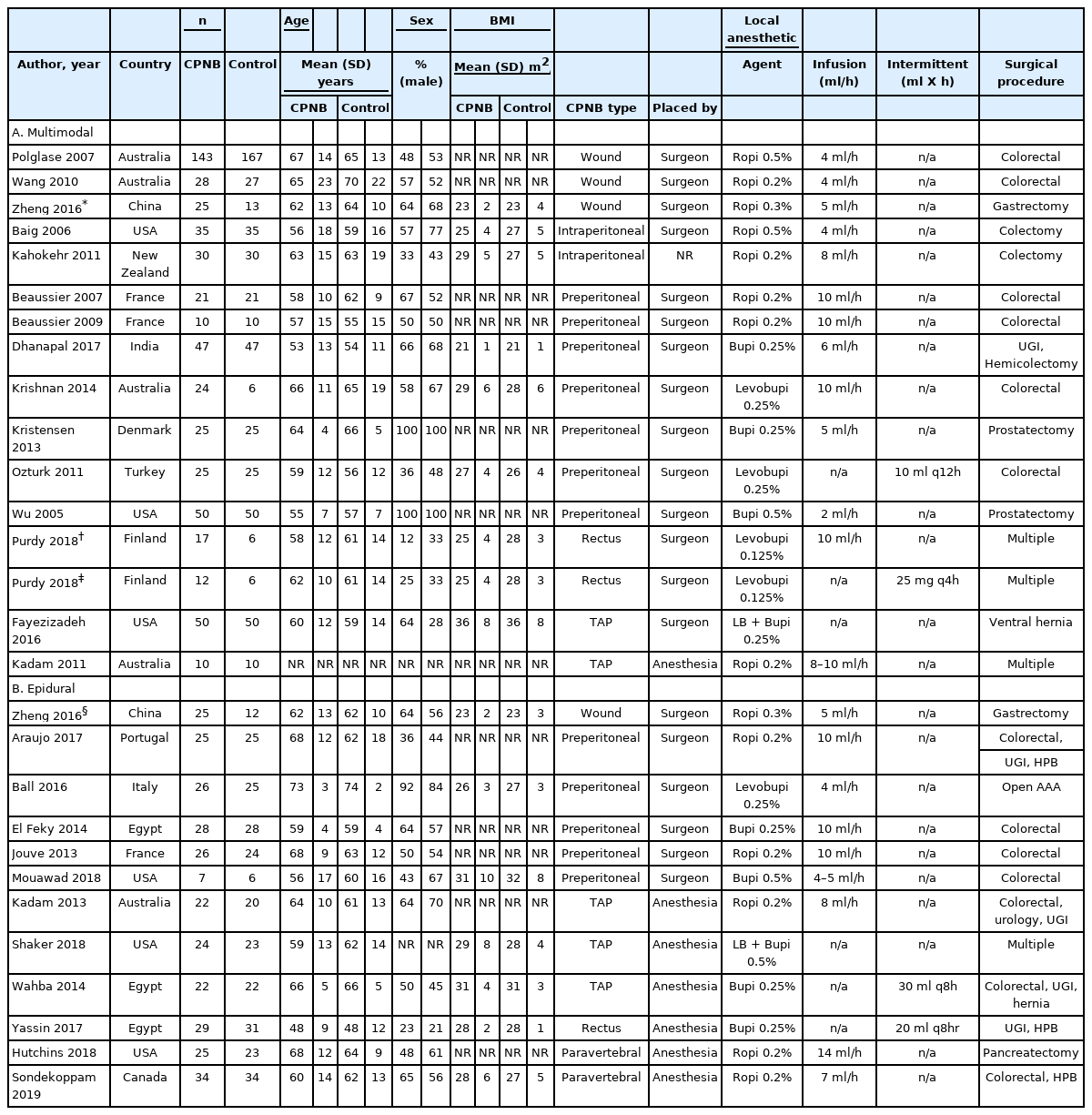
Characteristics of Included Studies Comparing Continuous Peripheral Nerve Blockade (CPNB) to Multimodal and Epidural Analgesia for Patients Undergoing Midline Laparotomy
Zheng et al. [34] found no difference in pain scores at rest or with movement between groups. Although Zheng et al. displayed these results as figures, exact numbers were not available for meta-analysis. Overall, patients with wound catheters used less opioids over 48 h (MD: -21.46 mg, 95% CI [-40.33, -2.59], P = 0.03, I2 = 94%, three studies, n = 403) (Fig. 2).
Cumulative opioid consumption (in oral morphine equivalents) at 48 h comparing between continuous peripheral nerve blocks (CPNB) and multimodal analgesia for patients undergoing midline laparotomy. CPNB: continuous peripheral nerve block, IV: inverse variance, PCA: patient-controlled analgesia, SD: standard deviation, green color: low risk of bias, yellow color: unclear/moderate risk of bias, red color: high risk of bias, bold text: indicates subgroups, subtotal and total effect sizes and weighting.
Wang et al. [28] reported higher rates of PONV among wound catheter participants compared to controls. Zheng et al. [34] recorded lower PONV and sedation scores in the wound catheter group compared to the patient-controlled analgesia (PCA) group, particularly in the first 12 postoperative hours. There was a shorter LOS among participants in the wound catheter group than participants in the PCA group. Rates of PONV and LOS were not significantly different between the wound catheter and epidural groups.
Intraperitoneal catheters
The evidence for intraperitoneal catheters comes from two double-blind placebo-controlled RCTs using the ON-Q® system [37,39]. In the first RCT, Baig et al. [39] studied 66 patients undergoing elective colectomy and found that intraperitoneal catheters decreased the 48-h opioid consumption. There was no significant difference in pain scores except for postoperative day two afternoon. The generalizability of the study is limited by the lack of multimodal analgesia.
The second RCT consists of 60 patients undergoing colectomy, with both groups also receiving thoracic epidurals [37]. This study also found that an intraperitoneal catheter infusion for three days further decreased the pain scores with movement and coughing at multiple time points within the first week postoperatively. However, the data need to be interpreted in the context of overall low pain scores (maximum 4/10) in both groups. We were not able to obtain opioid consumption data from the study authors for meta-analysis.
Preperitoneal catheters
There were 12 studies included involving preperitoneal catheters with seven compared against multimodal analgesia [25,30,31,35,40–42] and five compared against epidural catheters [21,24,43–45]. In all cases, the catheters were placed by the surgeon during wound closure. In one case, both the preperitoneal and the comparison groups received thoracic epidurals [25]. We considered this study to compare multimodal analgesia with preperitoneal catheters since both groups received epidurals, which we assumed would decrease the overall effect of preperitoneal catheters.
Of the studies comparing preperitoneal catheters to multimodal analgesia, only four of seven reported 48-h pain scores. There was no significant difference in pain at 48 h, either individually or pooled (MD: -0.01, 95% CI [-0.12, 0.10], P = 0.84, I2 = 0%, four studies, 294 patients). The pooled results of six studies showed less cumulative opioid consumption at 48 h in patients with preperitoneal catheters than those receiving multimodal analgesia (Fig. 2). When compared to epidurals, there was no significant difference in pain scores (MD: 0.38, 95% CI [-0.10, 0.86], P = 0.12, I2 = 12%, three studies, 114 patients). The pooled results of these two studies showed less opioid consumption among patients with epidurals (Fig. 3).

Cumulative opioid consumption (in oral morphine equivalents) at 48 h comparing between continuous peripheral nerve blocks (CPNB) and epidural analgesia for patients undergoing midline laparotomy. CPNB: continuous peripheral nerve block, IV: inverse variance, SD: standard deviation, green color: low risk of bias, yellow color: unclear/moderate risk of bias, red color: high risk of bias, bold text: indicates subgroups, subtotal and total effect sizes and weighting.
Compared to placebo, preperitoneal catheters reduced LOS in two of four studies reporting hospital stay duration; however, the overall effect was not statistically significant (MD: -1.77 days, 95% CI [-5.04, 1.49], P = 0.29, I2 = 98%, three studies, 192 patients) (Supplementary Fig. 2) [25,35,40,42]. Epidurals reduced LOS compared to preperitoneal catheters in two of three studies (MD: 1.11 days, 95% CI [0.71, 1.51], P < 0.001, I2 = 65%, three studies, 157 patients) (Supplementary Fig. 3) [43–45].
TAP catheters
Five studies involving TAP catheters were included, with two comparing to multimodal analgesia [23,32] and three comparing to epidural analgesia [26,36,46]. In one study, the TAP catheters were placed by the surgeon [32], whereas in the other four studies TAP catheters were placed by anesthesiologists under ultrasound guidance [23,26,36,46]. The opioid groups did not have catheters placed and all patients in those studies received PCA pumps.
Kadam and Field [23] found a significant reduction in pain scores during coughing in the first two days for patients with TAP catheters compared to multimodal analgesia. Wahba and Kamal [36] found that the epidural group had significantly lower pain scores at all time points compared to the TAP group. The other three studies found no differences in pain scores. There was no significant difference overall in pain scores compared to multimodal analgesia (MD: -1.32, 95% CI [-2.70, 0.06], P = 0.06, I2 = 52%, two studies, 120 patients) or epidural analgesia (MD: 0.89, 95% CI [-1.10, 2.88], P = 0.38, I2 = 95%, three studies, 133 patients). Both studies comparing with opioid analgesia found a significant reduction in opioid use over 48 h when patients received TAP catheters (Fig. 2) [23,32]. The evidence for comparing TAP catheters to epidurals was conflicting. One study comparing TAP to epidural catheters found no difference in opioid consumption [46], one found a significant reduction in opioid use with epidural analgesia [36], and the other found less opioid use in the TAP group [26] (Fig. 3). It must be noted that the study finding higher opioid use in the epidural group included a converted dose of the epidural opioids in the total opioid consumption [26]. Wahba and Kamal [36], and Rao Kadam et al. [46] did not use opioids in their epidural solution [36,46].
Rectus sheath catheters
Two studies involving rectus sheath block (RSB) catheters were included with one comparing to multimodal analgesia [33] and one comparing to epidural analgesia [29]. Purdy et al. [33] included three groups: RSB with intermittent dosing, RSB with continuous infusion, and a control (opioid analgesia). The catheters were placed by the surgeon in the Purdy et al. [33] study and under ultrasound guidance by an anesthesiologist in the Yassin 2017 study.
Purdy et al. [33] found no differences in the 48-h pain scores between the three groups. The means and standard deviations were not available for meta-analysis. The intermittent dosing group had lower pain at rest at 12 h; all other time points were not significantly different [33]. Similarly, Yassin et al. [27] found no differences in pain scores at any time point [29]. In terms of opioid consumption at 48 h, Purdy et al. [33] found a reduction among both RSB groups compared to multimodal analgesia (Fig. 2), whereas Yassin et al. [27] found opioid consumption to be significantly lower in the epidural group compared to the RSB group (Fig. 3).
Paravertebral catheters
Two randomized trials on paravertebral catheters met the inclusion criteria [22,27]. Hutchins et al. [22] studied 48 patients undergoing open pancreatic surgery randomized to T8 paravetebral catheters or T7-8 epidurals. This trial found that while opioid consumption was decreased within the first 24 h in the epidural group, there was no difference in opioid consumption at other time points (Fig. 3). Moreover, there was no significant difference in pain scores.
In a pragmatic randomized trial of 70 patients comparing bilateral paravertebral versus epidurals, all inserted between T7 and T9, Sondekoppam et al. [27] found that paravertebral catheters provided non-inferior analgesia for the primary outcome of 24-h pain score with movement. Within the follow-up period of 72 h, there was no significant difference in pain scores or opioid consumption. The LOS in hospital was also similar (MD: -1.40 days, 95% CI [-4.31, 1.51], P = 0.34, I2 = 23%, two studies, 116 patients) (Supplementary Fig. 3).
Overall comparison and sensitivity analyses
Primary outcomes
When comparing the combined effects of all CPNB studies, there was no statistically significant difference in pain scores between CPNB and either multimodal analgesia or epidural analgesia (MD: -0.35, 95% CI [-0.77, 0.07], P = 0.10, I2 = 95%, 10 studies, 909 patients; MD: 0.45, 95% CI [-0.13, 1.04], P = 0.13, I2 = 84%, eight studies, 375 patients, respectively) (Tables 2 and 3). Patients receiving CPNB used significantly less opioids than those receiving multimodal analgesia (MD: -31.52, 95% CI [-42.81, -20.22], P < 0.001, I2 = 93%, 13 studies, 970 patients). This was observed for the subgroups receiving continuous wound and preperitoneal catheters (Fig. 2). There was no statistically significant difference in opioid use between CPNB and epidural analgesia in the overall comparison (MD: 16.13, 95% CI [-0.10, 32.36], P = 0.05, I2 = 94%, eight studies, 342 patients); however, opioid consumption was reduced in patients receiving epidural analgesia in the preperitoneal, rectus sheath, and paravertebral subgroups (Fig. 3).
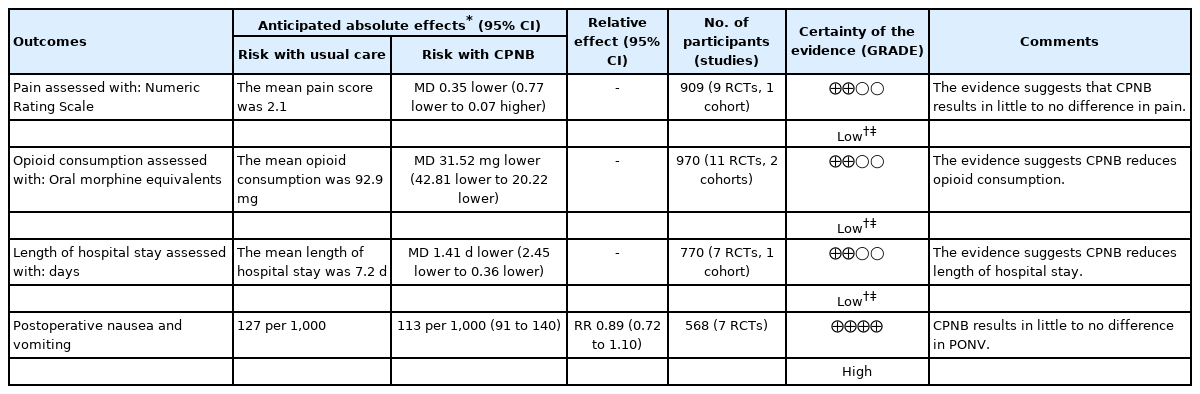
Summary of Findings for Continuous Peripheral Nerve Block (CPNB) Compared to Multimodal for Patients Undergoing Surgery via Midline Laparotomy
Secondary outcomes
Length of hospital stay was significantly shorter for the epidural group compared to the CPNB group (MD: 0.78 days, 95% CI [0.27, 1.29], P = 0.003, I2 = 59%, eight studies, 399 patients, Table 3 & Supplementary Fig. 3) and again less for the CPNB group compared to multimodal analgesia (MD: -1.41 days, 95% CI [-2.45, -0.36], P = 0.008, I2 = 98%, eight studies, 770 patients, Table 2 & Supplementary Fig. 2). PONV was not statistically significantly different between either multimodal or epidural analgesia overall (odds ratio [OR]: 0.89, 95% CI [0.72, 1.10], P = 0.30, I2 = 0%, seven studies, 568 patients; OR: 1.02, 95% CI [0.56, 1.86], P = 0.96, I2 = 36%, five studies, 265 patients), nor for any of the subgroups (Tables 2 and 3).
Sensitivity analyses
We examined the robustness of the main outcomes by conducting a series of sensitivity analyses (Supplementary Table 3). Nine studies had two or more domains that were deemed to have high risk of bias [21–23,26–28,32,42,46]. In the primary analyses, the difference in opioid consumption between CPNBs and epidurals only bordered on statistical significance. However, there was a significant difference in opioid consumption favoring epidurals once the high risk of bias studies were removed (MD: 16.66, 95% CI [2.48, 30.84], P = 0.02, I2 = 96%, five studies, 205 patients). Removing the high risk of bias studies resulted in the LOS difference becoming non-significant between CPNB and multimodal analgesia (MD: -1.57 days, 95% CI [-3.61, 0.48], P = 0.13, I2 = 88%, six studies, 570 patients). Other outcomes were minimally affected by removing the high risk of bias studies.
The only two studies that included patients with a lower midline incision were removed to examine the effect [30,42]. Removing these studies had minimal effect on the pain scores, PONV, opioid consumption, or LOS. The two cohort studies comparing CPNBs to multimodal analgesia were removed to examine the effect [31,32]. Removing cohort studies had minimal effect on pain scores, PONV, and opioid consumption. However, the difference in LOS became a statistical non-significant result (MD: -1.29 days, 95% CI [-3.16, 0.57], P = 0.17, I2 = 94%, seven studies, 670 patients).
Eight studies [21,22,26,27,34,43–45] used opioids in the epidural solution while four studies [24,29,36,46] used only local anesthetics. Removing the studies that did not use opioids in the epidural solution did not change the effect size of pain scores but made the results statistically significant (MD: 0.48, 95% CI [0.34, 0.61], P < 0.001, I2 = 0%, four studies, 216 patients). Only one study explicitly stated that epidural opioids were included in the calculation of cumulative opioid consumption [26]. Removing these studies reduced the effect size of opioid consumption between CPNB and epidural analgesia (MD: 4.48 mg, 95% CI [-14.95, 23.91 mg], P = 0.65, I2 = 93%, four studies, 183 patients). Removing these studies had minimal effect on the LOS and PONV rates.
Discussion
The use of CPNBs, often in the form of fascial plane blocks, is increasingly common [47]. The popularity of these techniques has grown in response to the potential complications and drawbacks of neuraxial analgesia such as hypotension from sympathetic blockade, leg weakness, epidural hematomas, and epidural abscesses [47]. However, many of these techniques are relatively new and their efficacy has not been established relative to epidural analgesia, opioid analgesia, or to one another.
We found that pain scores were not significantly different when comparing the combined effect of all CPNBs to either multimodal or epidural analgesia for abdominal surgery via a midline laparotomy. Our meta-analysis found that opioid consumption was significantly less for CPNBs compared to conventional analgesia with opioids, particularly for wound, preperitoneal, and rectus sheath catheters. There was no significant difference in opioid consumption when comparing CPNBs as a whole to epidural analgesia. However, opioid consumption was significantly less for patients receiving epidural analgesia when compared to preperitoneal, rectus sheath, and paravertebral catheters. In a number of cases, this review states that there are no significant differences between CPNBs and either multimodal or epidural analgesia. This does not necessarily imply equivalency between the two techniques, but rather insufficient data to suggest superiority of one technique over the other. This is particularly true when a small number of studies are used in the comparison. Although meta-analysis seeks to increase statistical power by combining studies, the power may decrease when a small number of studies are included. Because the random-effects model accounts for between-study variation, five or more studies are required to reliably achieve greater power than the primary studies [48].
Overall, the main findings of this review were robust, being only minimally influenced by the sensitivity analyses. Removing studies with procedures using lower midline incisions did not significantly change the results of the meta-analyses. When studies with two or more high risk of bias domains were removed from the opioid consumption, comparison moved from bordering on statistical significance to favoring epidurals; however, the change in effect size between groups was negligible. LOS was the most sensitive to removing high risk studies. When high risk of bias and cohort studies were removed the difference in LOS became not statistically significant with the point estimate moving in the opposite direction.
One area of concern is that we were not able to determine whether most studies included opioids administered via the epidural route in the calculation of total cumulative opioid consumption. This was only explicitly stated in one study. This may have a large impact on whether one technique is favored over another in terms of opioid reduction for a few reasons. Although there is some uncertainty about equianalgesic dose conversion from IV systemic to epidural opioids, the most commonly cited conversion is 10 : 1 for both morphine and hydromorphone [49]. Thus, even low dose opioids added to epidural solutions can contribute to a large proportion of the cumulative opioid consumption. Furthermore, the patients would receive this amount of opioid regardless of whether they needed it. This creates a conflict for pain research because including epidural opioids in the cumulative opioid consumption will favor other techniques, while not including them will favor epidurals. Our recommendation is future studies comparing CPNB to epidural analgesia use only local anesthetic without opioids in the epidural solution if using opioid consumption as an outcome. The next best option is to be very explicit in the method of equianalgesic opioid conversion from the epidural solution to the cumulative opioid consumption.
The majority of studies in this review had at least one domain that was deemed to have high potential for bias. Our ability to draw firm conclusions from this review was hampered by this high risk of bias. However, removing the studies with two or more domains of high risk of bias did not influence the pain score comparison. The finding that epidurals may reduce opioids more than CPNBs was strengthened when removing these studies and the finding that CPNBs may reduce LOS compared to multimodal analgesia was lessened. Overall, if bias was influencing the results of the studies, it seems to exaggerate the benefits of CPNBs in our included studies.
In addition to the risk of bias, our ability to draw conclusions was limited by heterogeneity. There was some clinical heterogeneity between studies due to various types of surgery and practice patterns regarding the type and dose of analgesics and adjuncts. However, pooled results for pain scores and opioid consumption were deemed acceptable by our team since the bulk of postoperative pain originates from the abdominal wall [50]. All included studies involved a midline incision and each intervention was aimed at reducing afferent nociceptive signaling from the thoracoabdominal nerves. There was also statistical heterogeneity found in many of our analyses. This was expected given the practice variation in terms of pain management and uses of adjunct therapies. The heterogeneity seen in terms of pain and opioid consumption also relates strongly to the type of surgery. Despite these differences, the pooled results were deemed acceptable given that in each case the two comparison groups were undergoing the same surgical procedure and were subject to the same pain management practice patterns. Ideally, we would have compared various CPNB techniques to one another using a network meta-analysis. We contemplated this but decided that, given the degree of clinical and statistical heterogeneity described above, the assumptions of transitivity and consistency would not be met.
This review did not find evidence of superior pain scores between CPNBs and either multimodal or epidural analgesia. CPNBs may decrease postoperative opioid consumption and hospital LOS compared to multimodal analgesia. Epidural analgesia may further decrease opioid consumption and LOS when compared to CPNBs. CPNBs should be considered a viable alternative to epidural analgesia when contraindications to epidural placement exist for patients undergoing midline laparotomies. Future studies should directly compare various CPNB techniques to one another. Future systemic reviews should seek to directly or indirectly compare various CPNB techniques once enough high-quality studies allow assumptions to be met.
Notes
Funding
CM received financial assistance from the Dr. Thomas Coonan Anesthesia, Pain & Perioperative Medicine Studentship and JJ Carroll Travel Fund Award through the Dalhousie Medical Research Foundation (Halifax, Canada).
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Jonathan G. Bailey (Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Supervision; Writing – original draft)
Catherine W Morgan (Data curation; Formal analysis; Funding acquisition; Project administration; Writing – review & editing)
Russell Christie (Data curation; Formal analysis; Investigation; Writing – review & editing)
Janny Xue Chen Ke (Data curation; Formal analysis; Investigation; Writing – review & editing)
M. Kwesi Kwofie (Conceptualization; Writing – review & editing)
Vishal Uppal (Conceptualization; Formal analysis; Methodology; Writing – review & editing)
Supplementary Materials
Search strategy for Embase, Cochrane, and MEDLINE databases
OpenGrey search strategy (adapted from the MEDLINE search)
Summarized results of sensitivity analyses
Funnel plot to assess publication bias for studies comparing pain scores and cumulative opioid consumption between continuous peripheral nerve blocks (CPNB) and multimodal analgesia. A: pain scores, B: opioid consumption, MD: mean difference, TAP: transversus abdominus plane, SE: standard error
Length of stay (LOS) in hospital comparing between continuous peripheral nerve blocks (CPNB) and multimodal analgesia for patients undergoing midline laparotomy. CPNB: continuous peripheral nerve block, IV: inverse variance, PCA: patient-controlled analgesia, SD: standard deviation, green color: low risk of bias, yellow color: unclear/moderate risk of bias, red color: high risk of bias, bold text: indicates subgroups, subtotal and total effect sizes and weighting.
Length of stay in hospital comparing between continuous peripheral nerve blocks (CPNB) and epidural analgesia for patients undergoing midline laparotomy. CPNB: continuous peripheral nerve block, IV: inverse variance, SD: standard deviation, green color: low risk of bias, yellow color: unclear/moderate risk of bias, red color: high risk of bias, bold text: indicates subgroups, subtotal and total effect sizes and weighting.