Surgical excision of the breast giant fibroadenoma under regional anesthesia by Pecs II and internal intercostal plane block: a case report and brief technical description: a case report
Article information
Abstract
A 22-years-old female patient at 171 cm and 67 kg visited the Department of Breast Surgery of the hospital with a mass accompanied with pain on the left side breast as chief complaints. Since physical examination revealed a suspected huge mass, breast surgeon decided to perform surgical excision and requested anesthesia to our department. Surgery of breast tumor is often under local anesthesia. However, in case of big size tumor, surgery is usually performed under general anesthesia. The patient feared general anesthesia. Unlike abdominal surgery, there is no need to control visceral pain for breast and anterior thoracic wall surgery. Therefore, we decided to perform resection under regional anesthesia. Herein, we report a successful anesthetic and pain management of the patient undergoing excision of a huge breast fibroadenoma under regional anesthesia using Pecs II and internal intercostal plane block.
Surgery to remove breast tumor is often under local anesthesia. However, in case of big size tumor, surgery is usually performed under general anesthesia. Surgery can also be performed under conventional regional anesthesia utilizing thoracic epidural block (TEB), thoracic paravertebral block (TPVB), and intercostal nerve block (ICNB). Recently, pectoral nerve block (Pecs block), a new anterior thoracic wall block method that uses ultrasound, has been introduced as a safer peripheral nerve block than prior conventional methods. Since its introduction, Pec block is being used for postoperative pain control such as breast cancer surgery [12]. Although there is nearly no study report on this Pecs block, if it is performed using ultrasound, it is comparatively easy with less risk of complication such as hematoma or pneumothorax. Therefore, it is becoming preferred and widely used method to manage perioperative pain management for breast surgery.
Herein, we report an anesthetic and pain management of patient undergoing an excision of a huge breast fibroadenoma under regional anesthesia using Pecs II block and internal intercostal plane block (IIPB).
Case Report
A 22-years-old female patient at height of 171 cm and weight of 67 kg visited the Department of Breast Surgery of the hospital with a mass accompanied with pain on the left side breast as chief complaints. Since physical examination findings suspected a huge mass, breast surgeon decided to perform surgical excision and requested anesthesia to our department. There were no other specific findings from preoperative assessment. The patient feared general anesthesia. Therefore, we decided to perform resection under regional anesthesia considering that there would be no particular problem if the somatosensory pain could be managed and the surgical site was restrained on the left side breast. On the day before surgery, these matters were explained to the patient and the guardian. We also obtained the informed consent.
No premedication was administered. When the patient arrived at the operation theater, monitoring devices including electrocardiograph, noninvasive blood pressure monitor, and pulse oximeter were attached to the patient.
Before the patient was sedated, ultrasound-guided Pecs II block and IIPB were performed with the patient in supine position. Skin was disinfected. Ultrasound probe and cable were protected with a sterile ultrasound probe cover. Transportable ultrasound equipment with a 50 mm linear 15–6 MHz probe (SonoSite M-Turbo™, SonoSite Inc., Bothell, WA, USA) was used. The probe was placed below the lateral third of the clavicle. Skin puncture site was infiltrated with 2% lidocaine. Block was then performed by using a 22-gauge Quincke needle (BD Spinal Needle, BD Medical, New Jersey, USA). The needle was advanced to the neurovascular plane between the pectoralis major and minor muscles at the vicinity of the pectoral branch of the thoracoacromial artery and 10 ml of 0.375% ropivacaine was injected (Fig. 1). In a similar way, 20 ml of 0.375% ropivacaine was injected at the level of the 4th rib in the mid-axillary line between pectoralis minor and serratus anterior muscles (SAM) (Fig. 2). And 10 ml of 0.375% ropivacaine was injected at the level of the 4th costal cartilage space over the internal intercostal muscle (Fig. 3).

Ultrasound image of Pecs 1 block showing local anesthetic spread between pectoralis major and minor muscle. PM: pectoralis major muscle. pm: pectoralis minor muscle. R3: 3rd rib.
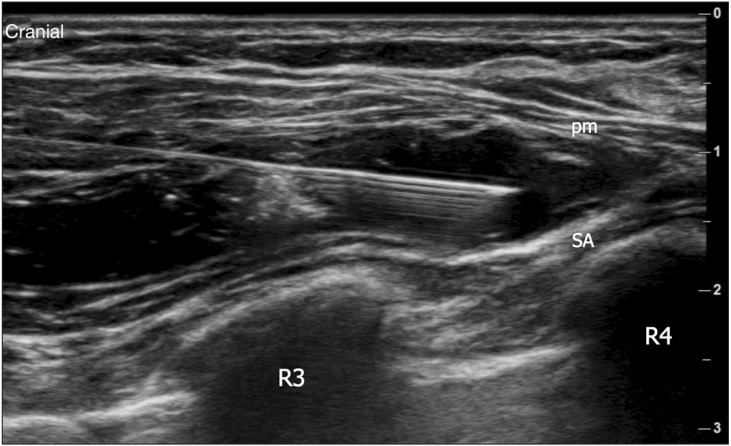
Ultrasound image of second injection of Pecs II block showing local anesthetic spread over serratus anterior muscle. pm: pectoralis minor muscle. SA: serratus anterior muscle. R3: 3rd rib. R4: 4th rib.

Ultrasound image of internal intercostal plane block showing local anesthetic (LA) spread over internal intercostal muscle. PM: pectoralis major muscle. EIm: external intercostal membrane. IIM (arrowhead): internal intercostal muscle. ☆: innermost intercostal/transversus thoracis muscle. C4: 4th costal cartilage. C5: 5th costal cartilage.
At 15 minutes after performing the block, we checked sensory loss through cold test. According to the patient's wish to sleep, propofol was infused by using a target controlled infusion (TCI, Orchestra®, Fresenius Vial, Brezins, France) by setting it to Schnider model. It was started from the effect-site concentration TCI of 1.5 µg/ml. It was then slowly increased toward the target point of Observer's Assessment Alertness/Sedation (OAA/S) scale 2–3 level. The surgery started at 25 minutes after performing the block. Operation time was 1.5 hours. Anesthesia time was 2 hours and 15 minutes. Intraoperative vital signs were stable. No opioid was needed. The patient did not complain postoperative pain of the surgical site. Her numerical rating scale of pain was 0/10.
Discussion
The well-known methods for anesthesia or analgesia objective in breast cancer surgery are TEB, TPVB, and INCB, etc. [345]. Compared to conventional regional anesthesia, Pecs block is a less invasive procedure with easier techniques and lesser risk of complications. Therefore, it has been increasing used. Blanco [1] decribed Pecs block for the first time in 2011. Pecs block is categorized into Pecs 1 block and Pecs II block. Pecs 1 block is a compartment block that injects local anesthetics between pectoralis major and minor muscles in order to block medial and lateral pectoral nerve that innervate the pectoralis major and minor [1]. The medial pectoral nerve arises from the medial cord (sometimes directly from the anterior division of the inferior trunk) of the brachial plexus which originates from the eighth cervical and first thoracic roots. It enters the deep surface of the pectoralis minor muscle where it divides into a number of branches to supply the muscle. Two or three branches pierce the muscle and end in the sternocostal head of the pectoralis major muscle. The medial pectoral nerve pierces both the pectoralis minor and the sternocostal head of the pectoralis major. The lateral pectoral nerve arises from the lateral cord of the brachial plexus which originates from the fifth, sixth, and seventh cervical nerves. It passes across the axillary artery and vein, pierces the clavipectoral (coracoclavicular) fascia, and is distributed to the deep surface of the pectoralis major muscle. Therefore, injection of local anesthetics between pectoralis major and minor muscles can block medial and lateral pectoral nerves.
Pecs II block is the 2nd injection for the purpose of intercostal nerve block subsequent to Pecs 1 block. It is a compartment block to inject local anesthetics above or under the SAM above the 3rd rib [2]. The intercostal nerve runs between the innermost intercostal/transversus thoracis muscle and the internal intercostal muscle (IIM). At the mid-axillary line, it branches off the lateral cutaneous branch (LCB). The LCB pierces the external intercostal muscle and the SAM, and divides into posterior and anterior branches. The anterior branch runs over the pectoralis major muscle into the mammary gland. The anterior cutaneous branch (ACB) divides into a medial branch coursing over the sternum and a lateral branch running into the breast tissue. From both sides, fine branches course to the nipple-areola complex (Fig. 4). Therefore, the LCB of intercostal nerve can be blocked by injecting local anesthetic superficial or deep beneath SAM overlying the 3rd rib.
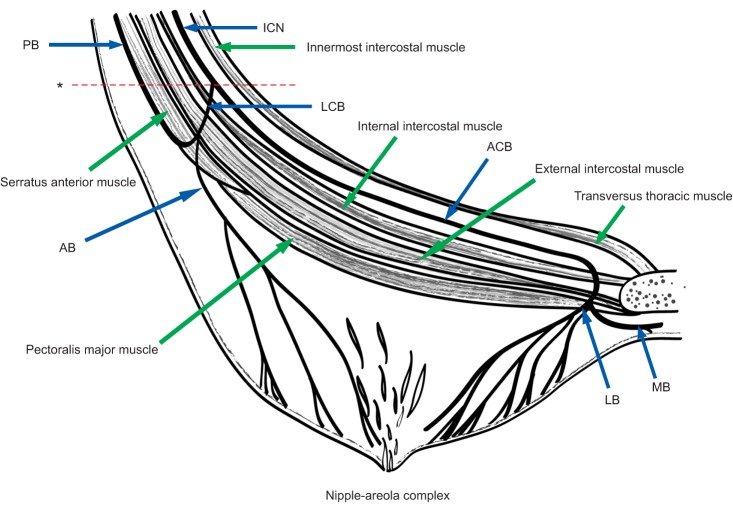
Schematic representation of the course of anterior cutaneous branch (ACB) and lateral cutaneous branch (LCB) of an upper intercostal nerve (ICN) in the horizontal plane. The intercostal nerve runs between the innermost intercostal/transversus thoracis muscle and the internal intercostal muscle. At the mid-axillary line, it branches off the LCB. The LCB pierces the external intercostal muscle and the serratus anterior muscle and divides into a posterior branch (PB) and an anterior branch (AB). The AB runs over the pectoralis major muscle into the mammary gland. The ACB divides into a medial branch (MB) coursing over the sternum and a lateral branch (LB) running into the breast tissue. From both sides, fine branches course to the nipple-areola complex. *Indicates mid-axillary line.
Usually, Pecs II block is also known to be good enough for making breast surgery possible. However, the actual cutaneous innervation of female breast area and nipple-areola complex should involve LCB as well as ACB of the intercostal nerve [6]. Therefore, blocking up to the ACB would not cause problem to breast surgery. In this case, the surgery range was expected to be the nipple-areola complex region and if required, it could invade into pectoralis muscle. Therefore, we conducted Pecs II block in order to block pectoral nerve and LCB. Local anesthetic was injected between IIM and external intercostal membrane (internal intercostal plane, IIP) in order to block the ACB.
ACB runs between innermost intercostal/transversus thoracis muscle and IIM. Therefore, we could inject local anesthetics above transversus thoracis muscle (transversus thoracic muscle plane, TTP) [7]. However, since there was pleura right under transversus thoracis muscle, there might be a risk of pneumothorax when punctured. In addition, the internal thoracic artery and vein run through above transversus thoracis muscle. Therefore, they might be injured. And ultrasonographic identification of the TTP may be difficult at the lateral edge of the sternum.
ACB also penetrates through IIM and pectoralis major muscle at this site and runs anteriorly. Therefore, injection to IIP (IIPB) could block ACB (Fig. 4). In addition, local anesthetic can spread to the above and below levels due to myofascial continuity like Pecs block. Therefore, it is possible to perform multiple segment blocks. In this case, sensory loss of ACB approximately from 2nd to 6th level by total injection of 10 ml was confirmed.
The advantage of this block method is that almost the whole anterior chest wall surgeries are possible under regional anesthesia by using this block method. As the patient wanted sedation, the surgery was carried out under sedation by using propofol. However, sensory loss of the surgery site was confirmed before sedation based on cold test. Even with effect-site concentration TCI of propofol at 1.9 ug/ml, the sedation was well-maintained without any change in intraoperative vital signs. In addition, the patient did not complain of postoperative pain of the surgery site. Judging from this, the analgesia was probably sufficient for this surgery.
Another advantage of this block method is that it is possible to modify and apply depending on the case. For the second injection of Pecs II block, it does not have to be injected at the third rib level. The injection level can be modified according to the surgical site. In this case, as the tumor was located around the nipple, the injection was performed not at the 3rd rib level, but at the 4th rib level.
Unlike abdominal surgery, there is no need to control visceral pain in case of breast and anterior thoracic wall surgeries. Therefore, anesthetic management using this block method would be a good alternative of general anesthesia. In addition, depending on the case, it is possible to perform surgery such as ambulatory surgery so that patient could be admitted and discharged on the same day. If breast surgery is conducted under general anesthesia using this block method concurrently, it will reduce the usage of anesthetics and opioids during and after surgery, resulting in early recovery of the patient.
