Evaluation of the ability of continuous palonosetron infusion, using a patient-controlled analgesia device, to reduce postoperative nausea and vomiting
Article information
Abstract
Background
The efficacy of palonosetron in preventing postoperative nausea and vomiting (PONV), as well as chemotherapy-induced nausea and vomiting, has already been demonstrated in multiple clinical studies. The purpose of this study was to determine whether continuous infusion of palonosetron following single injection could reduce PONV to a greater extent than single injection only of palonosetron.
Methods
In total, 132 women were enrolled in the study. All subjects were over the age of 20 years and were scheduled to undergo gynecologic laparoscopic surgery. Patients were randomly allocated into two groups. In both groups, patients received 0.075 mg of palonosetron intravenously, immediately before induction of anesthesia. In the continuous palonosetron infusion group, 0.075 mg (1.5 ml) of palonosetron was added to the patient-controlled analgesia device. In the single-injection palonosetron group, 1.5 ml of normal saline was added.
Results
The incidence of PONV 24 hours postoperatively was significantly lower in the continuous palonosetron infusion group than the single-injection palonosetron group (31.8 vs. 56.1%, P = 0.009).
Conclusions
Continuous palonosetron infusion, following single injection, reduces the incidence of PONV compared with single injection only.
Introduction
Postoperative nausea and vomiting (PONV) is a common and distressful complication following anesthesia and surgery. Although PONV is usually a mild and self-limiting condition, serious PONV-related complications such as pulmonary aspiration pneumonia, wound dehiscence, esophageal bleeding, and even vision loss have been reported [1]. Therefore, PONV is an important concern to anesthesia providers, and different drugs and modalities are being investigated as possible treatments.
5-hydroxytryptamine type 3 (5-HT3) receptor antagonists comprise a major group of drugs frequently used to prevent PONV. Palonosetron is the most recently developed 5-HT3 receptor antagonist, and has a greater efficacy and a longer elimination half-life than previously studied 5-HT3 receptor antagonists [2]. The efficacy of palonosetron in preventing PONV, as well as chemotherapy-induced nausea and vomiting (CINV), has been demonstrated in several clinical studies [3,4]. Recently, Laha et al. [5] showed that palonosetron was comparable to ondansetron for PONV prophylaxis in laparoscopic cholecystectomy, and in another prospective, randomized, double-blinded study, palonosetron had superior antiemetic efficacy to ondansetron or ramosetron in high-risk patients undergoing laparoscopic surgery [6]. In addition, for high-risk patients receiving fenatnyl-based patient-controlled analgesia (PCA) after thyroidectomy, palonosetron was shown to be more effective than ondansetron [7].
The purpose of our study was to determine whether continuous infusion of palonosetron following single injection reduced PONV to a greater extent than single injection alone of palonosetron, and if so, the extent to which the palonosetron infusion was effective. In this study, continuous infusion was provided using a PCA device.
Materials and Methods
Prior study approval was obtained from the Institutional Review Board of our hospital under protocol #OC11MISI0109, and all enrolled patients provided written informed consent. The study protocol was also registered with clinicaltrials.gov. In total, 132 women were enrolled in the study. All subjects were over the age of 20 years and were scheduled to undergo gynecologic laparoscopic surgery. No patient received emetic or antiemetic medication or therapy prior to initiation of the study, and all patients were classified as American Society of Anesthesiologists Physical Status 1 or 2.
Patients were allocated randomly into two groups. In both groups, patients received 0.075 mg of palonosetron intravenously, immediately before induction of anesthesia. Anesthesia was induced with 2 mg/kg propofol and maintained with 1-4% sevoflurane in an oxygen-air mixture (FiO2 = 0.5). Tracheal intubation was facilitated with 0.6 mg/kg rocuronium, and additional rocuronium was administered as needed. End-tidal CO2 was kept at 30-35 mmHg throughout the surgery, and no opioid was used before providing PCA.
Approximately 30 min before the end of the surgery, PCA devices were provided. These devices were prepared to deliver 10 µg/h background infusion of fentanyl with a 10 µg bolus, with a lock-out time of 15 min. In the continuous palonosetron infusion group (group C), 0.075 mg (1.5 ml) of palonosetron was added to the PCA device. In the single-injection palonosetron group (group S), 1.5 ml of normal saline was added. At the end of surgery, patients received pyridostigmine 0.2 mg/kg and glycopyrrolate 0.008 mg/kg for reversal of neuromuscular blockade. For postoperative pain control, ketorolac 30 mg was allowed when the verbal rating scale (VRS) score ranging from 0 (no pain) to 10 (worst pain imaginable) exceeded 5 and the patient requested treatment.
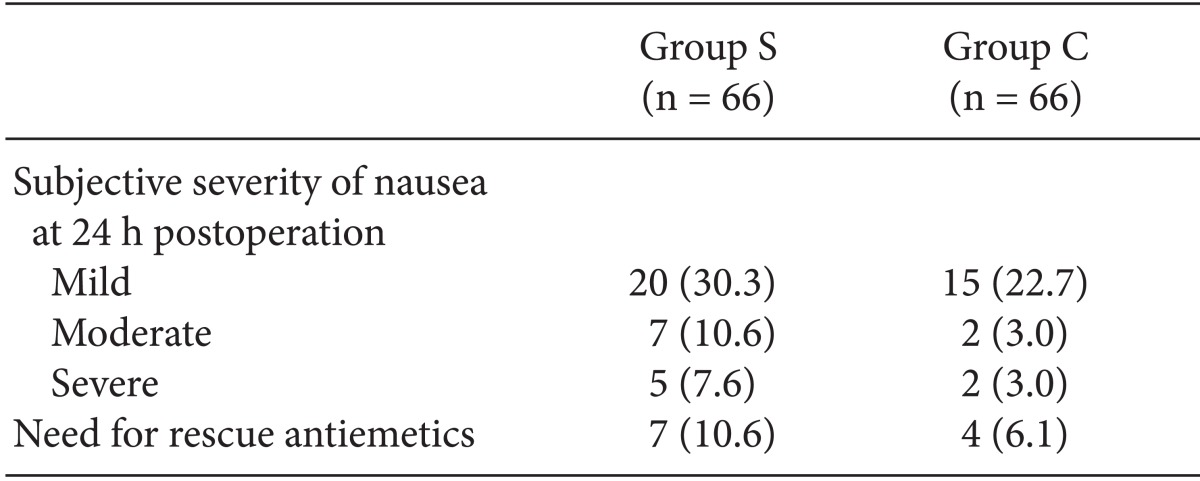
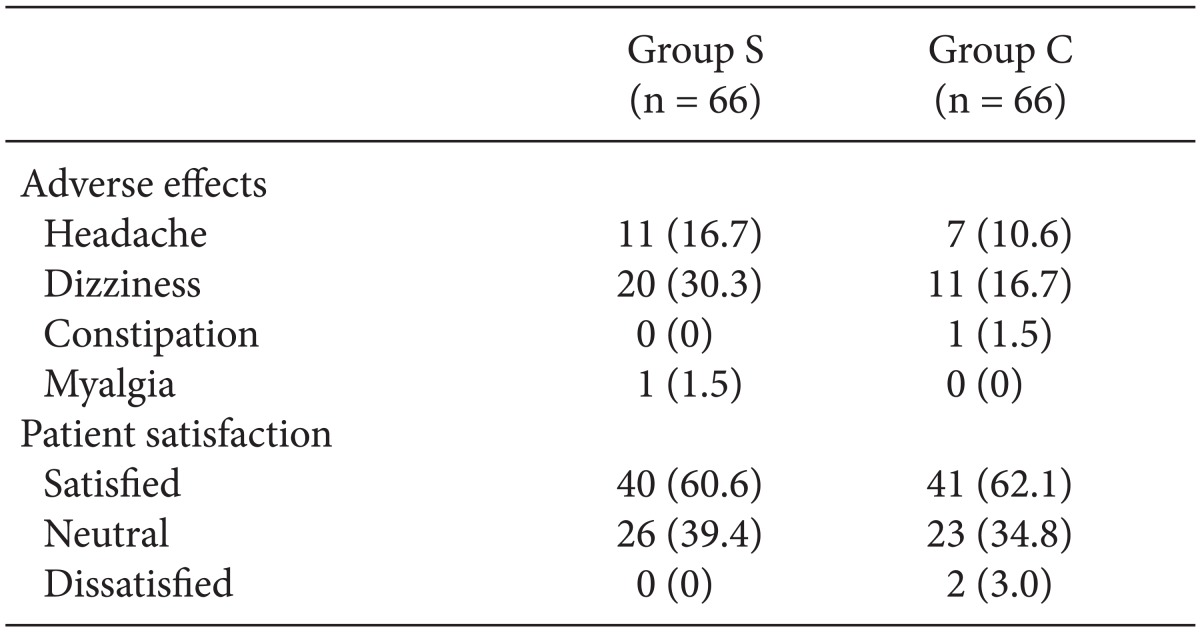
Doctors who were not involved in the study monitored and interviewed enrolled patients. Incidences of nausea and vomiting were assessed during the following postoperative time intervals: 0-2, 2-6, and 6-24 h. Patients were also asked to rate their subjective severities of nausea at 24 h postoperation. Severity was rated on a 3-point scale (mild, moderate, or severe). Rescue antiemetic use and adverse effects, including headache, dizziness, constipation, and myalgia, were also assessed, and at 24 h postoperation, patients were asked to rate their satisfaction on a 3-point scale (satisfied, neutral, or dissatisfied). As a rescue medication for PONV, metoclopramide 10 mg was permitted intravenously at the patient's request when more than moderate nausea or vomiting occurred.
Sample size was designed to show a 50% (ranging from 50 to 25%) difference in the incidence of PONV, allowing an alpha error of 5% and a beta error of 20% [8,9,10]. Student's t-test and the Mann-Whitney rank sum test were used to compare continuous variables, while the χ2 and Fisher's exact test were used for categorical variables. A difference was regarded as statistically significant when P < 0.05. All statistical analyses were performed using the SPSS® statistical package, version 19.0 (SPSS Inc., Chicago, IL, USA) for Windows®.
Results
No differences in any clinical characteristics or operative data were observed between the two groups (Table 1). Incidence of PONV 24 hours postoperation was significantly lower in group C than group S (31.8 vs. 56.1%, P = 0.009) (Fig. 1). Patients in group S experienced significantly more nausea for 24 hours postoperation than patients in group C (54.5% vs. 31.8%, P = 0.014) (Fig. 1). However, this trend was not observed for vomiting. No statistically significant differences were found in the severity of nausea, rescue antiemetic use, incidence of adverse effects, or patient satisfaction between the two groups (Tables 2 and 3).
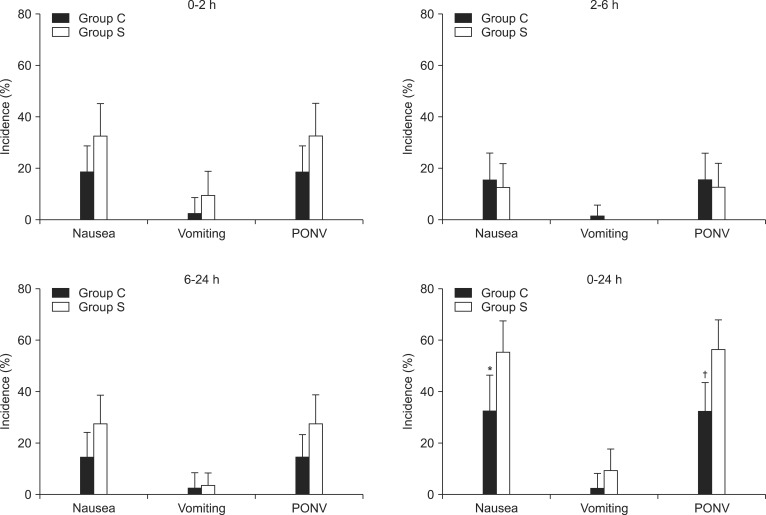
Incidence (%) of postoperative nausea and vomiting (PONV). *Patients in group S experienced significantly more nausea 24 hours postoperation than patients in group C (54.5 vs. 31.8%, P = 0.014). †The incidence of PONV for 24 hours postoperation was lower in group C than group S (31.8 vs. 56.1%, P = 0.009). Error bar indicates the value of the upper limit of the 95% confidence interval for the percentage of patients.
Discussion
Palonosetron is a recently developed 5-HT3 receptor antagonist. It has a high affinity for the 5-HT3 receptor, with a pKi of 10.4 (100 times that of ondansetron), and has an extremely long elimination half-life of about 40 h [11]. Several studies have revealed its improved efficacy in preventing PONV compared with previously developed 5-HT3 receptor antagonists [12,13]. Although previous studies have also supported the merits of palonosetron as an option for preventing PONV, the incidence of PONV remains high in patients with multiple risk factors [4,9].
To prevent PONV, palonosetron has typically been administered at a dose of 0.075 mg. However, palonosetron is known to be safe at even higher doses [14,15]. Furthermore, Y-site administration of palonosetron has been reported to be compatible and stable with fentanyl [16]. On the basis of these reports, we designed the present study to test whether the incidence of PONV could be lowered by continuous infusion of palonosetron using a PCA device, accompanied by a single injection of palonosetron.
Choi et al. [8] reported that PCA-administered continuous infusion of ramosetron, combined with a single injection of ramosetron, significantly decreased the incidence of PONV. Ondansetron was also reported to be effective when administered continuously via a PCA [17].
In the present study, the incidence of PONV was significantly lower 24 hours postoperation in the continuous infusion group than the single injection-only group (31.8 vs. 56.1%, P = 0.009) (Fig. 1).
The elimination half-life of palonosetron is 40 h, and it has been debated whether prolonged inhibition of 5-HT3 receptors by palonosetron is associated with allosteric binding or receptor internalization. In a recent report, palonosetron treatment was shown to down-regulate the amount of available 5-HT3 receptor binding sites, rather than cell surface expression levels of 5-HT3 receptors [18]. This result suggests that palonosetron inhibits 5-HT3 receptors by interacting with an allosteric binding site rather than by inducing receptor internalization.
In the case of another 5-HT3 receptor antagonist, ramosetron, it was proposed that higher receptor occupancy indicated more extensive antiemetic action [19], and it was hypothesized that continuous infusion of the drug following single injection would maintain higher receptor occupancy [8]. Palonosetron exhibits significant receptor occupation for as long as 4 days [18]. Given this characteristic of palonosetron, we investigated the effects of continuous infusion in the context of a PCA on the incidence of PONV in high-risk patients. We observed that the incidence of PONV decreased with supplemental continuous infusion of palonosetron following a single injection of palonosetron, and we assumed that similar to the case of ramosetron, continuous infusion of palonosetron using a PCA increased the plasma concentration of palonosetron, thereby improving receptor occupancy and antiemetic action.
Compared with the 0-2 h (18.2 vs. 31.8%, P = 0.108) and 2-6 h (15.2 vs. 12.1%, P = 0.800) time intervals, the difference in PONV incidence between the continuous infusion group and the single injection group was marginally significant at the 6-24 h time interval (13.6 vs. 27.3%, P = 0.084) (Fig. 1). This result suggests that additional continuous infusion could potentially prevent PONV during the late postoperative period (6-24 h). A similar difference was observed at the 0-2 h time interval, although this difference was also not statistically significant. It is interesting that the amount of additionally administered palonosetron during the period was quite small. However, little is known about the relationship between the pharmacokinetic profile of palonosetron and its clinical effects. Furthermore, the etiology of PONV is complex and multi-factorial, and additional factors such as patient transportation and volume status during the 0-2 h time interval, as well as diet and ambulation during the late postoperative period, may contribute to the incidence of PONV. Although the amount of palonosetron added to the PCA device was small, it appeared to be helpful in controlling PONV during these periods.
In this study, continuous infusion of palonosetron in addition to single injection resulted in a similar incidence of side-effects compared to single injection only, indicating a similar safety profile. Two vials of palonosetron (0.075 mg each) were used in the continuous infusion group; further studies are warranted to determine the optimum rate of continuous palonosetron infusion and to evaluate its cost effectiveness in high-risk patients and clinical situations in which PONV is extremely harmful. In the present study, all enrolled patients were women, and most exhibited three or more risk factors as determined by their simplified Apfel's scores [20]. The cost effectiveness of palonosetron for treating CINV has already been evaluated and was shown to be favorable [21].
In conclusion, we demonstrated that continuous palonosetron infusion, following single injection, reduced the incidence of PONV compared with single injection only.