Local anesthesia with monitored anesthesia care for patients undergoing thyroidectomy: a case series
Article information
Abstract
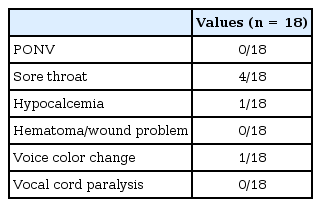
Because the current trend favors minimally invasive surgery for thyroid disease, increasing interest has developed for thyroidectomy under local anesthesia with monitored anesthesia care (MAC). Here, we retrospectively reviewed 18 cases of thyroidectomy performed under local anesthesia with MAC in a single center. All of the procedures were performed by a single surgeon, using local lidocaine infiltration around the incisional site and propofol plus remifentanil target-controlled infusion. Sore throat (4/18), hypocalcemia (1/18), and transient voice color change (1/18) were observed, but the patients recovered during the follow-up period. No cases of postoperative nausea and vomiting, hematoma, wound problems, or vocal cord paralysis were observed. Local anesthesia with MAC provided satisfactory sedation in most patients without conversion to general anesthesia.
Early in the 20th century, thyroid surgery was performed under local anesthesia. However, improvements in anesthetic drugs and equipment have allowed surgeons to perform thyroidectomy exclusively under general anesthesia. Although the majority of thyroid surgery is currently performed under general anesthesia, steady interest in the use of local/regional anesthesia for thyroid surgery has been developing. According to a recent survey conducted on patients with thyroid cancer [1], the second most frequent preoperative concern is the "side effects of general anesthesia (18.2%)," followed by "voice color change (40.3%)." "Feelings of lethargy and drowsiness after emergence from general anesthesia (28.3%)" was the second most stressful postoperative event followed by "postoperative pain (40.3%)." This survey shows that patients suffer much more from general anesthesia than previously believed. Several additional recent studies have reported that thyroid surgery can be safely performed under local, regional anesthesia, and general anesthesia [23]. However, no official reports of thyroidectomy under local/regional anesthesia with monitored anesthesia care (MAC) have been published in Korea. Here, we retrospectively reviewed 18 cases of thyroidectomy performed under local anesthesia with MAC with a review of the relevant literature.
Case Report
The use of patient data in the present report was approved by the Institutional Review Board of Seoul National University Hospital (Registration Number: 1603-149-751). The need for informed consent was waived. A total of 20 patients (age, 20–80 years), who were scheduled for thyroidectomy under local anesthesia with MAC between December 2015 and February 2016, were retrospectively reviewed. Electronic medical records including anesthetic, operative, nursing, and outpatient clinic records were reviewed. Exclusion criteria were communication barriers such as dementia, a language barrier, mental retardation, sternotomy, lateral neck dissection or multiple procedures, locally invasive cancer, morbid obesity, history of sleep apnea, claustrophobia, or an anxiety disorder. All of the thyroidectomies were performed by a single senior otolaryngologist.
Patients entered the operation theater without any premedication. After standard (electrocardiography, noninvasive arterial blood pressure, and pulse oximetry) and bispectral index (BIS; VISTATM monitoring system; Aspect Medical Systems Inc., Norwood, MA, USA) monitoring were applied, 3 L/min was delivered to patients through a nasal prong, and end-tidal CO2 was monitored with this equipment. All of the patients were administered 0.01–0.02 mg/kg midazolam during surgical dressing and draping. Propofol and remifentanil were delivered using a target controlled infusion (TCI) pump (Orchestra® module DPS, Fresenius Kabi, Langenhagen, Germany) with initial concentrations of 0.3 µg/ml and 0.5 ng/ml, respectively. The level of sedation was closely observed and targeted by BIS between 70–90 and a Ramsey Sedation Scale (RSS) score of 2–3. We increased or decreased the drug concentration by 0.2 µg/ml or 0.2 ng/ml on the TCI pump, according to the patient's response, to obtain the target sedation level.
The patients underwent the surgery in a supine position without extending the neck or using a back roll. After preparing the skin and surgical draping, the operator directly injected 10–12 cc of 2% lidocaine plus 1 : 100,000 epinephrine anesthesia around the incision line and the anterior field using a 22 gauge spinal needle. After the planned surgery was finished, the sedative drugs were stopped, respiration and the RSS were checked by an attending anesthesiologist, and the patient was delivered to the post-anesthesia care unit (PACU). Patients were discharged from the PACU if they achieved a modified Aldrete score ≥ 9 [4].
The total amount of administered sedatives such as propofol, remifentanil, or midazolam; desaturation (SpO2 < 95%); unexpected movements, such as coughing, swallowing, respiratory or limb motions, which interrupted the surgical procedure; and any other patient complaints were checked. After the surgery, the surgeon and patient were asked if they were satisfied with the anesthesia on a 3-point scale (bad-so so-good). Postoperative data were collected during hospitalization and at the outpatient clinic 1–2 weeks after discharge. The incidence of postoperative nausea and vomiting (PONV) and the use of analgesics or antiemetics were also determined. Postoperative analgesics/antiemetics were administered when the patients complained of postoperative pain/nausea (numerical rating scale > 5) or when they required these drugs. Treatments of 1 g propacetamol, 400 mg ibuprofen, or 0.075 mg palonosetron were intravenously administered for pain/nausea control. Postoperative complications were defined as more than one of the following conditions: PONV, sore throat, transient/permanent vocal cord paralysis, voice color change, hematoma, hypocalcemia, or wound problems.
Table 1 shows the patient characteristics; 2 of the 20 patients were excluded due to incomplete intraoperative electronic medical records. All of the scheduled surgical procedures were completed without intraoperative conversion to general anesthesia. The mean duration of surgery was 70.0 ± 24.2 min, and the mean duration of anesthesia was 87.5 ± 25.4 min (Table 2). Median intraoperative BIS was 80.5 (interquartile range [Q1-Q3], 80–94), and the median RSS score was 2 (Q1-Q3, 1–3). Four desaturation events occurred intraoperatively, but the patients soon recovered with respiration encouragement or elevation of the mandible in the surgical field without mask bagging or additional airway management. Neither the patient nor surgeon was disqualified from the anesthetic technique. Postoperative complications were evaluated during hospitalization and at the outpatient clinic follow-up (Table 3). No cases of PONV or receiving antiemetics were encountered postoperatively. No patient received analgesics while in the PACU, but five patients required pain control on the ward. According to the nurse's records, four patients complained of sore throat during hospitalization. Symptomatic hypocalcemia occurred in one patient, which was medically corrected during hospitalization without subsequent complications. Transient voice color change was observed in one patient who had recovered by the follow-up examination.
Discussion
This report describes cases of thyroidectomy under local anesthesia with MAC. The major advantages of general anesthesia are total loss of awareness, stable operative field, and a controlled airway. However, general anesthesia prolongs postoperative recovery and can lead to hemodynamic instability during anesthetic induction. In contrast, local anesthesia with MAC results in a faster postoperative recovery, no throat or vocal cord irritation, and avoidance of muscle relaxant use. However, it can be challenging to control the sedation level to meet the surgeons' and patients' requirements and while simultaneously maintaining proper oxygenation.
The ideal properties of sedative agents include rapid onset, easy titration, high clearance, and minimal side effects, particularly a lack of hemodynamic impairment or respiratory depression. However, no definitive data are available for sedative drugs used during thyroidectomy under local or regional anesthesia. Snyder et al. [3], reported about patients who received local anesthesia with MAC and boluses of midazolam, propofol, or fentanyl citrate for supplemental analgesia. Another study administered incremental doses of midazolam and fentanyl citrate to patients under MAC with regional anesthesia only when required [2]. The total and maintenance doses of the drugs were not reported in either study. This single or repeated bolus technique can induce an unstable plasma/effect-site concentration, consequently leading to variability in sedation level and hemodynamic instability [5].
To overcome this problem, we selected TCI, which results in a stable concentration of sedative agent at the effect site, and for which the sedation level can be easily changed. In early cases, we set the initial target propofol and remifentanil concentrations to 1.0 µg/ml and 1.0 ng/ml, respectively, during surgical draping, but recurrent desaturation events were observed at this concentration. A transient decrease in mean blood pressure (MBP) > 20% compared to baseline MBP simultaneously occurred in one case. Therefore, we decreased the initial target concentration after several cases and found that an effect-site propofol concentration of 0.3–1.5 µg/ml and that of remifentanil of 0.5–1.0 ng/ml produced a satisfactory level of sedation without disturbing hemodynamic stability in the other cases. Caution is needed when increasing the concentration of sedative according to surgical stimulation, as a small titration is essential to cope with the inter-individual pharmacodynamic effects of each drug. Although it is difficult to directly compare with sedation protocols used for other procedures, Höhener et al. [5] used a similar sedation protocol as our protocol under regional anesthesia (propofol effect-site concentration of 0.4–0.8 µg/ml and 0.5–1.0 ng/ml for remifentanil). In addition, we added a 0.01–0.02 mg/kg midazolam bolus before draping or surgical incision to provide anxiolysis and mild amnesia. Accordingly, previous reports noted that low-dose midazolam with propofol improves patient comfort and quality of the sedation without delaying recovery and made the operation easier than using propofol alone during sedation [67].
Recent reports have demonstrated that both of general and local anesthesia with MAC can be used for thyroidectomy due to similar clinical outcomes, perioperative complications, and patient satisfaction [238]. Although no significant differences were observed in the number of nausea episodes between the general and local anesthesia groups, the general anesthesia group required more antiemetics than the local anesthesia group [3]. Moreover, patients receiving local anesthesia with MAC spent less time in the PACU and daycare center, leading to early discharge [23]. We did not compare our cases with thyroidectomy under general anesthesia, so we cannot be certain that local anesthesia with MAC is superior to general anesthesia during thyroidectomy. However, the incidence of postoperative complications was similar to that of general anesthesia or local anesthesia with MAC compared to previous studies [239].
Local anesthesia with MAC allows patients to avoid the undesirable side effects and risks of general anesthesia. In this report, a 37-year-old female patient with myasthenia gravis safely underwent a planned thyroid lobectomy under local anesthesia with MAC, and was discharged without any discomfort or perioperative complications 1 day after the surgery. The neurologist recommended local anesthesia or preparing for mechanical ventilation after general anesthesia during a preoperative work-up because of the possibility of delayed recovery from the effects of muscle relaxants. Other reports have demonstrated that patients with a family history of malignant hyperthermia or toxic amiodarone-induced hyperthyroidism have safely received thyroid surgery under local anesthesia [1011]. In addition, intraoperative voice monitoring is possible in patients receiving local anesthesia with MAC, which may make it preferable for patients with professional voice demands such as singers, vocal trainers, or teachers.
The need for local anesthesia combined with MAC is rising with development of minimally invasive techniques in the field of thyroid surgery, particularly in outpatient settings. However, candidates for thyroid surgery under local/regional anesthesia with MAC must be chosen carefully. In a previous review, some absolute and relative contraindications were suggested to help with local/regional anesthesia for thyroidectomy [12]. In their criteria, a communication barrier, a technically challenging operative procedure, patient refusal, and allergy to local anesthetic drugs were considered as absolute contraindications for local/regional anesthesia. Morbid obesity, sleep apnea, obscure anatomy, anticipated difficult intubation, prior neck surgery, and limited neck extension were relative contraindications; however, these patients can be candidates for local anesthesia with MAC on a case-by-case basis. Although we followed these classic criteria, selection criteria can be broadened over the course of increasing experience of the surgeon and anesthesiologist. Spanknebel et al. [9] reported cases over 16 years and included patients with substernal goiter, extensive cancer, and morbid obesity in the last 5 years.
In addition, any possible intraoperative events beyond adjusting the sedation level should be known. Not only pain, but a vague awareness of being in the operation theater, sense of pulling and pressure on the surgical field, and fear of a blinding field of vision with surgical drapes can be irritating to patients. On the other hand, the surgeon must contend with occasional motion of the operative field due to movements by the patient such as swallowing, coughing, or respiratory motion under local anesthesia with MAC. Conversion to general anesthesia is occasionally required due to unanticipated lymphadenectomy, nerve sacrifice or injury, a change in the operative plan due to local invasion of a tumor, patient discomfort/anxiety, or long duration of the procedure. Having a prior consultation or conversation among the surgeon, patient and anesthesiologist might help the surgeon can be accustomed to those intraoperative incidents of sudden motion, the patient can understand and endure the minor discomfort, and the anesthesiologists can prepare the rapidly changing condition of operative field or patients.
This report is a preliminary study on a new anesthetic approach for thyroidectomy. However, we could not fully demonstrate whether local anesthesia with MAC for thyroidectomy is superior to general anesthesia. Our case report neither had a sufficient number of subjects to make a definitive recommendation on this topic nor had a control group, but rather shows the possibility of this new anesthetic approach for thyroid surgery. The positive experiences from this case report offer pilot data or a clinical protocol for further investigation of thyroidectomy under local anesthesia with MAC. In conclusion, thyroid surgery in selected patients can be performed safely using local anesthesia with MAC by experienced surgeons and anesthesiologists and may be a simple and reasonable alternative to general anesthesia.
Notes
Eugene Kim is now with the Department of Anesthesiology and Pain Medicine, Catholic University Hospital of Daegu, School of Medicine, Catholic University of Daegu, Daegu, Korea.