Analysis of medical disputes regarding chronic pain management in the 2009–2016 period using the Korean Society of Anesthesiologists database
Article information
Abstract
Background
The active involvement of anesthesiologists in chronic pain management has been associated with an increase in the number of related medical dispute cases.
Methods
Using the Korean Society of Anesthesiologists Legislation Committee database covering case files from July 2009 to June 2016, we explored injuries and liability characteristics in a subset of cases involving chronic pain management.
Results
During the study period, 58 cases were eligible for final analysis. There were 27 cases related to complex regional pain syndrome (CRPS), many of them involving problems with financial compensation (24/27, 88.9%). The CRPS cases showed male dominance (22 males, 5 females). In a disproportionately large number of these cases, the causative injury occurred during military training (n = 5). Two cases were associated with noninvasive pain managements, and 29 cases with invasive procedures. Of the latter group, procedures involving the spine (both neuraxial and non-neuraxial procedures) resulted in more severe complications than other procedures (P = 0.007). Seven of the patients who underwent invasive procedures died. The most common type of invasive procedures were lumbosacral procedures (16/29, 55.2%). More specifically, the most common damaging events were inadvertent intravascular or intrathecal injection of local anesthetics (n = 6).
Conclusions
Several characteristics of medical disputes related to chronic pain management were identified: the prevalence of injury benefit claims in CRPS patients, higher severity of complications in procedures performed at the spine or cervical region, and the preventability of inadvertent intravascular or intrathecal injection of local anesthetics.
Introduction
Chronic pain is one of the most frequent reasons that patients seek medical care [1]. The active involvement of anesthesiologists in chronic pain management has been paralleled by an increase in the number of related medical dispute cases [2]. Clearly, given that many different medical specialties are involved in chronic pain management in Korea and elsewhere, medical disputes are not limited to the anesthesiology community. However, because anesthesiologists have guided the practice of pain management (especially, interventional procedures), they are likely to be involved in the majority of chronic pain management disputes, now and in the future. Although complications do not always lead to lawsuits, they are usually the trigger for them. Thus, avoiding complications is of utmost importance.
In this study, we explored injuries and liability characteristics in the subset of cases associated with chronic pain management. The data were obtained from the Korean Society of Anesthesiologists (KSA) Legislation Committee database and covered case files from July 2009 to June 2016.
Materials and Methods
This study is the fourth analysis to use the KSA Legislation Committee database. Since its creation in July 2009, the KSA Legislation Committee database has been used to evaluate adverse anesthetic outcomes (including those related to pain clinics) based on information obtained from the case files of expert consultation referrals to the KSA. The data collection process was described previously in detail [34].
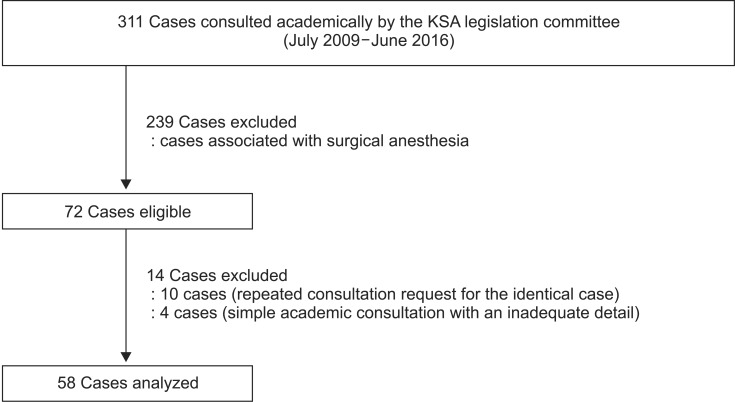
From the entry of the first case file into the database in July 2009 to June 2016, 311 cases have been collected, including 72 cases (23.2%) related to chronic pain management. Because the practice of pain control in our country includes many specialties, cases eligible for analysis were not limited to those in which anesthesiology was the responsible specialty. After the exclusion of 14 cases because of repeated consultation requests for the identical case (n =10) and simple academic consultations, the details of which were insufficient (n = 4), 58 cases were included in the analysis (Fig. 1).
Description of the variables
The characteristics of the patients and practitioners, the cause of referral (dissatisfaction with treatment outcome, determination of the appropriateness of the diagnosis or treatment, or the development of complications), treatment details, the mechanism and timing of the subsequent injury, and the outcomes were recorded. In addition, for those cases associated with complex regional pain syndrome (CRPS), a causative injury profile was included as well.
Chronic pain management claims were divided into two main categories based on the mode of treatment: invasive procedures and noninvasive pain management. Invasive procedures included nerve blocks, injections, ablative procedures, and implantation, maintenance, or removal of a device. If multiple treatments occurred, the case was categorized according to the treatment implicated in the complaint and the source of the alleged injury.
Invasive procedures were sub-classified according to the involved anatomic site; the spine, head and neck, upper extremities including the shoulder, trunk (chest, abdomen, and groin), and lower extremities. The spinal procedures were additionally sub-categorized into neuraxial procedures (epidural procedures including epiduroscopy, root blocks, and intrathecal procedures) and non-neuraxial procedures (paravertebral procedures such as facet joint blocks and vertebroplasty).
Noninvasive pain management was defined as diagnostic or therapeutic activities that did not require the use of needles or the insertion of a catheter or device. These included systemic medication management, physical therapy, and consultations.
Damaging events were defined as the mechanism by which an injury or complication occurred or allegedly occurred. These events were independently judged by each case file reviewer and grouped into the two categories depending on whether they were directly related to the procedure. Procedure-related events included needle trauma to the nerve or spinal cord, inadvertent intravascular injections, dural punctures, high block/total spinal block, pneumothorax, compressive hematoma events, and infections or abscesses. Events not directly related to the procedure included failure to diagnose, improper positioning, patient falls, deterioration of the patient's condition unrelated to the procedure, and failure to meet the patient's expectations.
The severity of the injury in each case was scored using the 10-point scale of the National Association of Insurance Commissioners (NAIC), which ranges from 0 (no obvious injury) to 9 (death) [5]. The severity scores were grouped into three broad categories for analysis; temporary and non-disabling (score 0–5), permanently disabling injuries (score 6–8), and death (score 9). The severity of the injury reflected the latest assessment at the time the case was referred.
The NAIC severity scale includes the following categories (examples are in parentheses):
0: No obvious injury
1: Emotional only (fright, no physical damage)
2: Temporary insignificant (lacerations, contusions, minor scars, rash; no delay in recovery)
3: Temporary minor (infections, fracture, fall in hospital; delayed recovery)
4: Temporary major (burns, surgical material left, drug side effect, brain damage; delayed recovery)
5: Permanent minor (loss of fingers, loss or damage to organs; includes non-disabling injuries)
6: Permanent significant (deafness, loss of a limb, loss of an eye, loss of one organ)
7: Permanent major (paraplegia, blindness, loss of two limbs, brain damage)
8: Permanent grave (quadriplegia, severe brain damage, lifelong care or fatal prognosis)
9: Death
Statistical analysis
Categorical variables are presented as number (%) and were compared using Pearson's χ2 test with a continuity correction or Fisher's exact tests, as applicable. The SPSS 18.0 package (SPSS, Inc., Chicago, IL, USA) was used for the statistical analysis. A P value < 0.05 was considered to indicate statistical significance.
Results
Of the 58 cases included in the final analysis, 22 (37.9%) were referred by police departments, 35 (60.3%) by civil or criminal courts, and one by the Anti-Corruption and Civil Rights Commission.
Characteristics of the CRPS cases
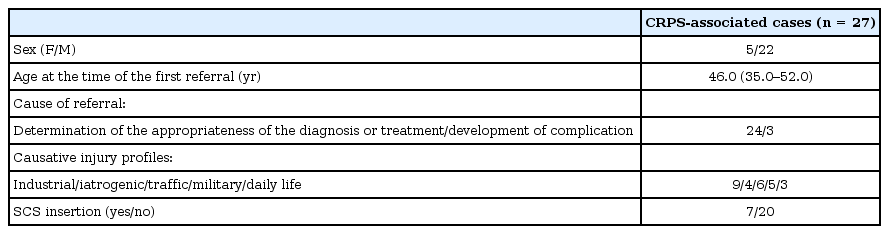
The majority of the 27 CRPS-related cases (46.6% of the overall cases) arose from problems with financial compensation, such as a request for the determination of the appropriateness of a diagnosis or treatment (24/27, 88.9%). In cases associated with CRPS, the median (interquartile) age of the patients at the time of injury was 39.0 (32.0–50.0) years, and most of the patients were male (22 vs. 5 females). Patients in CRPS-associated cases tended to be younger (P < 0.001) and were more likely to be male (P = 0.002) (Tables 1 and 2).
With respect to the distribution of cases in terms of the cause of the injury, industrial injuries were the most common type (9 cases), followed by traffic injuries (6 cases) and injuries from military training (5 cases). Seven cases (25.9%) involved the implantation of a spinal cord stimulator.
Invasive procedures vs. noninvasive pain management
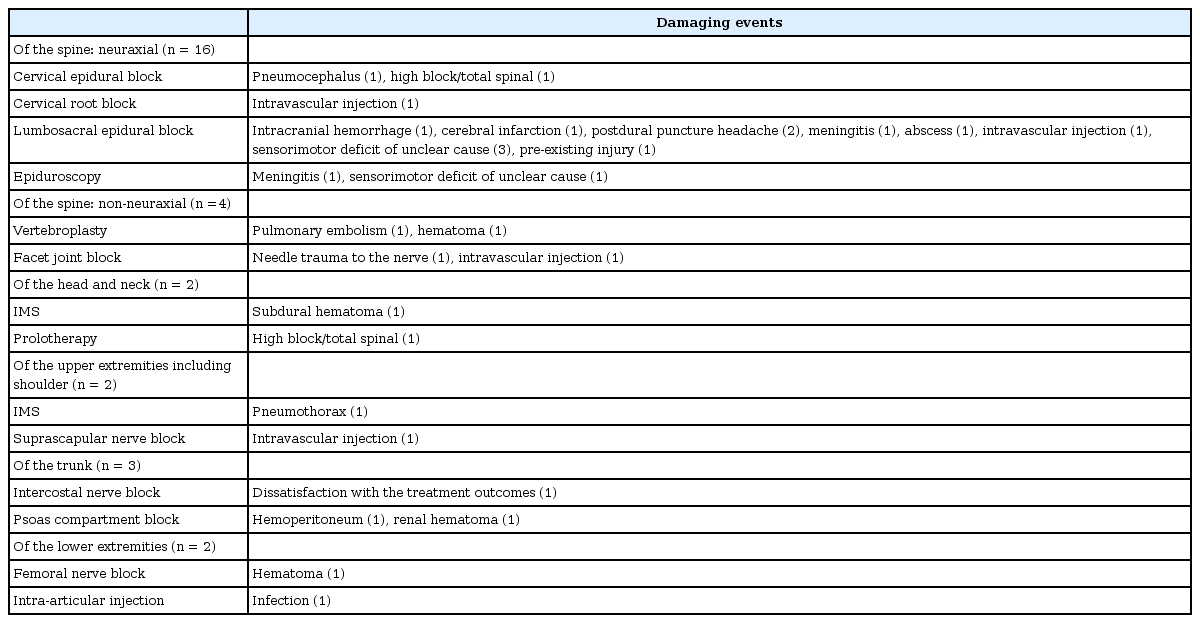
Two cases were associated with noninvasive pain management; one was a death caused by repeated propofol injections for lower back pain, and the other was a delayed diagnosis of spinal metastasis in which the patient was treated only with medication and physical therapy. Analysis of invasive procedure-related cases according to the involved anatomical site revealed that ‘spinal procedures’ were the most prevalent type (20/29, 69.0%) (Table 1).
The 29 cases related to invasive procedures included two cases not directly related to the procedure; one case of patient dissatisfaction with pain relief from the procedure, and one case in which the patient suffered a new trauma not related to the interventional procedure. The distribution of invasive procedure-related cases among provider types showed that the majority of providers were anesthesiologists (19/29, 65.5%), followed by general physicians (5/29, 17.2%).
Of the cases involving invasive procedures, seven resulted in death (Table 3).
Neuraxial vs. non-neuraxial procedures in the spinal procedures
In the cases related to invasive procedures of the spine, the severity of complications that developed due to neuraxial and non-neuraxial procedures was similar, according to their NAIC scores. The proportions of temporary/nondisabling injuries, permanent/disabling injuries, and death were also similar (4, 10, and 2 cases in the neuraxial procedures vs. 0, 1, and 3 cases in the non-neuraxial axial procedures, respectively). However, the complications from the spinal procedure (both neuraxial and non-neuraxial) were more severe than those from the other procedure types (P = 0.007) (Table 3).
Damaging events in the invasive procedure-related cases
Lumbosacral spinal procedures accounted for 55.2% of the 29 invasive procedure-related cases (10 cases of interlaminar or transforaminal epidural block, 1 of caudal epidural block, two of epiduroscopy, two of facet joint block, and one case of vertebroplasty). The only case related to thoracic spinal procedures was a claim that resulted from a case in which a pulmonary embolism during vertebroplasty led to death (Table 4). Five cases were related to cervical procedures (2 cases of cervical epidural block, and 1 case each of cervical root block, intramuscular stimulation, and prolotherapy).
Most of the damaging events occurring during invasive procedures were directly related to the procedure itself (92.6%, 27/29); these included intracranial hemorrhage (n = 1), cerebral infarction (n = 1), pneumocephalus (n = 1), pulmonary embolism (n = 1), pneumothorax (n = 1), direct needle trauma to a nerve (n = 1), high block/total spinal block (n = 2), meningitis (n = 2), abscess or infection (n = 2), postdural puncture headache (n = 2), hematoma or bleeding (n = 5), and inadvertent intravascular injection of local anesthetics (n = 4). Four cases of sensory or/and motor deficits were classified as of unknown cause due to an unclear mechanism/insufficient data or an inability to distinguish a pre-existing injury from a newly acquired one.
Discussion
In recent years, the interest and involvement of anesthesiologists in the new subspecialty of pain medicine have grown rapidly. As interventional pain management techniques have evolved, they have become safer, but they are still not without risks. Thus, subsequent to the serial KSA analytic reports on surgical anesthesia, we performed a focused analysis of medical disputes related to chronic pain management.
Prevalence of CRPS-associated cases
During the collection of case files over a 7-year period, from July 2009 to June 2016, there were 27 cases related to CRPS (46.6% of the overall cases), most of which were compensation claims (24/27, 88.9%). A similarly high prevalence of CRPS-related claims was determined in a foreign study, which reported that CRPS patients accounted for 17% of lawsuits and 54% of workers compensation claims [6]. These conflicts may be mainly attributed to the enigmatic nature of CRPS, its highly variable intensity and duration with diverse clinical outcomes, and its lack of definite diagnostic and treatment measures [7]. Because some patients complain of severe, persistent symptoms and signs that cannot easily be explained by an initial minor trauma, a causal relationship is often difficult to prove in litigation involving CRPS.
In South Korea, until August 2014, the two administrative bodies responsible for compensation, the Workmen's Compensation Insurance Act (WCIA) and the Patriots and Veterans Welfare Corporation Act, used the criteria of the American Medical Association in the diagnosis of CRPS, whereas most pain physicians diagnosed CRPS based on the revised International Association for the Study of Pain (IASP) criteria. This difference in diagnostic criteria was an additional cause of litigation involving CRPS. With the adoption by WCIA of new diagnostic criteria for CRPS based on the revised IASP criteria, the rate of CRPS-related claims is expected to decrease.
With the exception of one case, KSA case file reviewers determined that all referred cases were appropriate for the diagnosis of CRPS. The KSA Legislation Committee diagnoses CRPS using the modified IASP criteria. Although psychological factors such as anxiety, depression, and personality are not predictors for the development of CRPS, they influence the treatment response and the persistence of symptoms, as in other chronic pain conditions [8]. Thus, in the diagnosis of CRPS, it is critical to rigorously eliminate other possible causes, especially in injury benefit claims.
Our data showed male dominance (22 males, 5 females) in CRPS cases; this does not concur with the findings of studies from other countries, which have reported female-to-male ratios of 2.3–4.1 : 1 [910]. Although the KSA case files do not provide the actual incidence of CRPS in our country, a previous Korean epidemiologic study of CRPS also reported male dominance (female-to-male ratio of 0.8 : 1) [11]. The reasons for these different results between countries remain to be determined in larger epidemiologic studies.
Another finding of our study was the disproportionately high rate of military training (n = 5) as a causative injury; again, this was in contrast to the findings of the reports from other countries [910]. A previous Korea epidemiologic study found a prevalence of military personnel among CRPS patients 30–40 years of age (16/22, 72.7%) [11]. This may be explained by the increased risk of trauma during obligatory military service, together with a lack of early recognition and active treatment in military hospitals.
Spinal procedures: more severe complications
Similar to the results of the American Society of Anesthesiologists first closed claims analysis for chronic pain management [12], the most common invasive procedure-related medical dispute in our study involved neuraxial procedures, especially those at the lumbosacral level. Similar results were obtained in a previous domestic analysis of pain management-related medical disputes, in which case files were collected through the Korean Medical Association's Mutual Aid and a private medical malpractice liability insurance company [2].
Lumbar epidural procedures are performed by utilizing three approaches: caudal, interlaminar, and transforaminal. On reviewing medical records for consultation, the caudal approach could be easily differentiated from the other two approaches, but interlaminar and transforaminal approaches could not be differentiated in most cases. Therefore, we were unable to perform an additional analysis based on the approach technique.
Though there has been no randomized controlled trial comparing caudal, interlaminar, and transforaminal approaches in terms of the overall risk of complications, nerve injury may be theoretically more prevalent with the transforaminal epidural approach [13]. On the other hand, one study found that in terms of inadvertent intravascular injection, the caudal and transforaminal approaches had a similar risk profile, whereas the interlaminar approach was the safest of the three [14]. In that study, the authors suggested that the vascular anatomy was the reason for such results, namely the proximity of the radicular vein during the transforaminal approach, the high venous volume in the sacral hiatus, and thin posterior portions of the internal vertebral venous plexus at the interlaminar level.
Neuraxial procedures were also associated with grave outcomes (permanently disabling injuries and death), with 75.0% of the cases showing such outcomes. These findings may simply reflect the prevalence in South Korea of lumbar or sacral epidural procedures in the treatment of lower back pain. However, the proximity of the spinal cord during these interventions and the severity of the sequelae following injury to the spinal cord raise specific concerns about the safety of neuraxial procedures. In addition, our analysis suggested similarly grave outcomes in non-neuraxial procedures. Although vertebroplasty and facet joint blocks are generally considered to be inherently safer than neuraxial procedures, they carry the risk of intravascular injection, compressive hematoma, or even direct needle trauma to the nerve or spinal cord.
Systemic toxicity of local anesthetics
The most common specific damaging events were inadvertent intravascular (n = 4) or intrathecal (n = 2) injection of local anesthetics. These adverse events may be preventable by following a basic precaution during the interventions: aspirating the needle or catheter before each injection [15]. However, this precaution is not fail-safe and may not identify intravascular placement in at least 2% of patients [16]. Thus, in addition to a preliminary injection of a test dose and the use of radiographic guidance, it is important to use the smallest drug volume and lowest drug concentration that will produce the desired result [1517].
In-depth analysis of cases of mortality associated with invasive procedures
There were seven fatalities associated with invasive procedures. The most remarkable finding was that four cases involved cervical interventions (one case each of prolotherapy at the neck, cervical epidural block, cervical vertebroplasty, and cervical facet joint block). In other words, of the five cases involving cervical procedures, four resulted in death. Such findings may be attributed to the proximity of the vertebral artery and spinal cord during procedures of the cervical spine [18]. In particular, when considering a mortality case of prolotherapy presumably due to injection of local anesthetics into the spinal canal, practitioners should remain highly vigilant when performing even superficial cervical procedures.
Selection of pain medicine due to a fear of surgical anesthesia-related litigation
Our analysis indicated that in the cases associated with invasive procedures, anesthesiologists were the most common practitioners. This is not surprising given that anesthesiologists have been in the forefront in the practice of chronic pain management, especially with respect to interventional procedures.
In fact, some anesthesiologists limit their clinical practice to chronic pain management because of a fear of litigation involving surgical anesthesia. However, our analysis suggested that invasive procedures for chronic pain management carry a high risk of grave outcomes, as evidenced by the seven deaths identified in this study. In parallel with a recent trend toward interventional techniques, the proportion of anesthesia malpractice claims associated with pain medicine has increased. Thus, our findings suggest that anesthesiologists, as pain specialists, should proactively continue to search for safer and more effective treatment modalities.
Limitations of our database analysis
Similar to closed-claim analyses, the limitations of our analysis included the fact that only partial numerator data and no information on denominator data were available for a number of the procedures performed; thus, the tabulation of complications may have been biased toward more severe complications. In addition, our analysis was conducted on data that were transcribed to online data sheets by case file reviewers, who rely on the information contained in the referral file. Therefore, specific detailed information regarding mechanisms of injury may have been incomplete. Nonetheless, our analysis provides useful information on rare adverse events that are difficult to study prospectively without expensive large multicenter efforts [19].
In conclusion, our analysis identified several of the characteristics of medical dispute cases related to chronic pain management: the prevalence of injury benefit claims in CRPS patients, the higher severity of complications of the procedures involving the spine or cervical region, the preventability of inadvertent intravascular or intrathecal injection of local anesthetics, an increased risk of medical disputes, and a recent trend toward interventional techniques.
As more anesthesiologists have become interested and involved in the subspecialty of pain medicine, malpractice claims related to chronic pain management as a proportion of anesthesia malpractice claims have increased. These medico-legal conditions highlight the need for anesthesiologists, as pain specialists, to continue the search for safer and more effective treatments in their clinical practices.