A suspected malignant hyperthermia managed without dantrolene sodium
Article information
Malignant hyperthermia (MH) is a hypermetabolic reaction that develops in individuals with sensitivity to inhalation anesthetics or depolarizing muscle relaxants [1]. The clinical manifestations of MH are characterized by muscle rigidity, hypercapnia, tachycardia, myoglobinuria, acidosis, rhabdomyolysis, and hyperthermia [1]. We herein report a suspected case of MH that manifested during general anesthesia.
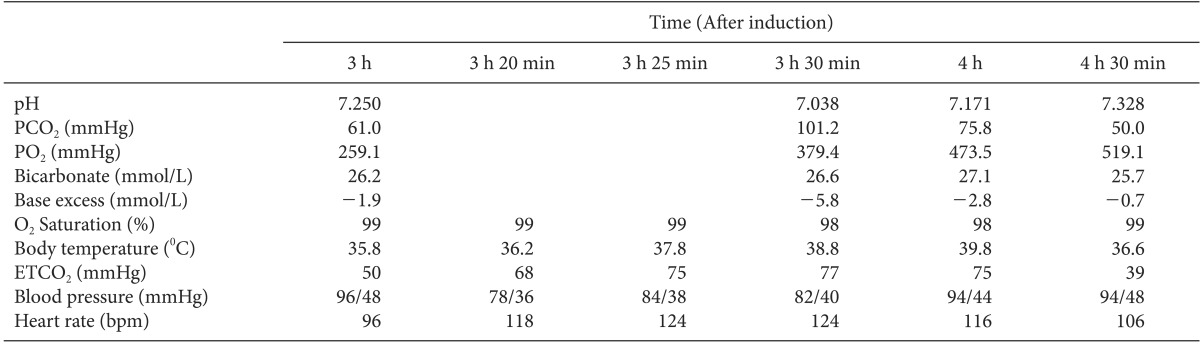
A 61-year-old man was scheduled to undergo left lateral temporal bone resection, parotidectomy, and supraomohyoid neck dissection. He had no history of surgery. Preoperative laboratory, chest radiographic and electrocardiographic findings were normal. Upon arrival in the operating room, standard monitoring was applied. The baseline blood pressure (BP) and heart rate (HR) were 129/71 mmHg and 85 bpm, respectively. Anesthesia was induced with propofol and remifentanil. After tracheal intubation, anesthesia was maintained with sevoflurane, oxygen, and medical air. About 3 h after induction, the end-tidal carbon dioxide (ETCO2) gradually increased to 50 mmHg. At that time, the patient's esophageal temperature was 35.8℃, and arterial blood gas analysis (ABGA) revealed a pH of 7.250, PCO2 of 61.0 mmHg (Table 1). First, we checked for bending or blockage of the breathing circuit. We found no signs of tracheal tube obstruction. The patient's respiratory rate and tidal volume were increased in an effort to decrease the ETCO2. However, the ETCO2 gradually increased and eventually maximized at 75 mmHg. At 3 h 30 min after induction, hypotension and tachycardia developed, and the ETCO2 was still high (77 mmHg). At this time, the patient's esophageal temperature abruptly increased to 38.8 from 36.2℃ 10 min previously. ABGA showed a pH of 7.038, PCO2 of 101.2 mmHg (Table 1). Within 5 min, the esophageal temperature reached 39.0℃, and the tympanic membrane temperature was 39.2℃. MH was suspected, and we promptly initiated the recommended therapy for MH. Sevoflurane administration was immediately discontinued, and the patient was hyperventilated with 100% oxygen (>10 L/min) through a non-rebreathing circuit. The anesthesia machine was quickly replaced with a machine that had not been exposed to inhalation anesthetic agents. Anesthetic maintenance was changed to a continuous infusion of propofol, and all means of lowering the temperature were used. Because dantrolene sodium was not available in our hospital, we called two medical centers that possessed this drug to deliver it to us as quickly as possible. The heating devices and heated circuit were removed. A Levin tube was inserted for cold saline irrigation. The axillary area was filled with ice packs, and the abdomen, both lower extremities and groin were massaged with ice water. Esmolol (20 mg) was administered to control the HR. During the treatment, the highest ETCO2 was 102 mmHg, and the highest BT was 39.9℃. Thirty minutes after the first detection of hyperthermia (at 4 h after induction), the patient's body temperature reached 39.8℃. The arterial pH increased from 7.038 to 7.171, and the PCO2 decreased from 101.2 to 75.8 mmHg (Table 1). A complete blood cell count, coagulation profile, cardiac enzyme analysis, creatine kinase level, and urinalysis (including urine myoglobin) were then ordered. Laboratory findings were normal with the exception of an elevated serum myoglobin level. During the next 30 min, the ETCO2 decreased to 39 mmHg, and the patient's condition gradually stabilized (Table 1). The operation then resumed, and all vital signs remained within the reference range. The dantrolene sodium arrived at this point, but the patient's acute symptoms had improved. We decided not to use dantrolene sodium. No additional episodes were observed until the end of the operation. The patient was transferred to the intensive care unit to monitor any possible postoperative relapse of MH. On postoperative day 1, the patient was moved to the general ward. The patient was discharged 10 days postoperatively without specific complications.
In this patient, the presenting symptoms were an increase in the ETCO2 and tachycardia, both of which are nonspecific for MH. We found no cause of the hypercapnia or tachycardia after exploring various possible causes. The increase in body temperature followed shortly thereafter. This helped us to diagnose MH. It is well known that an abrupt increase in body temperature can be an important sign of MH [2]. However, it is a relatively late sign. Therefore, unexplained elevation in the ETCO2 can be a sensitive and the earliest symptom of MH [2]. Baudendistel et al. [3] reported two cases of MH in which the earliest sign was a rise in the ETCO2. They found that close monitoring of ETCO2 helped to achieve rapid diagnosis and treatment [3]. In our patient, despite the gradual adjustment of the minute ventilation, the ETCO2 eventually increased to an uncontrollable level. At that time, we associated the elevation of ETCO2 with the abnormalities in other vital signs such as the body temperature and heart rate. We suspected MH based on the unexplained increase in the ETCO2 and the presence of tachycardia and hyperthermia.
In our patient, the onset of MH was late (3 h after exposure to sevoflurane). There are agent-specific relationships between inhalational agents and the onset time of MH [4]. The time interval between induction of anesthesia and the development of clinical manifestations of MH may suggest the relative potency of the inhalation anesthetics triggering MH [4]. Hopkins [4] reported that the onset of the MH reaction to halothane is faster than that to enflurane and sevoflurane.
Dantrolene sodium is the treatment of choice for termination of MH. In the current case, however, we did not administer this agent. According to a report by Larach [5] on MH that developed in patients in North America from 1987 to 2006, 22 of the total 286 patients recovered without dantrolene sodium. This implies that MH can be treated with symptomatic therapy only, as in the present case.
In conclusion, MH can occur slowly after exposure to sevoflurane with nonspecific symptoms such as hypercapnia and tachycardia and can progress to overt hyperthermia in a short period of time. Early recognition of MH and subsequent symptomatic treatment is important in that the patient can recover even without the use of dantrolene sodium.